Contents
- Palliative medicine – what should you know about it?
- The beginnings of palliative medicine
- What is symptomatic treatment in palliative medicine?
- Palliative medicine and its place in oncology
- Which patients can be covered by palliative and hospice care?
- Palliative medicine and the patient’s family
- What are the benefits of palliative care?
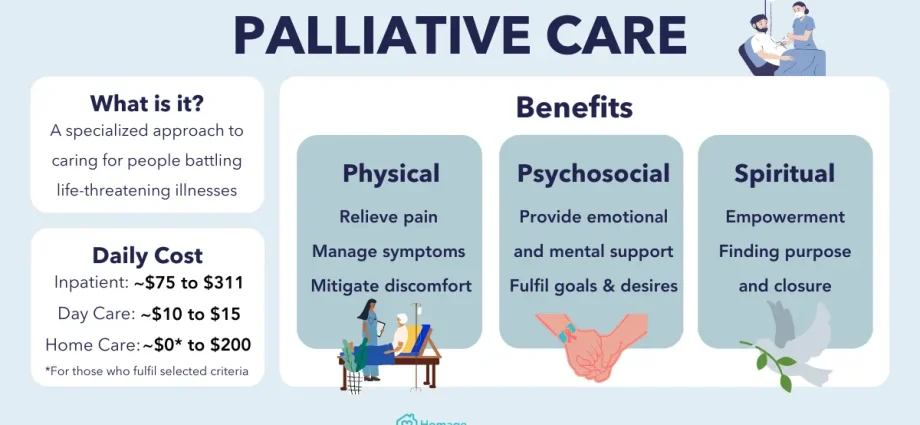
Palliative medicine is otherwise simply called palliative care. The name comes from the English word palliative, meaning “soothing”, “relieving”. According to the definition of the World Health Organization (WHO), palliative medicine is an activity that improves the quality of life of patients and their families when problems related to a life-threatening disease arise.
Palliative medicine – what should you know about it?
It is a branch of medicine dealing with the treatment and care of terminally ill people, which can also be defined as a philosophy. Contrary to appearances, the aim of her actions is not to cure the sick, but to improve the quality of his life. These activities focus on alleviating the symptoms of the disease, reducing or completely reducing pain and supporting the patient and his relatives both mentally and spiritually.
- Check what holistic medicine is all about
The palliative medicine team includes doctors, nurses and trained volunteers. However, an important role is played by nurses who accompany the sick every day. The doctor, in turn, determines what the patient’s needs are and what therapy to use. Sometimes the team is also joined by psychiatrists and physiotherapists, but also people not related to medicine, e.g. a social worker, psychologist or a clergyman.
The beginnings of palliative medicine
Cicely Sanuders, a British doctor who opened St. Krzysztof in London. The center quickly became a place where doctors and carers were trained. What distinguished him from other hospitals and care centers was a new approach to symptomatic treatment and individualized patient care. The hospice staff proved that the doctor has a significant influence on the patient’s fate, regardless of the type of disease.
Apart from C. Saunders, Elisabeth Kuebler-Ross, an American physician of Swiss origin, also contributed to the development of palliative medicine. E. Kuebler-Ross had many valuable observations regarding mental reactions and adaptation to the daily functioning of terminally ill patients. Hospices, such as in the United Kingdom, then begin to emerge in Canada, Australia, the Netherlands, Japan and the USA as well.
- Find out more about mental illness
Palliative medicine in Poland began to develop in the 80s – at that time such centers were known as the “hospice”. In the 90s of the twentieth century there was a dynamic development of this field and now there are about 200 units dealing with palliative medicine. Moreover, access to this type of treatment is confirmed by the UN convention – access to palliative medicine is a human right.
Inpatient care has been included in the national health care system since the early 90s. In 1999, a medical and nursing specialization in palliative medicine was established. Earlier, there was also the “Program for the development of palliative and hospice care in Poland”, functioning at the Ministry of Health. Palliative Medicine is also considered as part of oncology and is financed from public funds.
What is symptomatic treatment in palliative medicine?
One of the main tasks of palliative medicine is to relieve the symptoms of the disease. For example, an advanced cancer disease causes many symptoms that make it impossible for the patient to function – often it is both physical and mental suffering. Moreover, these sufferings are felt not only by the patient, but also by his relatives, for whom the mere sight of a sick person causes psychological discomfort and suffering.
The success of symptomatic treatment depends on the diagnosis – the elements of the diagnosis include: analysis of the pathomechanism and response to a given treatment method. Thanks to the analysis of the pathomechanism, it is possible to target the treatment and limit the development of the inflammatory response and reduce the emotional response. The palliative medicine treatment plan takes into account not only the clinical picture of the disease, but also the influence of factors such as the patient’s self-esteem in both physical and social matters, and how close to death is.
Contrary to traditional medicine, specialists in palliative medicine attach importance to the patient’s self-esteem. Many patients judge themselves through the prism of what the doctor tells them – it is the doctor who is often the patient’s highest authority. As a result, palliative medicine specialists care about how they communicate information to patients, what terms they use and what gestures they make.
Palliative medicine and its place in oncology
It is recognized that palliative care in oncology should be considered as an additional aid. ESMO (European Society for Medical Oncology) defines palliative care as supportive treatment aimed at improving the patient’s quality of life, his functioning in the family and community. It also recognizes that palliative care should relate to the stage when the person is terminally ill.
Which patients can be covered by palliative and hospice care?
Palliative care centers admit people with life-limiting diseases, people with advanced cancers and other chronically progressive conditions that reduce their quality of life. Whether the patient is admitted to the center depends on both somatic, psychosocial and spiritual criteria. The person deciding whether a given patient should be admitted or not is the physician of the palliative or hospice care center.
In 2005, the American Palliative and Hospice Association determined that the indications for such care include the following conditions:
- advanced neoplastic disease,
- neoplastic disease with hematological diseases that cannot be treated causally,
- neuromuscular disease (primarily amyotrophic lateral sclerosis),
- dementia,
- Alzheimer’s disease,
- chronic heart failure in stage III and IV,
- lung diseases with advanced respiratory failure,
- circulatory failure,
- chronic lung disease
- stroke,
- the presence of chronic and difficult-to-heal wounds,
- chronic lymphedema,
- chronic pain accompanying e.g. osteoporosis, chronic rheumatic disease,
- inflammation of the pancreas (chronic and not responding to treatment),
- neuropathic pain
- inoperable aortic aneurysm.
Palliative medicine and the patient’s family
Palliative medicine specialists show the same interest in both patients and their relatives. The illness of one family member often has a devastating effect on his relatives and the people who love him. The lack of treatment effects, side effects of treatment and other unpleasant symptoms make the suffering of the patient’s relatives deepen. The reason for problems in the patient’s family is also the inability to cooperate.
Family support is also needed because of the burden that is imposed on them by caring for a sick person alone. As a result, its members have more responsibilities, which are often a considerable physical burden for them. In addition, it causes psychological problems, e.g. anxiety about the patient’s mental state, fear that it is not possible to give him hope, reassurance or fear that the patient will be given the right dose of the drug.
The family of a person requiring such advanced care often has many internal blockages, e.g. before hygienic procedures, changing dressings with unpleasant odors. Often, for these and other reasons, relatives of the patient begin to suffer from depression, have sleep disorders, problems with concentration, and even begin to drink more alcohol or take drugs. All this has an impact on the patient’s well-being, which is why his relatives are also covered by palliative care.
Medical personnel specializing in palliative medicine have different methods of working with patients and their families. He also shows an interest in the mental suffering of his relatives, talks with them about what they are going through and what actions they take in relation to caring for the patient. Monitoring somatic symptoms and spiritual-existential problems is a great help.
What are the benefits of palliative care?
Palliative and hospice treatment are standard methods of treatment in modern medicine and constitute an important element of the entire treatment and oncological care. It is believed that they should also be standard treatments for patients with other life-limiting diseases. Palliative care, enriched with rehabilitation and creative therapy, may limit the development of the disease, although it will not cure it.
Palliative care has a unique impact on the health of the patient and extends his life. Moreover, it brings significant improvements in physical and mental health, alleviates symptoms of severe illnesses and protects against complications. Due to the fact that it soothes ailments, it enables further oncological therapies. As a result, the patient also functions better in the family and can carry out life plans – this also translates into a better well-being of his relatives.
Due to the fact that the interdisciplinary specialist team includes not only a doctor, nurse, but also a psychologist, physiotherapist, occupational therapist and a clergyman, the sick person can stay at home with their relatives and not give up the home for the benefit of the hospital – this solution is often for it is more convenient and comfortable.
Medical care is provided free of charge, also at weekends. The patient also receives the necessary equipment, such as a hospital bed, anti-bedsore mattress, an infusion pump for subcutaneous administration of drugs, and an oxygen concentrator. The patient is also constantly monitored by qualified nurses, who constantly cooperate with the doctor – frequent visits by nurses also promote good communication between the patient and the family.
A sick person can also stay in a specialist palliative and hospice care unit. However, only patients who cannot be treated at home can go there. These centers are also reserved for single people who are at the end of their lives and for those who need to take part in additional examinations and specialist consultations.