Contents
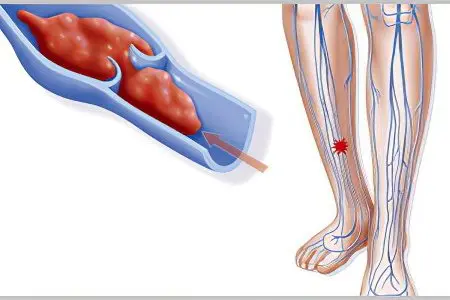
Occlusive thrombosis is the complete blockage of an artery, with impaired circulation distal to the site where the blockage occurred. Occlusive thrombosis can develop anywhere on the body, on any vessel. Pathology is expressed in the absence of pulsation, in blanching of the skin and pain. The victim is shown urgent medical care, in some cases surgery is required. Occlusive thrombosis is a condition that poses a direct threat to life or health. If the patient does not go to the doctor in time, he may lose a limb and become disabled.
Acute occlusive thrombosis most often occurs in men over the age of 60 years.
Depending on the location of the thrombus, doctors give the following statistics:
In 40% of cases, thrombosis of the vessels of the mesentery is observed.
In 35% of cases, occlusive thrombosis develops in the vessels of the brain.
Limb arteries and aortic bifurcation are affected in 25% of cases.
In 34% of cases, femoral arteries are exposed to thrombus occlusion.
In 22% of cases, occlusive thrombosis affects the iliac arteries.
Popliteal arteries are affected in 9% of cases.
In 14% of cases, the pathology affects the subclavian vessels, vessels of the shoulder and lower leg.
Causes of occlusive thrombosis
The cause of occlusive thrombosis is the blockage of the lumen of a vessel or artery by a thrombus. It can be represented not only by a blood clot, but also by fatty, as well as tissue, microbial or tumor fractions.
Diseases against which occlusive thrombosis can develop are:
Heart disease: ischemic heart disease, myocardial infarction, heart disease, arrhythmia, hypertension, atherosclerosis, aortic and cardiac aneurysm, inflammation of the heart muscle, dilated cardiomyopathy.
Tumor neoplasm in the body: a tumor of the heart, a tumor of the lungs.
Congenital malformations of the heart: open foramen ovale, patent ductus arteriosus, defects of the cardiac septum.
Diseases of the blood system: leukemia, polycythemia.
Other pathologies: Takayasu’s disease, periarteritis nodosa
Risk factors that can lead to occlusive thrombosis are:
Transferred operations on the arteries with their damage.
Frostbite of parts of the body.
Vasospasm.
Extravasal compression.
Heart rhythm disturbances.
Blood pressure jumps.
Excessive physical or psycho-emotional overstrain.
Taking medications.
Hypodynamia.
Forced sitting position for a long period of time, including work-related.
Sometimes doctors fail to determine the cause of blockage of blood vessels. A sharp weakening of blood circulation in that part of the body that receives nutrition from the arteries that have undergone occlusion is caused not only by the presence of the thrombus itself, but also by the spasm of the vessel. The fact is that when the speed of blood flow through the clogged veins weakens, it begins to increase its coagulation potential, and the walls of the artery continue to shrink. This leads to the fact that bypass ways of blood flow will also be blocked over time. As a result, the patient’s condition will only worsen, and ischemic lesions will worsen.
On the other hand, the clinical symptoms are enhanced by muscle edema, which increases against the background of the death of cells suffering from oxygen starvation. The damaged vessel itself loses its density, its permeability increases, which also leads to a more pronounced swelling of the affected area of the body.
So, the structure of the veins changed by injuries, injections or infectious processes, increased blood clotting and slowing of blood flow – these are the three factors that will contribute to the growth of symptoms of pathology.
Symptoms of occlusive thrombosis

Symptoms of occlusive thrombosis directly depend on where exactly the pathology develops. The stage of the lesion, the size of the thrombus, etc., are important. The main signs that indicate occlusive thrombosis are as follows:
Pain. It occurs in the area where occlusive thrombosis develops in 80% of cases. Although when blood flow finds a bypass, pain may be absent or mild.
The pain gradually increases, is diffuse in nature. After the person has changed the position of the body, the pain does not subside. It can only pass if the occlusion resolves on its own.
The artery near where the clot formed stops pulsing. The limbs that are fed from the vessel gradually become paler, then acquire a bluish tint. A marble pattern appears on the skin. If you touch it, you can feel the cold.
Occlusive thrombosis is always accompanied by numbness of the affected area of the body, there is a feeling that goosebumps run through the skin.
If we are talking about the limbs, then they lose their muscle strength, the patient is not able to perform full-fledged movements with his leg or arm. As the symptoms increase, the paralysis intensifies more and more, bringing the patient to complete immobility.
Nearby lymph nodes may increase in size and become painful.
With a pronounced inflammatory process in a person, the body temperature rises.
If the patient does not seek medical help, then he may develop gangrene, which will lead to amputation of the leg or arm.
Diagnosis of occlusive thrombosis

Diagnosis of occlusive thrombosis requires an integrated approach, but always begins with an examination of the patient and anamnesis. The doctor must feel the pulsation of the artery in the characteristic places for this. It is possible to carry out specific tests (Moshkovich’s test, Panchenko’s test, etc.).
Laboratory studies for suspected occlusive thrombosis:
Blood sampling for a general analysis, which allows you to confirm the presence of an inflammatory process in the body.
Performing a coagulogram. Against the background of vascular occlusion, there is an increase in the prothrombin index, a jump in the level of fibrinogen.
D-dimmer test, which allows you to diagnose thrombosis with a high probability.
Instrumental methods for examining a patient with suspected occlusive thrombosis:
Performing duplex scanning of blood vessels. This method will give information about the size of the thrombus, the degree of occlusion, the state of the vascular wall, and how much the blood flow through the veins is impaired.
Performing peripheral arteriography.
Computed tomography or MRI angiography.
It is imperative to distinguish between occlusive thrombosis with thrombophlebitis and abdominal aortic aneurysm.
Treatment of occlusive thrombosis
If there is a suspicion of occlusive thrombosis, then the patient must be urgently hospitalized. It must be examined by a vascular surgeon.
Therapy with medications involves the appointment of thrombolytic drugs that are administered intravenously. In parallel, antiplatelet agents, antispasmodics are prescribed. If there is no threat to the life of the patient, then he is sent for physiotherapy, but is not discharged from the hospital. These can be procedures such as magnetotherapy, barotherapy, diadynamic therapy.
All this time the patient must adhere to strict bed rest. To avoid the development of inflammation at the site of occlusive thrombosis, the patient is prescribed therapy with non-steroidal anti-inflammatory drugs. To restore the vascular wall, it is necessary to prescribe phlebotonics.
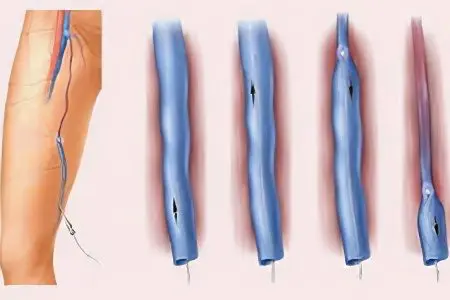
If after a day from the onset of occlusive thrombosis there is no improvement in well-being, then the doctor decides on thromboembolectomy (removal of pathological thromboembolic masses from the lumen of the affected vessel). If the patient develops necrotic tissue changes, then emergency amputation of the limb is indicated. Otherwise, the patient may die.
The prognosis for occlusive thrombosis largely depends on how soon the patient received medical care. The earlier intensive therapy is started, the greater the chances of its successful completion. As a rule, 90% of patients manage to recover. If a person delayed seeking medical help, then there is a high probability of amputation of the limbs that are supplied with blood from the affected vessel, or even the death of the patient.
[Video] Cardiovascular surgeon, phlebologist Abasov M. M. – How to get rid of a blood clot in 2 weeks:









