Contents
What is pericarditis
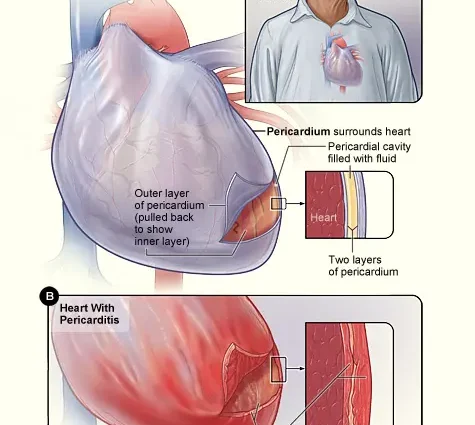
Pericarditis is an inflammation of the pericardium, the thin, two-layer sac that surrounds the heart. There is a small amount of liquid between the layers to prevent friction when beating. When the layers become inflamed, this can lead to disruption of the full functioning of the heart, the formation of adhesions in the cavity, the accumulation of fluid and pain in the chest. The pericardium also helps keep the heart inside the chest.
Pericarditis usually comes on suddenly and lasts from a few days to a few weeks.
Anyone can get pericarditis. In most cases, it goes away on its own. However, 15 to 30% of people get sick more than once—this is called recurrent pericarditis.
There are several forms of pericarditis:
- acute – it can occur on its own or as a symptom of an underlying disease;
- recurrent – may be intermittent or permanent, the first recurrence usually occurs within 18 to 20 months from the initial illness;
- chronic – in this case, a relapse occurs immediately after treatment;
- delayed (Dressler’s syndrome) – it develops a few weeks after heart surgery or a heart attack;
- constrictive – the pericardium becomes scarred or sticks to the heart, so the heart muscle cannot expand (this form is rare and can develop in people with chronic pericarditis or after heart surgery);
- effusion-constrictive pericarditis – in this case, effusion (fluid) accumulates in the pericardium and the heart narrows.
A third of people with pericardial effusion develop cardiac tamponade, which is a medical emergency.
Causes of pericarditis in adults
The cause of most pericarditis is unknown, but it is believed that 80 to 90% of cases are associated with infections (viruses, bacteria, fungi, and parasites).
In addition, the cause of pericarditis can be:
- cardiovascular problems (previous heart attack or surgery);
- trauma;
- radiation therapy;
- autoimmune diseases such as lupus;
- some medicines, which is rare;
- metabolic disorders such as gout;
- kidney failure;
- certain genetic diseases, such as familial Mediterranean fever;
- cancer;
- some medicines.
Symptoms of pericarditis in adults
Pericarditis may feel like a heart attack with sudden sharp or stabbing pain in the chest. The pain may be in the middle or left side of the chest, behind the breastbone, and may spread to the shoulders, neck, arms, or jaw.
Other symptoms may include:
- temperature;
- dry cough;
- weakness or fatigue;
- difficulty breathing, especially when lying down;
- cardiopalmus;
- swelling of the feet, legs and ankles.
The resulting symptoms may worsen if the patient lies down, takes a deep breath, coughs, eats or drinks. But if he sits down, leaning forward, it gets better.
If a bacterial infection is the cause of pericarditis, the patient may have a fever, chills, and a higher than normal white blood cell count. If the cause is viral, there may be flu-like symptoms or indigestion.
In any case, if there is chest pain (it happens in 85 – 90% of cases), you should immediately call an ambulance.
Treatment of pericarditis in adults
First of all, the doctor will find out the medical history, ask about the symptoms, when they appeared, and what aggravates them. Then he listens to the heart with a stethoscope – if fluid has accumulated, friction of the pericardium against the outer layer of the heart will be heard.
Diagnostics
Other tests used for diagnosis include:
- chest x-ray, which shows the shape of the heart and possible excess fluid
- an electrocardiogram (ECG) to check the heart rhythm and see if the voltage signal is reduced due to excess fluid
- an echocardiogram, which will also show the shape, size of the heart, and fluid accumulation
- MRI;
- computed tomography, which gives a detailed image of the heart and pericardium;
- right heart catheterization, which will provide information about the pressure in the heart;
- blood tests to look for markers of inflammation indicative of pericarditis.
Modern treatments
Treatment for pericarditis will depend on its underlying cause. If it is a bacterial infection, antibiotics may be prescribed. In most cases, according to the American Heart Association, pericarditis is mild and resolves on its own with just rest. But the doctor may prescribe non-steroidal anti-inflammatory drugs (Ibuprofen, Aspirin).
If there are other medical risks, the patient may be hospitalized. In this case, therapy will be aimed at reducing pain, inflammation and minimizing the risk of relapse. As a rule, colchicine is prescribed in this case.
Corticosteroids are also effective in reducing the symptoms of pericarditis, however, studies have shown that early use of these drugs may have an increased risk of disease recurrence and should be avoided except in extreme cases where the disease does not respond to conventional treatment.
Surgery may be considered for recurrent pericarditis that does not respond to other treatments, in which case the pericardium is removed.
Prevention of pericarditis in adults at home
It is difficult to prevent pericarditis, but in case of illness, it is important to strictly follow the treatment plan prescribed by the doctor. Until complete recovery, rest more, avoid heavy physical exertion.
If you notice any signs of a relapse, see your doctor as soon as possible.
Recovery from pericarditis takes time. In some cases, the complete disappearance of symptoms may take several weeks.
Popular questions and answers
We asked questions about pericarditis to answer cardiologist Stanislav Snikhovsky.
● thickening or adhesion of pericardial sheets (external and internal), which leads to difficulty in the work of the heart and the development of heart failure;
● cardiac tamponade (accumulation of a large amount of fluid between the sheets of the pericardium), which also leads to difficulty in the work of the heart, the development of heart failure and possible cardiac arrest;
● formation of fistulas (holes) of the internal mammary artery – this is possible only with purulent pericarditis and is a rare complication;
After suffering pericarditis, cardiac conduction disturbances can be observed for a long time. They are manifested by periodic attacks of arrhythmia (especially during exercise).
Most often, patients complain of shortness of breath (at rest or with little physical exertion), pain in the heart, palpitations, general weakness.
Folk remedies in the treatment of pericarditis are used as an additional therapy and only in the treatment of dry (fibrinous) pericarditis. Among them:
● decoction of young needles;
● collection of hawthorn, calendula, linden flowers and dill;
● infusion of birch catkins;
● collection of valerian root, yarrow and lemon balm leaves.