Contents
What is hip osteoarthritis?
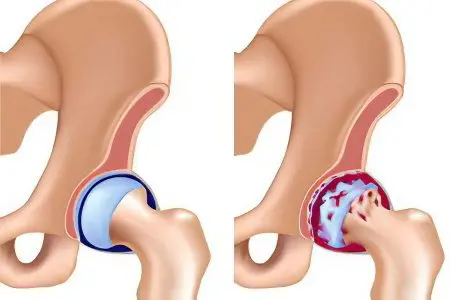
Osteoarthritis of the hip joint is a very complex disease in which the destruction of the hyaline cartilage that lines the surface of the femoral head (has a spherical shape) and the acetabulum occurs. Arthrosis is a degenerative-dystrophic disease that most often develops in the elderly.
In specialized periodicals, the results of ongoing surveys and medical studies are often published, according to which the female half of the population, who has reached the age of 40, is most susceptible to arthrosis of the hip joint. This is primarily due to the anatomical features of the female hip joint, which has a different shape and position than in men. Such differences can be explained by the fact that the hip joint plays an important role in the process of childbearing. The bones of the female pelvis experience a strong daily load, as a result of which they are more prone to various diseases. Males at a later age (by the age of 60) may experience arthrosis.
According to available statistics, patients who underwent surgical treatment of arthrosis of the hip joint may develop various complications:
blood loss during surgery;
thromboembolism (pulmonary artery) – 0,05% of cases;
development of infection (after surgery) – 0,5% -2% of cases.

Most often, in this category of patients, infection occurs in the area of the endoprosthesis that performs the functions of the joint. In this case, doctors perform a second operation, during which the endoprosthesis is removed, and after that a course of antibiotics is prescribed.
At the time of thrombosis, the patient has a blockage of the pulmonary artery. This type of complication is often fatal, especially for those patients who have a predisposition to the formation of blood clots. To prevent such a complication after surgery, patients are given special drugs that reduce blood viscosity.
Severe bleeding during surgery is a common complication of surgical treatment of arthrosis of the hip joint. In modern medical centers there is a large supply of blood and its substitutes, thanks to which specialists can easily cope with this complication.
Causes of arthrosis of the hip joint
Modern medicine divides this disease into the following categories:
Primary arthrosis develops for no apparent reason.
Secondary arthrosis develops against the background of previous injuries of the hip joint.
To date, the following causes of the development of arthrosis of the hip joint have been identified:
depression, as well as prolonged exposure to stress;
excess weight (even a slight set of excess weight can cause the development of this disease, since additional stress will be placed on the joints);
previous injuries: sprains, bruises, blows, fractures, etc.;
inflammatory processes;
damage to cartilage in the joint;
diseases of the endocrine system (in particular diabetes mellitus) that have a negative impact on the functioning of the adrenal glands;
poor heredity, against which a joint deformity can develop (genetic predisposition to arthrosis is the most common cause of this disease);
displacement or curvature of the femur;
hip dysplasia (most often diagnosed in newborns);
protrusion of the acetabulum;
sedentary (sedentary) lifestyle;
changes in the structure of blood vessels;
necrosis of the femoral head;
violation of metabolic processes in the body;
high concentration of uric acid in the patient’s blood (determined in a laboratory blood test);
gout, osteoradionecrosis, bone tuberculosis, Perthes disease, rheumatoid arthritis and other diseases in which bacteria infect the hip joint;
degeneration of the synovial membrane of the joint into cartilage;
circulatory disorders in the hip joint;
various neoplasms;
hormonal disorders in the body;
strong physical stress exerted on the hip joint during sports;
difficult working conditions;
advanced age, etc.
Symptoms of osteoarthritis of the hip joint

With arthrosis of the hip joint, patients experience the following symptoms:
severe pain in the hip and knee joints, as well as in the groin (pain syndrome accompanies this disease constantly, and with the progression of arthrosis, it can integrate into the region of the lower extremities);
impaired motor function (due to excruciating pain, patients cannot move independently, which is why they are forced to use special devices: crutches, canes);
shortening of the lower (affected by arthrosis) limb;
crunch in the joint that occurs with any movement;
lameness and gait disturbance;
stiffness and limited movements of the limbs;
when performing radiography in this category of patients, atrophy of the muscle tissues located in the thigh area is revealed;
when conducting hardware diagnostics, bone growths can be detected in patients;
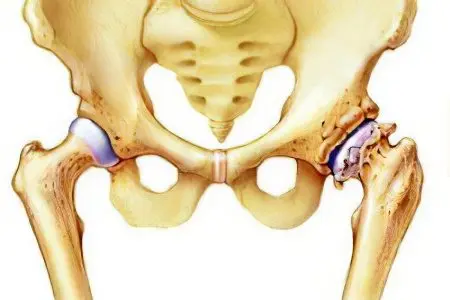
at the 2nd stage of arthrosis in patients, deformation occurs, and the head of the femoral bone is displaced upward (it increases significantly in size and acquires uneven outlines);
with the 3rd degree of arthrosis in patients, the head of the femoral bone expands, as a result of which the narrowing of the joint space begins, etc.
Degrees

To date, medicine knows three degrees of arthrosis of the hip joint. They are accompanied by certain symptoms and directly depend on the stage of the disease.
1 degree
At the first stage of this disease, patients do not have pronounced symptoms, as a result of which people in rare cases go to a medical facility.
With the development of arthrosis of the hip joint of the 1st degree, the following occurs:
the liquid begins to lose its properties;
the consistency of the liquid becomes more viscous;
fluid is not able to provide unhindered movement of the joint.
At the first stage of this disease, the structure of the cartilaginous tissue begins to break down, microcracks form in it. Over time, in the process of progression of arthrosis, thinning of cartilage tissue is observed. In many patients, substitution processes begin to occur, against the background of which bone growths form at the location of the cartilage.
At the first stage, arthrosis of the hip joint is very easy to completely cure. The problem is that patients, due to untimely access to specialists, cannot receive medical care. That is why doctors strongly recommend that people who have discovered any of the symptoms of arthrosis immediately visit the nearest clinic and undergo a comprehensive diagnosis.
2 degree
Arthrosis of the hip joint of the 2nd degree is accompanied by a strong pain syndrome, which can be integrated from the thigh and pelvis into the knee. At this stage of the disease, patients experience severe cartilage damage.
All damage can be seen thanks to X-ray:
thinning of cartilage tissue;
narrowing of the lumen between parts of the joint;
change in the structure of the head of the femoral bone;
the appearance of various neoplasms;
displacement of the head of the hip joint;
the number of bone growths (osteophytes) increases.
When carrying out diagnostic measures in this category of patients, inflammation of the periosteum is detected. If this disease is not treated, pain will increase in patients, motor functions will be impaired, and muscle tissue dystrophy in the lower extremities will develop. Such patients will experience unbearable pain, even while at rest.
3 degree
During the transition of arthrosis of the hip joint to the third stage, patients experience:
excruciating pain;
almost complete destruction of hyaline cartilage tissue;
violation of motor functions (patients are limited in their movements);
atrophy of muscle tissue;
change in gait;
shortening of the lower limb;
joint deformity;
severe narrowing of the joint space;
the spread of bone formations (having a spike-like shape), etc.
At the 3rd stage, the treatment of this disease is possible only surgically, since no medications can restore cartilage and restore mobility to a person. Currently, this category of patients undergo sparing operations, during which the damaged hip joint is replaced with an artificial prosthesis. Thanks to endoprosthetics, patients, after undergoing a long rehabilitation, can return to normal life.
Deforming arthrosis of the hip joint
Deforming arthrosis of the hip joint (coxarthrosis) is a severe form of osteoarthritis. This form of the disease is most often (in 40% of cases) diagnosed in patients who visited a medical facility for problems with the musculoskeletal system. Both women and men who have reached the age of 40 suffer from deforming coxarthrosis. According to world statistics, deforming arthrosis of the hip joint is more often diagnosed in the female half of the population.
There are a large number of factors that provoke the development of coxarthrosis. The main reason for the appearance of this disease is a violation of blood circulation in the pelvic organs. As a result, harmful enzymes begin to accumulate in the body of patients, which have a negative effect on cartilage, leading to their gradual destruction.
The causes of coxarthrosis can be attributed to both the physical and mechanical effects on the hip joint. Most often, this disease manifests itself in people who are professionally involved in sports. Excess weight also puts a strain both on the patient’s joints and on his body as a whole. Deforming arthrosis of the hip joint is usually accompanied by severe pain and limited mobility of the lower extremities. These symptoms should alert the patient and encourage him to contact a specialized medical institution. At the appointment, the patient will be examined and an x-ray will be prescribed, which will determine the degree of damage and the type of arthrosis.
Diagnostics
Many people who develop osteoarthritis of the hip may experience pain during movement or any other physical activity. Initially, the pain syndrome occurs only with physical overwork, but later, patients begin to experience torment even during rest. Pain is often integrated from the hip joint to the lower back, knee, thigh, etc. Against the background of pain, some people begin to self-medicate, which often leads to irreversible consequences. That is why it is necessary, when such a primary symptom of arthrosis appears, to turn to highly qualified specialists who will diagnose.
When visiting a healthcare facility, patients who are suspected of having hip arthritis should seek advice from the following highly specialized specialists:
Therapist. This specialist will assess the general health of the patient and determine the cause of the pain syndrome (sometimes pain occurs due to the progression of various chronic diseases).
Neurologist. Very often, pain in the area of the hip joint is a consequence of the formation of intervertebral hernias, therefore, when such symptoms appear, it is important to consult this specialist.
Urologist. In the male half of the population, pain in the hip joint occurs as a result of inflammatory processes in the prostate gland. A consultation with a urologist will confirm or refute such a suspicion.
Gynecologist. All women who have applied to a medical institution with complaints of pain in the hip joint are referred to this specialist. This is due to the fact that during the development of the adhesive process in the pelvic organs, patients often experience pain, therefore, when diagnosing arthrosis, it is important to obtain the conclusion of this highly specialized specialist.
Rheumatologist or arthrologist. These specialists can diagnose arthrosis of the hip joint at the first stages of its development. With timely access to a rheumatologist or arthrologist, the patient will be guaranteed a successful cure for this disease.
Orthopedist and surgeon. Patients with an advanced stage of arthrosis of the hip joint are referred to these specialists.
In the implementation of diagnostic measures, the specialist will first of all conduct a personal examination of the patient and collect an anamnesis of the disease. During palpation, he will be able to feel the upper third of the lateral surface of the thigh and identify serious injuries on it.
A specialist can carry out a number of simple manipulations, thanks to which it will be possible to make a preliminary diagnosis – arthrosis of the hip joint:
flexion and extension of the lower extremities;
turning the lower limbs in and out, etc.
To make an accurate diagnosis, patients are assigned a hardware and laboratory examination:
x-ray examination (an x-ray will reveal any damage in the hip joint);
arthroscopy;
ultrasound examination of the pelvic area;
magnetic resonance or computed tomography (this diagnostic method allows you to identify arthrosis at the very initial stage of development, when it is not yet accompanied by pronounced symptoms);
a laboratory study of blood and urine (clinical, biochemical) will reveal any inflammatory processes in the patient’s body.
The main task of hardware diagnostics is to identify arthrosis of the hip joint, as well as to determine the degree of this disease. It is very important to determine the cause of arthrosis, since the method of treatment of this disease will depend on this.
Treatment of arthrosis of the hip joint

At the first stage, arthrosis of the hip joint responds well to conservative treatment. The first task of the attending physician is to relieve the pain syndrome that prevents the patient from moving.
In the process of drug treatment is performed:
restoration of damaged cartilage;
restoration of nutrition and blood circulation in muscle and cartilage tissues;
reduced physical load on the injured joint;
activation of the hidden reserves of the human body, which will promote tissue regeneration at the microcellular level;
an increase in the joint space;
restoration of joint mobility, etc.
During the medical treatment of arthrosis of the hip joint, the following drugs are prescribed for this category of patients:
drugs with anti-inflammatory effect (non-steroidal);
painkillers;
muscle relaxants that restore blood circulation in muscle and cartilage tissues;
chondroprotectors that can restore the functions of the joints and stop their destruction;
steroids are prescribed to patients in the form of injections during an exacerbation of the disease to eliminate pain;
medications that can dilate blood vessels, etc.
During conservative treatment, patients should adhere to a diet specially designed for patients with arthrosis of the hip joint. The course of therapeutic therapy includes therapeutic massage, which is indicated for patients with stages 1 and 2 of arthrosis.
[Video] Dr. Evdokimenko – Osteoarthritis of the hip joint – stages 1, 2 and 3:
If the patient finds the following symptoms, he should stop daily activities for a while and contact a medical institution for advice:
exacerbation of chronic diseases;
increase in temperature;
increased blood pressure;
diseases of the heart and blood vessels;
hernias, cysts and other neoplasms, etc.
Prevention

To prevent the development of arthrosis in the hip joint, it is necessary to timely prevent this disease:
timely receipt of qualified medical care for any injuries of the hip joint;
refusal of a sedentary lifestyle;
playing sports;
leisure;
normalization of body weight;
timely correction of congenital or acquired defects of the hip joint;
proper nutrition;
giving up bad habits (smoking, alcohol, etc.);
water sports, etc.









