Contents
- Neuritis – what is it?
- The symptom is neuritis
- Complications of the disease
- Causes of Neuritis
- How to distinguish neuritis, neuralgia, neuropathy?
- Neuritis classifications
- Alcoholic neuritis
- Diagnosis of neuritis
- Treatment of neuritis
- Prevention of neuritis
- Nutrition recommendations
- Which doctor treats neuritis?
Neuritis – what is it?
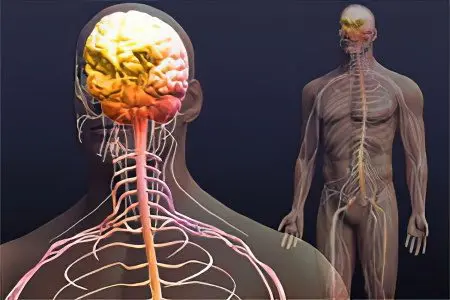
Neuritis – this is inflammation of the peripheral nerves, which is accompanied by pain and decreased sensitivity, paralysis and paresis are possible. In addition, the disease is characterized by movement disorders.
Innervation is the provision of tissues and organs with nerves, through which the central nervous system gives them a command to perform a particular function.
Neuritis can cause partial or complete paralysis.
There are nerves that suffer from inflammation more often than others:
Visual.
Auditory.
Facial.
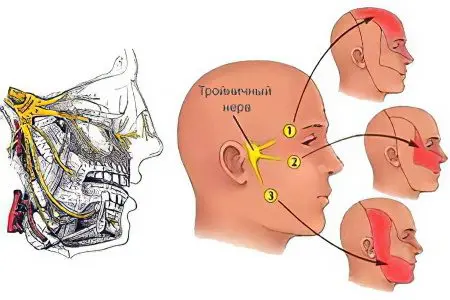
Trinity.
Ray.
Sciatic.
If the nerve becomes inflamed in only one place, we are talking about neuritis. When several nerves are exposed to inflammation at once, polyneuritis is indicated.
Neuritis is manifested by such symptoms as: deterioration of sensitivity, numbness, impaired motor functions, pain. In severe cases, movement of the affected area of the body becomes impossible.
A variety of infections, injuries, growing tumors, hypothermia, and diseases not associated with pathogenic flora, such as osteochondrosis or arthritis, can provoke the development of neuritis.
The mechanism of development of neuritis
The nervous system allows a person to exist. It is responsible for the mechanism of breathing, smelling, thanks to it people move, hear, see, etc. The peripheral nervous system is a huge internal organization that consists of many nerves.
The nerve itself is a unit of the nervous system. It is represented by plexuses of nerve fibers that are covered with a myelin sheath. Nerves connect the brain and spinal cord to each other and to other organs.
Inside the nerves are blood vessels.
If the nerves are large, then they are called nerve trunks. Branches branch out from these trunks. All nerves have a different structure.
Neuritis has a complex mechanism of development. But against the background of absolute health, it never arises. It is always preceded by any disturbances: vascular, metabolic, etc. An injury or a tumor growing in the body can cause the development of neuritis.
Pathological factors destroy myelin and Schwann cells, which are responsible for the transmission of nerve impulses. If the violation is serious, then the axial cylinder suffers. The affected nerve is not able to function normally, which leads to disruption in the functioning of organs and tissues.
Most often, neuritis is diagnosed in women in old age.
Neuritis according to ICD-10
According to the ICD-10, neuritis has the code M79.2, and neuropathy – G60-G64.
The symptom is neuritis

Symptoms of local neuritis are quite typical. These are steadily dull pains with paroxysmal irradiation along the nerve. There is also a violation of sensitivity, movement disorders occur, and at the site of the lesion – slight muscle atrophy. In more complex situations, the tendon reflexes may disappear, but rarely comes to paralysis.
The first manifestations of the disease:
Pain concentrated in the area of inflammation.
Deterioration of the sensitivity of the affected area, its numbness.
Tingling of the sore spot.
The symptoms of the disease will vary, depending on which nerve fibers are affected, as well as on how intense the inflammation is.
In this regard, neuritis can be manifested by such signs as:
Feeling of crawling all over the body, numbness of the affected area, tingling. All these symptoms occur if sensitive fibers have undergone inflammation.
Paresis and paralysis are the main symptoms of inflammation of the motor fibers. The patient’s muscles may atrophy, tendon reflexes will stop working.
Hair loss in the affected area, vitiligo, xeroderma, skin edema, deterioration of nails, ulcers, increased sweating. All these symptoms develop when the vegetative fibers are damaged.
Depending on which nerve is affected, the symptoms of the disease will vary:
Inflammation of the auditory nerve. This nerve is responsible for transmitting sound to the brain. Its damage is accompanied by the appearance of tinnitus, hearing loss. Often people complain of dizziness.
Damage to the optic nerve. A person complains of eye disorders. First of all, this concerns the deterioration of vision, which sometimes reaches complete blindness. The patient may have flies before his eyes.
Damage to the axillary nerve. A person notes that he has reduced sensitivity in the shoulder area, in 1/3 of its upper part. The joint in this area begins to hurt, the deltoid shoulder muscle gradually atrophies. It is difficult for a person to raise his hand or take it to the side.
Damage to the radial nerve. Depending on where exactly the inflammation is concentrated, the symptoms of neuritis will be slightly different:
Inflammation of the armpit or inflammation at the level of 1/3 of the shoulder is characterized by pain during flexion of the arm in the elbow joint. It becomes problematic to straighten the forearm, hand and thumb. The carporadial reflex worsens. If a person stretches his arms forward, then the hand of the affected limb will hang down. The patient is unable to turn the palm up.
If the inflammation is concentrated in the middle 1/3 of the shoulder, then the elbow and shoulder joints do not suffer.
If the inflammation is concentrated in the lower 1/3 of the shoulder, or in the upper forearm, then the sensitivity of the back of the hand worsens, it is difficult for a person to straighten not only the hand, but also the fingers.
Inflammation of the ulnar nerve. The disease has some features:
Deterioration of sensitivity and paresthesia of the palm. In this case, the area of the 5th finger suffers, as well as half of the 4th finger.
Decreased sensation in the back of the hand. Half of the 3rd finger suffers, the 4th and 5th fingers become completely numb.
Muscular weakness of the 4th and 5th fingers increases, their muscles atrophy. This leads to the fact that the hand resembles the appearance of a clawed paw. At the same time, the fingers at the base remain straight, and bend in the region of the middle phalanx.
Sometimes neuritis of this localization resembles the clinical picture of carpal tunnel syndrome.
Damage to the median nerve. Violation develops acutely, a person experiences severe pain in the fingers, as well as on the inside of the forearm. Then the sensitivity of the palm worsens, while half of the 4th finger and from 1 to 3 fingers suffer. Their man cannot bend. Also, the hand does not bend in the area of the wrist joint. The person is unable to rotate the arm so that the palm is pointing down. The thumb is atrophied. In appearance, the hand begins to resemble a monkey’s paw.
carpal tunnel syndrome. Clinical manifestations of inflammation proceed according to the type of tunnel syndrome, since the median nerve in the wrist area will be pinched. The patient is numb from 1 to 3 fingers. At first, this feeling occurs from time to time, and then it begins to bother a person on an ongoing basis. The pain is localized in the palm area, as well as in 1, 2 and 3 fingers. It is aching, gaining intensity during a night’s rest, and can spread to the elbow and shoulder. If a person sets the brush in motion, painful sensations lose their intensity. When the hand remains for 2 minutes in a bent position, the patient begins to feel how his fingers go numb (1, 2 and 3). The thumb loses its strength, sometimes its elevation undergoes atrophic processes.
Plexitis or lumbosacral plexopathy. The lower limbs lose their normal strength. The legs lose their sensitivity, the lower back and pelvis begin to hurt in the joints. Tendon reflexes become weak or disappear altogether.
Neuritis of the sciatic nerve. With this disease, there are pains in the buttocks that radiate to the thigh, to its back surface. Pain may radiate to the lower leg and foot. The Achilles reflex disappears. The pain is dull, but from time to time it occurs in the form of lumbago. A characteristic sign of neuritis of this localization is Lasegue’s syndrome, in which pain intensifies when trying to lift a heavy object with the foot in the supine position.
Inflammation of the femoral nerve. A person has difficulty when trying to bend the leg at the knee or in the hip joint, the sensitivity of the thigh in its lower part worsens. In this area, muscles begin to atrophy, severe pain appears if pressure is applied to the points under the inguinal ligament or to the exit point of the nerve in the thigh.
When cases are not severe, recovery occurs in about 2-3 weeks, but most often it takes longer, particularly in the elderly, and recovery is incomplete. Sympathetic methods are used to treat local neuritis.
Complications of the disease
Neuritis can lead to the development of complications such as:
Paresis.
Paralysis.
Replacement of normal muscle tissue with coarse connective tissue fiber.
Causes of Neuritis
Neuritis can be caused by such reasons as:
Received injuries. These include bone fractures, soft tissue bruises, muscle and tendon tears, fractures, electric shocks, exposure to radiation, etc.
Inflammation of internal organs.
Tumors growing inside the body.
Viral and bacterial infections.
Diseases: measles, influenza, diphtheria, osteochondrosis, kyphosis, scoliosis, lordosis, arthritis, herniated disc, VVD, atherosclerosis, hypertension, tunnel syndrome, allergies, diabetes mellitus, thyrotoxicosis, uremia, brucellosis, rheumatism, herpes, syphilis, leprosy, malaria, blood diseases.
Water deficiency in the body.
Subcooling.
Intoxication with food, alcohol-containing liquids, medicines, chemicals.
Vitamin deficiency.
Congenital anatomical anomalies.
Sometimes a person experiences symptoms of neuritis if he remains in an uncomfortable position for a long time. This can happen during a night’s rest, or because of the peculiarities of the profession. Symptoms of neuritis often affect people who lead a sedentary lifestyle.
How to distinguish neuritis, neuralgia, neuropathy?

Neuritis, neuralgia and neuropathy are different diseases that differ in the mechanism of their development, etiological factors, and clinical picture. Therefore, it is wrong to combine them into one concept.
Neuritis is an inflammation of a nerve located on the periphery. The disease is accompanied by damage to the nerve fiber itself. The myelin sheath and the axial cylinder suffer.
Neuropathy – this is a lesion of the peripheral nerves, while the nerve trunks most often suffer, and not its single branches. The nerve undergoes degenerative and metabolic destruction. Neuropathy can be caused by injuries, disorders in the circulatory system, metabolic failures. Symptoms of the disease are: deterioration of sensitivity, suppression of reflex activity, loss of strength. Neuropathy is a concept that is appealed not only by neurologists, but also by psychiatrists. In the latter case, the disease is understood as the increased excitability of the nervous system against the background of its excessive fatigue.
Neuralgia – this is inflammation of the peripheral nerves, but at the same time the person will not suffer from paralysis, from paresis or deterioration of sensitivity. The nerve itself is not damaged much, its myelin sheath is not destroyed, or deformed slightly. The main symptom of neuralgia is pain. It can be quite intense, focusing on the area of the affected nerve. At the person sensitivity can worsen, vegetative frustration sometimes join.
Neuritis classifications

Depending on how many nerves were involved in the pathological process, mononeuritis and polyneuritis are distinguished. In the first case, inflammation occurs in only one nerve, and in the second case, several nerve fibers suffer at once.
Depending on the location of inflammation, optic neuritis can be of the following types:
Retrobulbar or orbital neuritis. The optic nerve becomes inflamed outside the eyeball. The area that is located from the exit from the sclera to the chiasm suffers.
Axial retrobulbar neuritis. Inflammation will be concentrated in the maculopapillary bundle of the optic nerve. This is a serious pathology that can cause blindness.
Interstitial retrobulbar neuritis. The sheath of the optic nerve undergoes inflammation. It spreads into his deep structures towards the table.
Peripheral retrobulbar neuritis. Inflammation originates from the sheath of the optic nerve and passes to its tissues. With this type of neuritis, fluid will accumulate in the subdural and subarachnoid space.
Transversal neuritis. With this pathology, the optic nerve suffers along its entire length. The disease takes its beginning in the axial bundle, or on the periphery, and then spreads to other tissues.
False optic neuritis. This is a pathology of the development of the optic nerve. Symptoms of the disorder resemble inflammation, but the nerve itself does not atrophy, and visual function does not suffer.
In addition to optic neuritis, the following types of inflammation are distinguished:
Axial neuritis, when the axial cylinders of nerve fibers become inflamed.
Interstitial neuritis, in which connective tissue structures of nerve fibers suffer. Pathology most often develops against the background of autoimmune processes in the body.
Parenchymal neuritis. First of all, the myelin sheath of the nerve and its axial cylinders suffer, and then the inflammation passes to its connective tissue structures.
Vegetative neuritis. In this case, nerve fibers located on the periphery are exposed to inflammation.
Ascending neuritis. Such inflammation develops most often against the background of injuries of the lower or upper extremities. Then the pathological process begins to spread to the central nervous system.
cochlear neuritis. The auditory nerve in the cochlear part suffers. In this case, the patient begins to hear extraneous noises, his hearing deteriorates.
Classification by symptoms
There are three types of neuritis:
Gombo’s neuritis, in which the myelin sheath surrounding the nerve is destroyed. Axial cylinders in this case do not suffer.
Hypertrophic neuritis of Dejerine-Sotta. When the disease occurs, hypertrophy of the sheath of nerve fibers. First, the adducting part of the nerve is subjected to compression, and then it begins to collapse and loses its functionality.
Neuritis Rossolimo. This is a type of Dejerine-Sotta neuritis. The disease gets worse and then subsides. Most often, children suffer from this pathology.
According to the etiological factor
Depending on what exactly caused the development of neuritis, the following types are distinguished:
Traumatic neuritis. The disease develops against the background of a previous injury to the nerve fiber.
Professional neuritis. Pathology is a consequence of the characteristics of a person’s profession. So, inflammation often occurs in people who come into contact with heavy metals, chemical vapors. The effect of radiation on the body is negatively reflected.
Infectious neuritis. Inflammation of the nerve fiber occurs due to the infection of the body.
Alcoholic neuritis. Nerves suffer due to the fact that a person abuses alcohol. At the same time, vitamin B is washed out of the body, which is responsible for the normal functioning of the nervous system. In addition, with excessive alcohol consumption, nerve cells themselves die.
Alcoholic neuritis

The most common type of polyneuritis is alcoholic neuritis. Obviously, it is associated with a lack of vitamin B, which is typical for people suffering from alcoholism. The first signs of the disease are numbness, tingling, weakness in the limbs, namely in the hands and feet. Over time, the pain intensifies, the sensitivity of the skin increases, it becomes smooth and dry. Often there is keratosis (excessive keratinization) of the palms and feet. Deep reflexes disappear, muscle weakness becomes stronger (sometimes to the point of paralysis), while the functions of the bladder and rectum are not disturbed.
Symptoms are usually bilateral. The most commonly affected muscles are innervated by the peroneal and radial nerves. Violations of tactile and deep sensitivity are often detected. Nails become brittle, break, deform, hair becomes thinner. Severe cachexia (exhaustion), severe muscle atrophy, and vasomotor disorders occur. Alcohol consumption leads to blindness. During treatment, bed rest, prevention of contractures with splints and massage, maintaining the normal temperature of diseased limbs, analgesics and a diet rich in vitamins are recommended.
Diagnosis of neuritis

To confirm the diagnosis of neuritis, the patient will be referred for examinations such as:
Electromyography
Electroneurography
Functional trials
They, in turn, can be the following:
Diagnosis of radiation neuritis. A person puts his hand on the table, but at the same time he cannot put his 3rd finger on the fingers next to him. The brush is placed with the back side on the table and the person is asked to remove the thumb. He cannot do this. Then the patient is asked to stand up and put his hands down. In this position, he cannot turn the affected hand with the palm forward and is unable to withdraw his thumb.
Diagnosis of neuritis of the ulnar nerve. The patient puts the brush on the table. In this position, he cannot perform scratching movements with his little finger. The hand continues to lie on the table, the person is asked to spread his fingers apart. Particular difficulties arise with 4 and 5 fingers. Also, a person cannot clench them into a fist and will not be able to hold a strip of paper with his index finger and thumb. The thing is, none of them are fully folded.
Diagnosis of neuritis of the median nerve. A person cannot perform scratching movements with a finger on the surface on which his brush lies. The patient is unable to clench his fingers into a fist. This is especially true for fingers 1 and 2, and the 3rd finger is partially bent. A person will not be able to oppose the thumb to the little finger.
Treatment of neuritis

To cope with neuritis, it is necessary to direct efforts to eliminate the cause that led to its occurrence.
The main directions of therapy:
Elimination of the etiological factor of neuritis.
Taking medications.
Physiotherapy treatment.
Operation.
It will not be possible to cope with neuritis if the cause that led to its development remains unresolved. In parallel, efforts should be directed to the treatment of chronic diseases, if any.
List of medicines

Only a doctor can prescribe drugs for the treatment of neuritis. Self-administration of any medication is an unacceptable measure.
If neuritis develops against the background of an infectious process, then efforts should be made to eliminate it. When the cause of the disease is microbes, the patient is prescribed antibiotics. If the infection is of viral origin, then the patient is prescribed antiviral drugs.
The drug is selected depending on the sensitivity of the pathogenic flora to it:
Amoxicillin, Vancomycin, Clarithromycin, Erythromycin, Oxacillin. These drugs are prescribed for staphylococcal infections.
Erythromycin, Azithromycin, Doxycycline, Levofloxacin, Ceftriaxone, Cefotaxime – these drugs are prescribed for streptococcal infections.
Sulfamoxol and Sulfanilamide are drugs from the group of sulfonamides that can be used to treat neuritis.
Betaferon, Interlok, Laferon, Neovir, Reaferon and gamma globulins are indicated for admission if neuritis is of a viral nature.
The pathogenic flora that multiplies in the human body poisons it. Because of this, the patient may feel sick and even vomit, his body temperature rises, weakness increases, and general well-being worsens. Intoxication increases with the mass death of bacteria and viruses.
To remove them from the body, a person is prescribed detoxification therapy, which can be carried out in the following areas:
The use of sorbents: Atoxil, Polyphepan, Enterosgel.
The use of large volumes of liquid. Well, if it is enriched with vitamin C.
Taking diuretics: Furosemide and Diacarb.
Intravenous administration of glucose solution, polysaccharides, water-salt solutions.
To reduce inflammation and relieve pain, the patient is prescribed drugs from the NSAID group. In severe neuritis, glucocorticosteroids (Prednisolone) can be used. Representatives of NSAIDs – Ibuprofen, Diclofenac, Nimesil, etc.
If a child’s body temperature rises with neuritis, then it can be wiped with water and vinegar.
With tunnel syndrome, injections with Novocaine or Hydrocortisone are performed to eliminate inflammation. They are injected directly into the affected canal. If the disease was caused by a malnutrition of the nerve against the background of ischemia of the blood vessels, then vasodilator drugs are indicated. For this purpose, Eufillin or Papaverine can be used.
Neuritis is accompanied by a number of symptoms that can worsen a person’s life, reduce its quality. Therefore, the patient is shown taking medications aimed at eliminating these symptoms. So, in order to reduce the likelihood of developing muscle spasms, the patient is prescribed Persen or Bekhterev’s medicine.
In order for the damaged nerve to recover faster, a person must receive vitamins. Therefore, with neuritis, vitamins of group B, vitamin E, ascorbic acid, nicotinic acid, milgamma, neurobion, neurorubin are necessarily prescribed.
Auxiliary drugs that can be used at the discretion of the doctor are: antihistamines, antiplatelet agents, angioprotectors, inhibitors of proteolytic enzymes. Gravitational therapies can also be applied.
Physiotherapy

Patients with neuritis may be recommended physiotherapy methods such as:
Plasmapheresis
Mud treatment.
Muscle massage in the area of inflammation.
Hyperbaric oxygenation.
Current treatment.
UHF
Muscle electrical stimulation.
Ultraphonophoresis with hydrocortisone.
Electrophoresis with novocaine, neostigmine and hyaluronidase.
Often, patients with neuritis are selected for therapeutic and physical education complexes. Exercises depend on where exactly the inflammation is concentrated. Physiotherapy begins to be implemented on the 6-7th day from the start of the treatment of neuritis.
In what cases is the operation performed? An operation is prescribed for patients with neuritis if he has suffered an injury that led to inflammation of the nerves. The help of a surgeon may be required, provided that the medical correction was ineffective, or there are no signs of improvement in well-being.
Prevention of neuritis

To prevent the development of neuritis, it is necessary to observe such preventive measures as:
Protect yourself from injury.
Follow the rules of personal hygiene.
Avoid hypothermia.
Timely treat all diseases, prevent them from becoming chronic.
Do not take drugs that are not prescribed by the doctor.
Eat foods that are rich in vitamins and nutrients.
Nutrition recommendations
A person suffering from neuritis should eat well, nutrition should be rich in vitamins, mainly group B, which are most in brewer’s yeast, pork, cereals – oatmeal and buckwheat – peas, beans, wheat bread; vitamin B6 is found in yeast, beef liver, kidney, meat, yolk, cheese, milk.
The patient is advised to drink plenty of fresh vegetable juices, especially carrot juice.
Which doctor treats neuritis?
If symptoms of neuritis appear, you should consult a neurologist.









