Contents

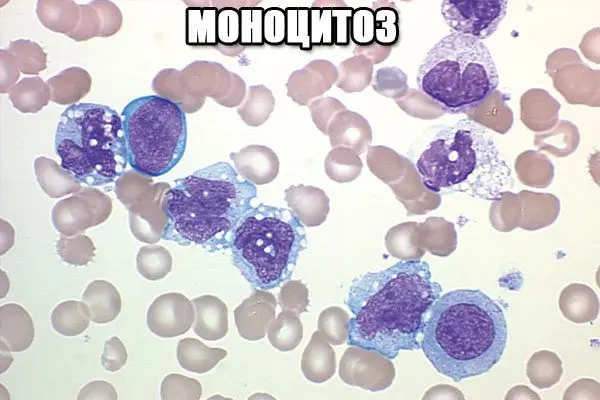
Monocytosis is an increase in the total volume of monocytes in the peripheral blood, most often develops against the background of an infectious disease, although it can also be recorded with other somatic pathologies. The state of monocytosis cannot be characterized as an independent disease. An increase in monocytes is one of the symptoms detected by laboratory diagnostics.
ICD code
ICD-10: D72.8
ICD-9: 288.8
DiseasesDB: 22713
Briefly, what are monocytes
Monocytes, macrophages, mononuclear phagocytes, phagocytic mononuclear cells are all types of non-granular leukocytes. There are no larger cells in the leukocyte group. The most impressive cellular parameters were formed taking into account the performance of certain vital functions for the body – the absorption and destruction of foreign bacteria, mutated or dead cells, immune complexes AG-AT. In a simpler language, we can say that monocytes perform the role of cleaners in the internal environment of the body, eliminating the consequences of inflammatory or pathological processes. Some authors call leukocytes of this type “janitors”, “orderlies”.
Immature monocytes enter the bloodstream and live in it for about three days. After this time, monocytes are transferred to the internal tissues, where they mature and transform into macrophages. Since that time, cells have fully displayed their physiological properties and perform “professional” functions. It can be argued that the group of mononuclear phagocytes consists of monocytes circulating in the bloodstream and tissue macrophages, which are fixed in the tissues of internal organs and are characterized by low mobility.
The mononuclear phagocyte system in the medical field often has other definitions: macrophage, phagocytic mononuclear system, mononuclear phagocytic system. In earlier specialized literature, it was referred to as the reticuloendothelial system – RES. Any of the above definitions contains a mention of phagocytosis, in connection with which the excess of the normal parameters of these cells – monocytosis – is characterized as a manifestation of the protective properties of the body, in response to the influence of pathogenic factors, viruses, bacteria. Monocytes are active participants in cellular and humoral immunity. In the first case, the phagocytic function is activated, and in the second, a combined action is carried out with lymphocytes, also related to non-granular cells of the leukocyte series.
Monocytosis, how normal

The physiological indicator of the norm of monocytes in adults can be fixed at the level of 2-9%. Some sources point to 3-11%. The absolute value of monocytes in the analysis in this case is from 0,09 to 0,6 * 109/ l. Starting from the first days of life and up to a year, infants have a higher level of cells of this type, as well as in the period of 6-7 years, associated with the phase of active growth. The normal indicator of the absolute value of monocytes at this age is 5-12%.
The development of monocytosis is not always a sign of the disease. In clinical medicine, a number of physiological conditions may be accompanied by an increase in the number of phagocytic mononuclear cells:
After a heavy meal.
The period of teething in young children – previously this process was perceived as absolutely not affecting the well-being of the child and blood counts.
At preschool age, up to the second crossover of the leukocyte formula.
At the end of menstrual bleeding, a local inflammatory process develops, which is associated with rejection of the inner layer of the endometrium. This is a completely normal process, not associated with any disease, but requires the presence of macrophages. The task of the “cleaners” is to eliminate cells that have already fulfilled their function, to provide the necessary conditions for the restoration of a new functional membrane of the uterus.
In any other case, the development of monocytosis occurs against the background of any disease. Pathological changes in the blood picture are formed due to the influence of infection or other non-infectious factors. Monocytosis can be divided into two types – absolute and relative.
Absolute monocytosis is formed due to an increase in the absolute volume of young macrophages – more than 1,0 * 109/ l. Simultaneously with an increase in the level of monocytes, there is an increase in the indicators of other cells that are part of the leukocyte formula, for example, neutrophils, basophils. The state of absolute monocytosis develops as a protective reaction of cellular immunity to the action of an infectious factor – bacteria, virus, fungus. In this case, the mechanism of cleansing the body is quickly launched.
About relative monocytosis can be said in the case when the percentage of monocytes increases, with a normal volume of other white blood cells. This condition develops against the background of other groups of leukocyte cells – neutrophils, eosinophils.
The difference between the two types of monocytosis lies in the fact that with an absolute high content of phagocytic mononuclear cells is observed throughout the disease, up to complete recovery, while a relative increase in monocytes is recorded only in the acute period.
Causes of pathological monocytosis

Indicators of absolute monocytosis over 1,0 * 109/l can be a symptom of a serious illness. The factors leading to an increase in the level of monocytes are most often:
Bacterial infections, provoking a number of severe pathologies – syphilis, tuberculosis, rickettsiosis, diphtheria, brucellosis, endocarditis of bacterial origin. This group includes protozoa, leading to protozoal infection, malaria, leishmaniasis, as well as fungi.
Viral infections – infectious mononucleosis, hepatitis, measles, rubella.
Malignant pathological processes hematopoietic systems – lymphogranulomatosis, leukemia, paraproteinemic hemoblastosis, monocytic and myelomonocytic leukemia.
Pathologies accompanied by an active inflammatory process in combination with the formation of granulomatous changes tuberculosis, ulcerative colitis, sarcoidosis. The mechanism of granuloma formation is directly related to the actions of macrophages.
Systemic autoimmune diseases that cause changes in the connective tissue (collagenosis) – rheumatism, rheumatoid arthritis, systemic lupus erythematosus, systemic scleroderma.
Chemical poisoningboth organic and inorganic origin. Intoxication is possible when toxic compounds enter the body, most often through the respiratory tract or by contact. Poisonous substances that cause monocytosis are tetrachloroethane, phosphorus and its compounds.
Recovery phase after infections – measles, diphtheria, rubella, respiratory diseases. During the period when the manifestation of specific symptoms decreases, a decrease in the level of monocytes in blood tests is also observed. If, against the background of an apparent recovery, prolonged monocytosis is determined, one should think about the fact that the root cause has not been completely eliminated or the underlying disease can be transformed into a chronic form.
Tumors of a malignant nature.
Condition after surgical treatment.
Neutrophils are the first to react to the appearance of an inflammatory focus – cells of the granular type. The next to enter the battle are monocytes. That is why the indicators of these blood elements are often simultaneously noted at a high level. In some cases, monocytosis is combined with neutropenia. This phenomenon is the result of immune disorders, in which the lack of neutrophils is compensated by a high level of monocytes.
Does monocytosis always require intervention?
All attempts to independently eliminate monocytosis in the blood will be ineffective. To change the analysis, you will need to completely eliminate the cause of the changes. If the disease has become chronic, the body may not respond to this with any obvious symptoms. In this variant, a person with monocytosis does not present any complaints. Long-term monocytosis should alert the attending physician. To find out the root cause, you will need to perform a set of diagnostic measures to eliminate changes in the peripheral blood.
If an infectious agent is established, the appointment of antibacterial or antiviral agents will be required. In the case of a systemic disease, a long treatment protocol must be followed. The expediency of complex measures is determined by the attending physician.
Correction monocytosis
The elimination of monocytosis is based on finding out the cause that served as its development. After an adequate diagnosis, a specific treatment is prescribed. In the case when monocytosis persists after an infectious disease, therapy is not prescribed. After the end of the recovery period, changes in the blood will pass on their own.
Conservative treatment

Specific treatment is prescribed to eliminate long-term persistent monocytosis. Therapy can be divided into types:
Anti-infective – used in case of viral diseases. Be sure to comply with bed rest. The patient is provided with a plentiful hot drink. Non-steroidal anti-inflammatory drugs (ibuprofen, paracetamol) are prescribed from medications. Symptomatic measures include gargling, washing the nasal passages, instillation of vasoconstrictor drops into the nose. If a bacterial pathogen is detected, antibiotics are prescribed, and specific anti-tuberculosis drugs are prescribed for the treatment of tuberculosis.
Anti-inflammatory – it is advisable for chronic collagenosis, granulomatosis. Mandatory drugs – glucocorticosteroids (prednisolone, methylprednisolone). Immunosuppressants (methotrexate, cyclophosphamide) give the necessary powerful effect in case of prolonged, pronounced inflammation.
Chemotherapy – the main method of treatment of malignant diseases of the circulatory system, histiocytosis. For a more pronounced therapeutic effect, chemotherapy drugs can be administered intrathecally – directly into the cerebrospinal fluid.
Useful and harmful products

A normal white blood cell count means a person is healthy. When their number is increased, this indicates the body’s fight against infection. A low level of monocytes signals a weak immune system.
It is known that the qualitative composition of blood depends on what products a person consumes.
It includes the following products:
Olive oil.
Green vegetables, leafy salads.
Tomatoes.
Berries: strawberries, blueberries, cherries.
Oranges.
Nuts.
Fatty fish: tuna, salmon, mackerel, sardines.
There are also foods that increase inflammation. These include:
Red meat and products based on it.
Fried dishes.
Any pastry, pasta is not made from durum wheat.
Sweet carbonated drinks.
Margarine, lard.
The best example of an anti-inflammatory diet is the Mediterranean diet. It is based on fresh vegetables and fruits, the menu regularly includes nuts, seeds, olive oil and whole grains.
In order for leukocytes to remain within the normal range, you need to play sports. Regular physical activity helps to normalize the level of monocytes. This is especially true for older people.
Independently analyze the leukocyte formula should not be. If a person has suspicions that his level of monocytes is too high, you need to consult a specialist.
Surgery
Surgical intervention is possible for the treatment of oncological blood pathologies, congenital neutropenia. For this purpose, hematopoietic stem cells from a healthy donor are transplanted. The method is based on HLA typing, a genetic test. The study determines the histological compatibility antigens of a potential donor with a recipient. The technique has a high mortality rate, therefore it is rarely used, in case of ineffective conservative treatment.









