Contents
What is neutropenia?
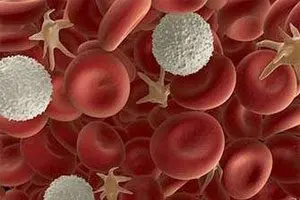
Neutropenia (agranulocytosis) occurs when the level of neutrophils (neutrophilic leukocytes) decreases in the blood (becomes less than 1500 in 1 μl). This leads to an increase in susceptibility to a variety of bacteria and fungi, reduces the body’s resistance to infections, and reduces immunity.
This condition can act as an independent disease, as well as as a result of other pathologies or external causes that affect the human body. In this case, neutropenia is a complication of a particular disease.
Agranulocytosis – a decrease in granulocytes in the blood in general. Granulocytes are represented by neutrophils, eosinophils and basophils (all of them belong to leukocytes). Neutrophils in this list are the most numerous. Therefore, often a doctor, speaking of agranulocytosis, has in mind precisely neutropenia.
Neutrophils destroy the pathogenic flora that has entered the body, and are also sent to the focus of inflammation and try to neutralize it. Pus is the result of the destruction of microbes, it is represented by their remains and dead neutrophils.
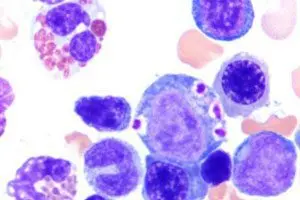
Neutrophils are synthesized in the bone marrow, where they mature, after which they enter the blood and tissues.
The normal level of neutrophils varies from 45 to 70% of all leukocytes. Neutropenia is indicated by a decrease in the level of neutrophils less than 1,5 * 109/ l. Black people have fewer neutrophils in their bone marrow than white people. Therefore, their neutropenia is indicated by a drop in the number of neutrophils to 1,2 * 109/ L.
Severe neutropenia is extremely rare, but this condition is dangerous not only for health, but also for life. To help a person, it is necessary to clarify the cause of the decrease in the level of neutrophils.
Types and degrees of neutropenia
Depending on the rate of development, the disease can be acute, occurring over a few days, or chronic, developing over many months or years.
Dangerous for human life is only a severe acute form of neutropenia, which can occur due to a violation of the formation of neutrophils.
The norm of neutrophils in the blood is 1500/1 μl. Based on this, three degrees of neutropenia are distinguished by the number of neutrophils:
Mild neutropenia, in which the level of neutrophils drops to 1.0-1.5×109/ L.
Moderate neutropenia, in which the level of neutrophils decreases to 0.5-1.0×109/ L.
Severe neutropenia, in which the level of neutrophils falls below 500 neutrophils per microliter of blood.
In severe neutropenia, the risk of developing health complications is extremely high.
There are the following types of neutropenia:
Autoimmune. This type of neutropenia develops under the condition that antibodies begin to be produced in the body that destroy neutrophils. Such a reaction can manifest for no apparent reason, or develop with other autoimmune diseases. Children born with immunodeficiency often suffer from this type of neutropenia.
Medicinal. This type of neutropenia is most often found in adult patients. Its causes may be hidden in the body’s allergic reactions to drugs. Penicillins, cephalosporins, chloramphenicol, neuroleptics, sulfonamides and anticonvulsants can provoke a drop in the level of neutrophils. After completion of the course of treatment, neutrophil counts return to normal (after 7 days).
Anticonvulsants are more likely to cause neutropenia. An allergic reaction is indicated by skin rashes and itching, fever and other symptoms. Be sure to cancel the drug, to which the body reacts with neutropenia. If this is not done, then a person may develop a serious immunodeficiency.
Neutropenia may manifest during chemotherapy or radiation therapy. In this case, the effect is on the bone marrow. After the start of treatment, the level of neutrophils will be markedly reduced already after 7 days. Restoration of the number of neutrophils occurs no earlier than a month later. During this period, the risk of damage to the body by various infections is high.
Infectious. Infectious neutropenia accompanies SARS and other acute infections. Most often, such neutropenia does not last long and resolves on its own after an average of 7 days. Infectious neutropenia due to HIV, sepsis and other serious diseases has a severe course. In this case, there is a failure in the production of neutrophils at the level of the bone marrow, as well as their death in the peripheral vessels.
Febrile. Febrile neutropenia develops during the treatment of tumors of the hematopoietic system with cytostatics, but sometimes it manifests itself during chemotherapy of other cancerous tumors. A severe infection develops in the body, which leads to the active growth of pathogenic flora against the background of insufficient immunity. Moreover, for a healthy person, such pathogens most often do not pose a threat to life (staphylococci, streptococci, fungi, herpes virus, etc.). However, the lack of neutrophils becomes fatal for the patient. His condition deteriorates sharply, and it is difficult to identify the source of infection, since the inflammatory reaction is very weak. The immune system is simply unable to cause it.
Benign. Benign neutropenia is a chronic condition that is diagnosed in childhood. Treatment is not required. As the child grows older, the level of neutrophils returns to normal. Doctors attribute the development of such neutropenia to the immaturity of the bone marrow in children under 2 years of age.
Hereditary. Congenital neutropenia: Costman’s syndrome, cyclic neutropenia, familial benign neutropenia, lazy leukocyte syndrome.
Causes of neutropenia
Neutropenia can develop as an independent anomaly, or as a result of various blood diseases. The most common cause of neutropenia is a decrease in the formation of neutrophilic leukocytes under the influence of drugs (antitumor and anticonvulsants, penicillin, antimetabolites, etc.). Sometimes the disease is a predictable side effect of taking a number of medications, and sometimes it occurs regardless of the dosage and timing of the use of a particular medication.
In rare cases, neutropenia is a congenital anomaly. Inhibition of neutrophil production may be due to hereditary agranulocytosis, familial or cyclic neutropenia, pancreatic insufficiency, renal failure, or HIV. Also, neutropenia can be caused by bone marrow damage, cancer, or even beriberi (deficiency of vitamin B12 and folic acid).
Symptoms of neutropenia

Symptoms that indicate the development of neutropenia can be very diverse, but they all develop against the backdrop of a failure of the immune system.
Therefore, signs of neutropenia can be considered:
Ulceration in the mouth. Perhaps the formation of areas of necrosis.
Dermatological diseases.
Inflammation of the lungs, intestines and other organ systems.
Increased body temperature.
Sepsis.
It is stomatitis, gingivitis and tonsillitis that are the basic signs of neutropenia. In this case, the inflammation is always acute, accompanied by painful sensations, swelling of tissues, bleeding gums. Such damage is caused by fungal microorganisms.
People with neutropenia are prone to respiratory diseases that are severe. They are accompanied by cough, fever, wheezing, pain in the chest.
The intestines with neutropenia are covered with ulcers and areas of necrosis. A person develops diarrhea or constipation. He is haunted by pain in his stomach. This condition is dangerous by perforation of the intestinal wall and the development of peritonitis, which is associated with a high risk of death.
Integuments with neutropenia can be covered with purulent rashes. In parallel, there is an increase in body temperature. Skin rashes do not go away for a long time, they can fester and ulcerate.
If neutropenia has a mild course, then it may not manifest itself in any way. A decrease in the number of neutrophils can be suspected by frequent viral infections. As neutropenia progresses, the patient begins to get sick longer, treatment becomes ineffective. In addition to viral infections, a person will suffer from attacks by fungal and bacterial flora. Severe neutropenia is accompanied by damage to internal organs, febrile conditions, acute inflammation. Possible development of sepsis and death.
Treatment of neutropenia

Neutropenia cannot be treated with a single regimen. It is important to determine the cause of the development of this condition. The choice of therapeutic measures is influenced by the age of the patient and his state of health.
Mild neutropenia, which does not have severe symptoms, does not need treatment. If a person develops severe neutropenia, the patient is hospitalized. The development of complications requires the appointment of antibiotics, antifungal and antiviral drugs. The dosage of drugs for people with neutropenia should be higher than the dose for the treatment of patients without neutropenia.
The choice of the drug is based on the sensitivity of the pathogenic flora to it. If it is not identified, then the patient is prescribed broad-spectrum antibiotics. They are administered intravenously.
If after 72 hours there is no improvement, then the scheme is recognized as ineffective and the drugs are changed, or the dose of the antibiotic is increased.
When neutropenia is provoked by tumor neoplasms or chemotherapy, the patient should receive an antibiotic until the neutrophil level reaches 500 cells per microliter of blood.
If a fungal infection is diagnosed in a patient with neutrophilia, then in addition to antibiotics, he is prescribed fungicides. They are used only for the treatment of mycotic lesions, and are not used for prophylactic purposes.
Co-trimoxazole can be used to prevent bacterial complications in neutropenia. However, its use is associated with the risk of developing candidiasis of various organs.
Children with congenital neutropenia, as well as persons with severe pathology, may be prescribed colony-stimulating factors, for example, Filgrastim. And this treatment is becoming more and more popular.
To increase the immunity of the patient, he is prescribed vitamin complexes with the obligatory content of B vitamins.
When neutropenia is autoimmune in nature, patients are shown the introduction of glucocorticosteroids.
Pentoxyl and Methyluracil preparations allow accelerating tissue regeneration and improving metabolic processes.
If a lot of neutrophils die in the body, then the removal of the spleen may be required. The operation is not performed in patients with sepsis or with the development of severe complications of neutropenia. Another radical treatment for neutropenia is a bone marrow transplant from a donor.
People with neutropenia need to follow certain preventive measures. This will prevent the development of severe complications at the stage of restoring the level of neutrophils. Be sure to wash your hands with soap. Limit contact with people who are carriers of the infection. It is equally important to avoid various injuries, including minor cuts and scratches. Food must be subjected to sufficient heat treatment. The implementation of these recommendations will reduce the likelihood of penetration of pathogenic flora into the body at the stage of treatment of neutropenia.









