Contents
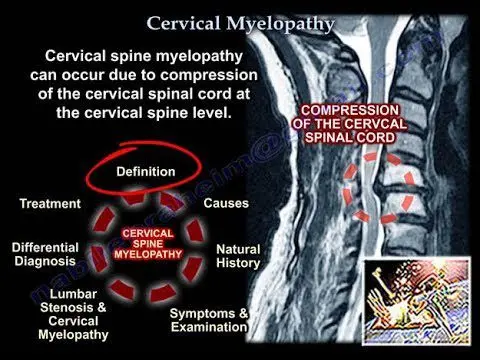
Myelopathy: how to treat cervical myelopathy?
Cervical myelopathy is damage to the spinal cord in the cervical vertebrae. Degenerative causes are the most common. At the onset of the disease, disorders typically predominate in the upper limbs in the form of pain, tingling or decreased tenderness in the arms, forearms or hands. Clumsiness is frequent with episodes of dropping objects. In more advanced forms, muscle weakness appears in the upper limbs and / or lower limbs with fatigue when walking. Sexual or sphincter disorders are also part of the symptoms. Usually, surgery is offered if the myelopathy is established, with severe compression of the spinal cord. Several technical methods exist but the systematic element is the release of the spinal cord, possibly associated with spinal arthrodesis.
What is cervical myelopathy?
While the term “myelopathy” means “dysfunction of the spinal cord”, cervical myelopathy corresponds in particular to damage to the spinal cord at the level of the cervical vertebrae.
Myelopathy is said to be “arthritic” when it is secondary to osteoarthritis lesions, linked to aging, causing narrowing of the cervical canal, itself leading to chronic compression of the spinal cord and neurological incapacity. We then speak of cervico-arthritis myelopathy.
The so-called “degenerative” cervical myelopathy, on the other hand, corresponds to a progressive and symptomatic spinal cord compression caused by degenerative lesions of the cervical spine. It is the leading cause of myelopathy after 50 years.
What are the causes of cervical myelopathy?
We can distinguish the degenerative causes which are the most frequent, traumatic causes (sprains and fractures), tumors, infectious or inflammatory.
Indeed, the aging of the cervical spine leads to degenerative lesions which lead to a narrowing of the central spinal canal and therefore compression of the spinal cord. These lesions include:
- soft or calcified herniated discs;
- osteoarthritis spurs such as parrot beaks or disco-osteophytic bars;
- slippage of the vertebrae (spondylolisthesis) or hypermobility (intervertebral instability);
- thickening or calcifications of the vertebral ligaments;
- a posterior articular cyst developed at the expense of the joints.
In some patients with constitutionally reduced central spinal canal size, the cervical spinal cord may be compressed with minimal damage.
What are the symptoms of cervical myelopathy?
Symptoms of cervical myelopathy are linked to three types of syndromes.
Spinal syndrome
Osteoarthritis lesions cause compression of the spinal cord and nerves, but they also usually cause neck and back pain. These pains are aggravated by exertion.
Lesional syndrome
It corresponds to neurological disorders located at the level of compression of the spinal cord and nerves:
- motor impairment: the impairment is then severe. Paresis (partial paralysis), paralysis, or clumsiness may result. The patient lets go of objects, finds it difficult to write and perform other simple actions of daily life such as buttoning his shirt;
- painful attack: it is cervico-brachial neuralgia. Electrical pain starts in the neck and goes to the shoulder, arm, elbow, forearm, hand and fingers;
- sensory impairment: the patient loses sensitivity in the arms, forearms or hands with a feeling of cardboard skin. He also suffers from tingling or an unpleasant cramping sensation.
The sub-lesional syndrome
The compression of the spinal cord resounds over the entire area under this crushing:
- walking is then disrupted with loss of balance, falls and muscle wasting linked to the decline in activity. The walking perimeter is reduced and the patient sometimes uses one or two canes or a walker in very advanced forms;
- in general, there is little pain in the lower limbs;
- late, we also observe vesico-sphincteric disorders with a pressing desire or difficulty urinating;
- erectile dysfunction is often present but can also be caused by other pathologies associated with aging.
The spontaneous course of the disease in the absence of treatment is characterized by the aggravation of neurological disorders in stages. This development is generally very slow and insidious, which often leads patients to consult late.
How to treat cervical myelopathy?
Medical treatment is not very effective in cases of myelopathy. This is why the surgical intervention should be discussed as soon as the first signs appear.
In the beginner forms, the surgeon may decide to monitor the patient at regular intervals.
Usually, surgery is offered if the myelopathy is established, with severe compression of the spinal cord. This consists of decompression of the spinal cord. Depending on the type, location and extent of spinal cord compression, an anterior approach, on the front of the neck, or a posterior approach can be used:
- anterior approach: release of the spinal cord through the disc space (trans-disc arthrodesis) or by removing a piece of vertebra (corporectomy);
- posterior approach: laminectomy – that is to say removal of the vertebral lamina, the posterior part of the vertebra, to free the channel of the spinal cord (with or without arthrodesis, or fusion of two or more vertebrae) -, laminoplasty vertebral (enlargement of the canal).
The aim of this treatment is above all to stabilize the progression of the disease. Functional improvement is observed in nearly 70% of cases. After surgery, the neurological problems usually go away. However, they may regress only incompletely, hence the importance of early management. In some particularly severe forms, myelopathy may worsen despite properly conducted surgical treatment.