Contents
Medical treatments and complementary approaches to painful periods (dysmenorrhea)
Medical treatments
pharmaceuticals
Nonsteroidal anti-inflammatory drugs. Period pain is usually relieved by the use of nonsteroidal anti-inflammatory drugs (NSAIDs), the effect of which is to interfere with the formation of pro-inflammatory prostaglandins. Ibuprofen (Advil®, Motrin®) is available over the counter. Another type of NSAID may be prescribed by the doctor if ibuprofen is not suitable, such as naproxen (Anaprox®, Naprosyn®) or mefenamic acid (Apo-mefenamic®, Ponstan®). They are used as soon as symptoms appear, for 2 or 3 days. They relieve pain caused by uterine contractions as well as headaches, nausea and diarrhea. Nonsteroidal anti-inflammatory drugs can cause side effects, the most common of which are heartburn, diarrhea, abdominal pain and headache.
Medical treatments and complementary approaches to painful periods (dysmenorrhea): understand everything in 2 min
Although NSAIDs are generally effective, 20% to 25% of women8 are not relieved by these drugs.
Oral contraceptives. Symptoms can also be relieved by taking an oral contraceptive, which prevents ovulation, reduces the production of prostaglandins, and reduces menstrual flow. This method is generally effective in reducing not only the length and abundance of periods but also the pain that accompanies them. Some people also choose to stop having their period by taking the birth control pill continuously, which indirectly fixes the pain problem or by switching to Depo-Provera® (a contraceptive given by injection that causes amenorrhea).
It is also possible to take contraception containing progestin alone, continuously. Usually, your periods are much less heavy and sometimes stop during treatment, which resolves the pain problem. Menstruation resumes when treatment is stopped.
Contraceptive by injection. Depo-Provera® (a contraceptive administered by injection that causes amenorrhea) is also offered but it is not without side effects: irregular bleeding, weight gain, decreased libido. In addition, these effects cannot be stopped once the substance has been administered and one must wait until the end of efficacy (4 months) to return to normal.
Intrauterine device (IUD). Another option is to wear the Mirena® IUD. It is an intrauterine device containing a progestin. It fits into the uterus. In addition to being contraceptive, it significantly reduces menstruation and pain. It should only be changed every 5 years.
In case of dysmenorrhea caused by gynecological disorder, the doctor will treat the condition causing the pain. Consult our Uterine Fibroma and Endometriosis fact sheets to learn more about their treatment.
Tips to reduce pain:
|
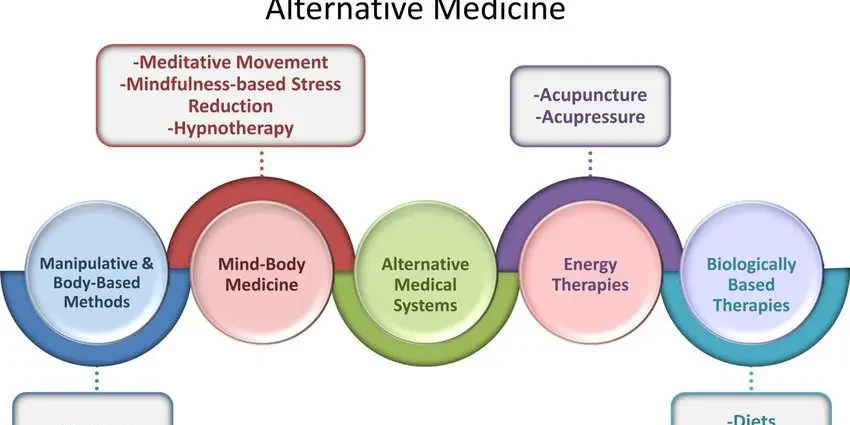
Complementary approaches
Caution. The clinical studies reported in this section focus on dysmenorrhea that occurs in adolescence or just before menopause, when the pain is not caused by a particular gynecological problem (such as endometriosis). In case of severe and sudden menstrual pain, consult a doctor. |