Contents
- What is atherosclerosis of the lower extremities?
- Symptoms of atherosclerosis of the lower extremities
- Causes of atherosclerosis of the lower extremities
- Diagnosis of atherosclerosis of the lower extremities
- Treatment of atherosclerosis of the lower extremities
- Diet for atherosclerosis of the lower extremities
- Conclusion
What is atherosclerosis of the lower extremities?
Atherosclerosis of the lower extremities – this is a group of pathological processes affecting the main blood vessels of the lower extremities, and representing a progressive violation of the blood supply to tissues due to narrowing (stenosis) or blockage (occlusion) of the arteries. The term “obliterating” in relation to this disease means a gradual but steady narrowing of the lumen of the blood vessels.
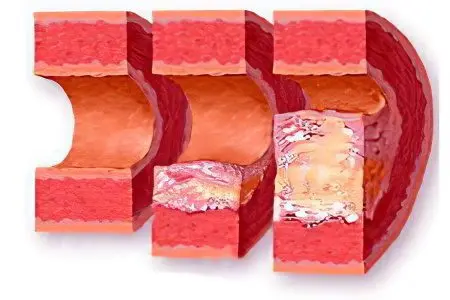
Arteries are large blood vessels. In a normal state, the lumen of the arteries is free and the blood circulates freely through the bloodstream. However, in some cases, the lumen of the vessels narrows, and the surrounding tissues receive less nutrients and oxygen necessary to maintain stable functioning, resulting in ischemia and subsequent necrosis.
In short, the mechanism of the formation of the disease is the blockage of blood vessels or their narrowing. Narrowing is a common cause, for example, for the body of a heavy smoker. Blockage can also occur if a fat-like substance, cholesterol (LDL-lipoprotein complex), is deposited on the walls of the arteries of the lower extremities. However, the process of development of pathology is not so simple and requires a more detailed explanation.
Mechanism of disease development

Most often, atherosclerosis of the vessels of the lower extremities manifests itself in old age and is caused by disorders of lipoprotein metabolism in the body. The development mechanism goes through the following stages.
The cholesterol and triglycerides that enter the body (which are absorbed into the intestinal wall) are captured by special transport proteins-proteins – chylomicrons and transferred into the bloodstream.
The liver processes the resulting substances and synthesizes special fatty complexes – VLDL (very low density cholesterol).
In the blood, VLDL molecules are affected by the enzyme lipoprotein lipase. At the first stage of the chemical reaction, VLDL is converted into intermediate density lipoproteins (or LDLP), and then at the second stage of the reaction, LDLP is transformed into LDL (low-density cholesterol). LDL is the so-called “bad” cholesterol and it is he who is more atherogenic (i.e., capable of provoking atherosclerosis).
Fatty fractions enter the liver for further processing. Here, high-density cholesterol (HDL) is formed from lipoproteins (LDL and LPP), which has the opposite effect and is able to cleanse the walls of blood vessels from cholesterol deposits. This is the so-called “good” cholesterol. Part of the fatty alcohol is processed into digestive bile acids necessary for normal food processing and sent to the intestines.
At this stage, liver cells can “fail” (due to genetics or explained by old age), as a result of which, instead of HDL at the exit, low-density fat fractions remain unchanged and enter the bloodstream.
No less, and possibly more atherogenic, are mutated or otherwise altered lipoproteins. For example, oxidized under the influence of H2O2 (hydrogen peroxide).
Low-density fatty fractions (LDL) are deposited on the walls of the arteries of the lower extremities. Long-term presence of foreign substances in the lumen of blood vessels contributes to inflammation. However, neither macrophages nor leukocytes can cope with cholesterol fractions. If the process is delayed, layers of fatty alcohol – plaques – are formed. These deposits are very dense and interfere with normal blood flow.
Deposits of “bad” cholesterol are encapsulated, and when the capsule is ruptured or damaged, blood clots form. Blood clots have an additional occlusive effect and further clog the arteries.
Gradually, cholesterol fractions in combination with blood clots take on a rigid structure due to the deposition of calcium-containing salts. The walls of the arteries lose their normal extensibility and become brittle, resulting in ruptures. In addition to everything, persistent ischemia and necrosis of nearby tissues is formed due to hypoxia and lack of nutrients.
Atherosclerosis of the vessels of the lower extremities is an insidious pathology. In some cases, it may not manifest itself at all, or it may manifest itself with nonspecific symptoms. For example, a patient can explain chilliness in the limbs or “goosebumps” by the fact that he “served” or “lay down” the limb.
Symptoms of atherosclerosis of the lower extremities
Atherosclerosis of the lower extremities is quite easy to recognize even on your own, subject to an attentive attitude to your own health and feelings. It is manifested by a system of specific and general symptoms.
Feeling of itching, “ripples” in the limbs, goosebumps etc. patients define these sensations in different ways, but often the feeling is similar to numbness of the limb as a result of a long stay in an uncomfortable position. In this case, the symptom is present for no apparent reason.
Feeling of coldness in the lower extremities. Also for no apparent reason. It can also be observed in the warm season.
Paleness of the skin of the legs.
Thinning of the muscle and fat layer in the thighs, legs and feet. Narrowing or blockage of the arteries that provide oxygen and nutrients to the tissues leads to active tissue degeneration.
Complete or partial loss of the hairline of the ankles and shins without subsequent hair growth. It is also associated with the development of tissue degeneration. The system of capillaries in the affected limbs grows unnaturally, but cannot compensate for the lack of blood supply.
Pain in the legs. They are observed at rest, when walking and any physical activity they increase. A specific symptom of atherosclerosis is lameness caused by severe paroxysmal pains.
In more advanced cases: darkening or redness of the feet and toes (tissues acquire an unnatural burgundy or dark red color), which indicates blood stagnation and thrombosis. The symptom is a precursor to such a formidable complication as necrosis.
Formation of ulcers on the legs (the so-called trophic ulcers).
tissue necrosis (gangrene). Appears in the last stages of the process. Since the disease develops rapidly, the stage can come quickly.
Thus, with obliterating atherosclerosis of the lower extremities, a complex of formidable symptoms is observed. Their manifestation indicates the need for prompt medical attention. In most cases, delay and indecision of doctors and patients entail amputation.
Causes of atherosclerosis of the lower extremities
Obliterating atherosclerosis of the lower extremities can develop for many reasons:
Gender. Both men and women are equally affected. The age of persons suffering from atherosclerosis ranges from 45 for males and from 50 for women. Men, as a rule, are 1.5-3 times more likely to acquire this pathology. The reasons for the difference in incidence are not completely clear, but it is assumed that estrogen (the female sex hormone) is able to somehow prevent clogging of the arteries.
Age. As mentioned, with age, the risk of getting sick proportionally increases. With the onset of menopause, the activity of producing sex hormones in the female body decreases, therefore, after 50-55 years, the number of cases among both men and women is approximately the same. In Russia, statistics on atherosclerosis is truly horrifying: 75% of men and 25% of women under the age of 40 suffer from pathology. And at the age indicated above, the number approaches 90%.
Elevated cholesterol and triglycerides. Both substances have the ability to clog blood vessels and cause ischemia. How to lower the level of triglycerides in the blood?
Hypertension. Represents elevated blood pressure. Normal values range from 120/80 to 130/85. Persistent or periodic excess of these figures indicates the presence of hypertension. Vessels with hypertension very quickly lose their elasticity and become brittle. On the inside, “worn out” vessels lose their elastic smooth texture, becoming coarsened. In this state, cholesterol plaques are formed much more actively.
genetic reasons. Atherosclerosis is a polyetiological disease. The hereditary factor plays an important role. By inheritance, the features of lipid metabolism in the body, the features of the hormonal background, as well as the specifics of the immune system, with the help of which the development of atherosclerosis can go faster or slower, are inherited.
Addictions. Nicotine, which abundantly enters the body, being absorbed into the blood, is extremely atherogenic. However, in heavy smokers, the mechanism of atherosclerosis formation is somewhat different. Without a doubt, nicotine can affect lipoprotein metabolism in the body, but most often the cause of acute insufficiency of blood supply to the tissues of the lower extremities is stenosis of the walls of the arteries, and not their blockage. Drugs have a similar, but even more destructive effect, and their use in the vast majority of cases means certain death or severe disability. Alcohol in small therapeutic doses, on the contrary, can have a positive preventive effect.
The presence of concomitant diseases and pathologies. Hand in hand with atherosclerosis goes diabetes. In diabetes mellitus, significant dysfunctions of lipid and lipoprotein metabolism are observed, and therefore, in 75-80% of diabetics, atherosclerosis develops during the first 4-5 years or even faster.
Lack of thyroid hormones (hypothyroidism of the thyroid gland) also affects the normal metabolism, increasing the risk of developing atherosclerosis of the lower extremities by 35-40%.
Stress. Especially if they are permanent and protracted.
Obesity. By itself, it often indicates the presence of metabolic disorders.
Foci of inflammation in large blood arteries.
Diagnosis of atherosclerosis of the lower extremities

Symptoms are not always pronounced, for this reason it is quite difficult to diagnose atherosclerosis without proper medical training. Only an experienced doctor can make a correct diagnosis, and meanwhile, delays in making a diagnosis and timely treatment can cost the patient the affected limbs.
Of great importance in the diagnosis are three main methods:
Samples.
History taking.
Ultrasound examination of the vessels of the lower extremities.
Collection of anamnesis
During the initial examination, a doctor who suspects atherosclerosis in a patient should interview the patient in more detail and take into account all factors.
As a rule, in the anamnesis of patients there is a combination of the following elements:
The presence of “experience” of smoking;
Increased body weight;
Absence of allergic diseases;
Age over 40 years;
Outwardly, the patient looks older than the actual;
Complaints of pain and problems with both legs;
Frequent or moderate attacks of intermittent claudication, which capture many muscles of the legs: from the buttocks to the calves.
The skin of the feet is pale;
The pulse over the large arteries is almost not felt. When listening to the affected areas, extraneous noises are detected.
Present: hypertension, coronary artery disease and/or diabetes mellitus.
The manifestations are permanent. It does not depend on the time of year or day.
There were people in the family with cardiovascular diseases. With a high degree of probability, the patient also has problems with cholesterol.
Functional trials and tests
At the end of the history taking, the doctor confirms his guess with special functional tests:
Functional Burdenko test. Atherosclerosis is associated with stagnant processes in the vessels. When bending the leg at the knee, the foot (sole) is covered with a marble vascular pattern. This indicates a poor outflow of blood from the limb.
Hyperemic Shamov/Sitenko test. Due to the same stagnant processes, the blood circulation of the tissues is disturbed. To detect atherosclerotic disorders in the work of blood vessels, a special cuff is applied to the shoulder or thigh for a period of 3-5 minutes. It compresses the surrounding tissues, preventing normal blood circulation. Normal blood supply (and, accordingly, the pink color) of tissues normally returns after 25-35 seconds. If the vessels are affected by atherosclerosis, it may take up to a minute and a half or more, depending on the degree of narrowing of the channel of the blood vessel.
Functional Moshkovich test to assess the plantar symptom. The patient assumes a supine position. Then he lifts his legs vertically upwards, without bending them at the knee joints. In this position, the patient is asked to remain for two to three minutes. Then the patient takes a standing position. Normally, in a healthy person, the skin turns pale in the first position, because there is an outflow of blood from the lower extremities, and as soon as it gets up, the blood supply is restored, and the skin again takes on a natural pinkish tint within 8-10 seconds or faster. This is not observed in patients with atherosclerosis. Skin from 30 seconds or more is able to maintain a pale color, marble vascular pattern, etc.
If violations have been identified, the doctor conducts a repeated, deeper test, aimed already at establishing the degree of lack of blood circulation (plantar symptom). To do this, the patient lies down again and stretches his legs up. But now he is asked to alternately or together bend and unbend his legs. Motor activity requires blood flow, and its lack will lead to rapid muscle fatigue. Those suffering from atherosclerosis experience rapid fatigue and pallor of the soles of the feet. Depending on the intensity and speed of the onset of these two factors, it is possible to establish the degree of lack of blood flow.
Ultrasound examination
To establish the severity of circulatory disorders, dopplerography of the vessels is used. This study allows you to establish the speed of blood flow and the degree of tissue saturation with essential nutrients and oxygen.
Other research methods
They are numerous and are prescribed to confirm the diagnosis:
Laboratory researches (analyzes). As a rule, with atherosclerosis, there is an increased concentration of triglycerides, LDL, and the most accurate and informative indicator is the so-called atherogenic index (coefficient), which is determined on the basis of the proportion between “good” and total cholesterol.
Radioisotope research allows you to determine the level and quality of blood supply to tissues and determine the degree of anemia.
Radiography makes it possible to establish the localization and size of vascular occlusions.
New diagnostic methods are also being actively introduced, such as spectral scanning, through which you can study the contours of the affected vessels, determine the speed of blood flow through them and measure pressure, and others.
An inexperienced specialist often runs the risk of not seeing the disease. The reason lies in the high adaptability of the body to various adverse factors. The patient develops a collateral blood supply. New blood structures are formed and grow, providing the tissues with the necessary substances. Although this method is unable to replace the normal circulatory system in the affected area, partial compensation is still achieved. This blurs the picture, confusing the doctor.
Treatment of atherosclerosis of the lower extremities

The treatment of atherosclerosis of the lower extremities is a significant difficulty, since the disease, as already mentioned, is polyetiological. Therefore, it can be caused by many reasons. Treatment consists in eliminating the root cause and getting rid of unpleasant and life-threatening consequences. The doctor must act competently and promptly. Atherosclerosis not only significantly reduces the quality of life, but also threatens the health of the patient.
Conservative methods include:
drug therapy;
Physiotherapy.
In extreme cases, resort to surgical methods. Traditionally, highly invasive operations are widely used in our time, but great importance is attached to relatively low-traumatic endoscopic methods of intervention.
Medication Therapy
Drug therapy is complex. The courses of treatment are fractional, carried out for 1,5-2 months with a frequency of up to 4 times a year, depending on the clinical picture. The drugs are aimed at combating spasm of blood vessels and their narrowing. Antispasmodics and drugs that expand the lumen of blood vessels are used (for example, no-shpa, compalamine, etc.).
Statins, fibrates, LC sequestrants are used to lower cholesterol. Of the more modern ones, one can name Ezetimibe-SZ, Evolocumab and Alirocumab. In addition to the main medicines, omega-3s are prescribed.
An important role is given to drugs that increase the rheological qualities of blood and, thereby, improve its circulation (including the well-known aspirin (Trombo ACC, Cardiomagnyl, Cardiask), or, if it is intolerant, more “calm” drugs: Curantil, Ticlid , Plavix, Brilinta, Trental.).
At the request of the patient, herbal preparations that have proven their effectiveness can be used in the complex. These include: Inflaminat, Nattokinase, Revitl Garlic Pearls, Ravisol – more about them is described here.
Physiotherapy
It is used in conjunction with drug therapy. The following types are most effective:
Impact on the affected areas with combinations of direct and alternating current (interference therapy).
Deep injection of drugs through electric current (electrophoresis).
Magnetotherapy.
UHF
These therapeutic procedures contribute to the complete or partial restoration of the work of the affected vessels.
In combination, these methods are highly effective in the early or later stages of the development of the disease. In 90% of cases, in combination with a hypocholesterol diet and the rejection of bad habits, conservative therapy gives the desired effect.
However, treatment does not always help. In addition, a situation may arise in which the process has gone too far and the vessels have finally lost their function without the possibility of its restoration. In this case, surgical intervention is indispensable.
Surgery
Traditionally, vascular prosthetics remain the main method. The damaged vessel that has lost its function is removed, and a prosthesis is installed in its place. Modern vascular prostheses are not much different from natural tissues, therefore they perform their task with dignity and allow the patient to return to a normal and fulfilling life.
Fortunately, for patients, time does not stand still, and a vessel that has been affected, but has not yet completely lost its functionality, can be restored through angioplasty. This is a minimally invasive but highly effective endoscopic method for removing occlusion or stenosis of a blood vessel.
Its essence lies in the fact that the endoscopist, under the control of a video camera, advances the catheter through the bloodstream to the affected area through a puncture in the femoral artery. Upon reaching the affected area of the artery, the doctor expands it, or removes foreign objects, due to which the function of the vessel returns. Unlike a traumatic operation to install a prosthesis, angioplasty is less traumatic. Another issue is that it is not always possible to get by with it.
Diet for atherosclerosis of the lower extremities

By itself, changing the diet is not able to have any therapeutic effect. It is effective either in combination with other therapeutic measures, or as a preventive measure.
A diet for atherosclerosis of the lower extremities is not just a one-time action. To achieve the desired effect, it must be adhered to for a long time. The new way of eating should become, in a way, a way of life. This will provide treatment, and at the same time further prevention. However, in most cases, at the initial stages of the disease, it is rarely necessary to refuse products for a long time.
The diet of a patient with atherosclerosis should include:
Meat products. Lean meat, poultry (preference is given to turkey).
Fish. Fatty fish is also allowed, since its fat has a rather positive effect on the vessels.
Fresh fruits, vegetables and berries – without restrictions.
Dairy products, including fatty ones.
Eggs in boiled and baked form (omelets). The lecithin contained in them, as well as a large amount of cholesterol, which, if properly cooked, will turn into a “good” form, will cleanse the vessels of deposits.
Vegetable oils (olive and sunflower oil).
Cereals, pasta from wholemeal flour. Also bran and bread.
Green tea.
Nuts (especially almonds and walnuts).
Legumes and leguminous crops (lentils, beans, peas).
Dry red wine.
Cheese (less than 30% fat).
It is necessary to limit the consumption of the following foods:
Synthetic foods rich in trans fats. This is margarine, spread.
Limit the consumption of by-products (brain, kidneys, liver) and products from them.
Sausages.
Mayonnaise, ketchup and other industrial sauces.
Potatoes (fried) and fast food. Potatoes are acceptable in small quantities and only boiled (in uniform) or baked.
Adhering to such a diet in conjunction with drug treatment and physiotherapy can alleviate the condition and get rid of the consequences of the disease.
It is worth paying attention to the Mediterranean diet, which, according to studies, reduces the risk of recurrent heart disease by 50-70%.
Conclusion
Thus, obliterating atherosclerosis of the arteries of the lower extremities may be directly related to the level of cholesterol in the blood, or may have nothing to do with it. One way or another, this is an extremely dangerous disease, which, in the absence of adequate treatment, leads to disastrous results. It is quite difficult to determine it (on your own – and completely impossible). Only an experienced doctor can cope with the diagnosis and prescribe treatment.
Fortunately, modern medicine has a full range of diagnostic measures at its disposal. Treatment is usually conservative in the early stages. In addition to traditional medical and physiotherapy, a general improvement of the body and the use of a special diet are recommended. However, in more severe cases, surgery is required.









