Contents
Leukoplakia of the cervix is a gynecological disease, the mechanism of development of which has not yet been fully understood. Therefore, no specialist can give an answer whether a particular patient will have a benign or malignant course of leukoplakia.
Statistics on the prevalence of cervical leukoplakia varies widely. According to various sources, the disease occurs in 1,1-12,5% of women.
Leukoplakia – what is it
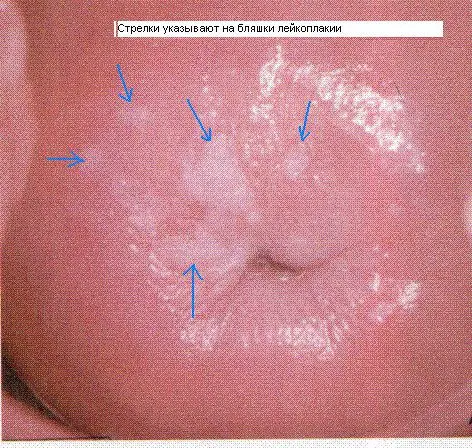
Leukoplakia is a thickening and keratinization of the epithelium of the vaginal or visible part of the cervix. Translated from the Greek language, the term “leukoplakia” sounds like “white plaque”. In foreign medical sources, this disease is called dyskeratosis or intraepithelial neoplasia.
General pathogenesis. After a pathological effect has been exerted on the cervix, inflammation develops. The body starts a protective process that contributes to its keratinization. Normally, this shouldn’t happen. Over time, the epithelium is reborn, plaques and scales form on it. There is no glycogen in these areas of keratosis.
Leukoplakia classification
Depending on the characteristics of the course of the disease, leukoplakia can be of 3 types:
Simple leukoplakia. This form of violation is detected in the early stages of the development of the disease. Plaques do not rise above the surface of the cervical mucosa, being on the same level with it. If the doctor examines the patient in the usual way, then it will be difficult to detect this form of pathology.
warty leukoplakia, which is also called the verrucous form of the disease. White growths are located on top of each other, so the cervix looks bumpy. The doctor will not be able to miss this form of the disease even with a standard gynecological examination.
Erosive leukoplakia. White plaques appear on the cervix, which will be covered with cracks or erosions.
If leukoplakia is detected, the doctor takes the altered tissue area for histological examination. This will make it possible to understand whether a woman has simple leukoplakia or proliferative. With a simple form of the disease, there are no atypical cells in the tissues. Proliferative leukoplakia is considered as a precancerous condition.
Causes of cervical leukoplakia
Scientists have only assumptions about what causes leukoplakia. They believe that both internal and external factors negatively affect the state of the cervix. Moreover, any of them can start the pathological process.
Internal factors in the development of leukoplakia:
Hormonal imbalance. If the pituitary gland, hypothalamus, uterus or ovaries are disturbed, hormone production fails. This affects ovulation, the menstrual cycle, there is a failure in the production of estrogen and progesterone. Therefore, diseases such as:
hyperplasia of the endometrium.
Uterine fibroids and other tumor processes in the organ.
Ovarian dysfunction.
Inflammatory process in the genital area:
Endometritis.
Adnexitis
Vaginitis.
Cervicitis.
Failure of metabolic processes in the body:
Overweight, including obesity of varying severity.
Diabetes.
Diseases of the thyroid gland.
Weakening of the immune forces:
Immunodeficiency congenital and acquired during life.
Deficiency of vitamins in the body.
Treatment with certain drugs. Cytostatics negatively affect the immune system.
External factors that can lead to the development of leukoplakia:
Cervical injury. They can be obtained during childbirth, during an abortion or other procedures, such as hysteroscopy or diagnostic curettage.
Any aggressive effect on the cervix, for example, its electrocoagulation or chemical treatment.
Sexually transmitted diseases.
Infection with chlamydia or HPV.
Infection with ureaplasmosis, mycoplasmas, cytomegalovirus infection.
Early onset of sexual activity and promiscuity.
Symptoms of cervical leukoplakia

A woman will not be able to notice the symptoms of leukoplakia on her own. Most often, the disease is detected during a gynecological examination. Sometimes patients complain of a certain discomfort, but most often it will be caused not by leukoplakia, but by the factors that provoked it.
These symptoms include:
Pain during intimacy.
The appearance of blood after intercourse.
Change in the nature of the discharge. They may give off an unpleasant odor.
Burning and itching in the genital area. These symptoms occur if the inflammation has spread to the vagina.
During the examination of the patient, the doctor visualizes the cervix, which is covered with a white film. Can’t be removed with a swab. Detachment of the film is accompanied by the appearance of blood. This characterizes the initial stage of leukoplakia.
If a woman develops a warty form of the disease, then the film will protrude several millimeters above the surface of the cervix. It is removed with a swab. Shiny pink shells are visible under it. The plaques can be round or oval.
Symptoms indicating the degeneration of leukoplakia into cancer
It is known that leukoplakia can become malignant. In this case, the woman has the following symptoms:
Rapid increase in the size of the affected area.
The appearance of erosions or seals on the cervix.
The plaque area loses uniformity.
The appearance of an ulcerative defect on leukoplakia.
Formation of a papilla or wart on leukoplakia.
All of these changes can only be detected by a doctor. Therefore, patients with leukoplakia should regularly visit a gynecologist.
Pregnancy and leukoplakia

If leukoplakia was diagnosed in a woman who wants to become a mother, then first you need to get rid of the pathology and only after that start trying to conceive. By itself, the disease is not capable of harming the health of the fetus or complicating the course of pregnancy. However, during the bearing of a child, the hormonal background changes. Under the influence of hormones, the disease can progress.
If the pathology was found in a pregnant woman, then her treatment is postponed. Therapy is carried out after delivery. Experts strongly recommend that a woman give birth in a natural way, if there are no other contraindications for this. A ban on independent childbirth is a condition in which plaques on the neck begin to grow rapidly and spread to the vagina. In such a situation, the woman is shown a caesarean section.
Diagnostics

To identify leukoplakia, a woman will need to undergo a comprehensive diagnosis. First you should visit a gynecologist and tell him about your complaints. The doctor will take an anamnesis and examine the woman on the chair. Additional studies that may be assigned:
The study of the smear. A swab taken from the vagina and from the cervix is sent for bacterial culture and PCR. This allows the detection of sexually transmitted diseases.
smear cytology. Cytological examination provides information about which cells represent the epithelium. The doctor takes a smear-imprint from the cervix. The procedure is performed using a special brush or Eyre spatula. In a woman with leukoplakia, stratified epithelial cells are found in a smear from the cervix. Normally, such cells are present only in its vaginal part. The epithelium is changed, signs of hyperkeratosis are revealed (most of the scales do not have nuclei). It is also possible to detect signs of parakeratosis.
Colposcopy. If leukoplakia is suspected, the doctor examines the cervix using a special device – a colposcope. This allows you to detect changes that are invisible to the naked eye. It also becomes possible to visualize the altered areas characteristic of a precancerous condition.
When the pathological areas of the cervix are visible when viewed on the mirrors, the doctor diagnoses “severe clinical leukoplakia.” When violations are detected only during examination using a colposcope, the doctor indicates the colposcopic form of the disease.
In the latter case, the woman will have iodine-negative zones that can be detected during the Schiller test. To do this, the cervix is treated with a solution of iodine. The test is considered positive if the entire organ turns brown. A negative sample is characterized by the presence of unpainted areas. Zones with leukoplakia do not respond to iodine, since there is no glycogen in the altered cells. It is he who gives a brown color when treated with Lugol’s solution.
Also, using a colposcope, you can visualize puncture, which is represented by red dots. The mosaic and sections of the cervix of different thicknesses are visualized. Such diagnostic signs should alert, as they indicate precancerous tissue transformation.
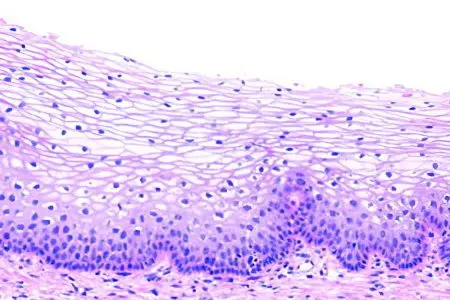
Histology. To implement this method in practice, you will need to perform a biopsy of the cervix with curettage of its canal. Fabrics are taken from the area that has undergone changes more than the others. Histological examination allows assessing the condition of the cells and identifying atypical formations in them.
Leukoplakia is characterized by such signs as:
Acanthosis.
The presence of horny scales, which normally should not be.
Proliferation of stratified epithelial cells.
Epithelial tissues are unevenly thickened, as intermediate cells are located between them.
Under the stratum corneum is a granular layer.
There are signs of hyperkeratosis and parakeratosis
The cells are saturated with lymphocytes.
Evaluation of the work of the ovaries. To do this, ultrasound is performed, measurements of basal body temperature are carried out, etc.
Immunogram. This study is prescribed only if indicated.
Treatment of cervical leukoplakia

To get rid of leukoplakia, you need to contact a gynecologist. To combat the disease, there are various methods. The primary task that confronts the doctor is the relief of inflammation, if any. It is also necessary to get rid of the factors that provoked the development of leukoplakia.
For the treatment of infectious diseases, antibiotics, antiviral agents, antimycotics are used. The choice of the drug depends on what kind of pathogenic flora multiplies in the female genital organs.
If the patient has hormonal imbalances, then its correction is required. After the treatment is completed, efforts can be made to get rid of leukoplakia.
Diathermocoagulation
This method involves the treatment of the cervix with electric currents. Simply put, altered tissues are cauterized. The current source is a special loop that is in contact with the affected area. The effectiveness of this method of treatment is 70%. However, this procedure for a woman is very painful. Therefore, not all patients decide on it. The advantages of electrocoagulation include its low cost and availability. Devices for its implementation are available in all gynecological clinics.
In modern medical practice, they try not to resort to such a painful method. If it is nevertheless carried out, then it is implemented in the first phase of the cycle, after the end of menstruation.
The disadvantages of electrocoagulation include:
Soreness.
The risk of exacerbation of diseases of the uterus and its appendages.
risk of bleeding. Moreover, it can happen both during the procedure and at the recovery stage, if the scab starts to move away too early.
Long rehabilitation period.
Scar formation in the treatment area. Sometimes it is quite rough and large, leading to fusion of the cervical canal. Therefore, electrocoagulation is carried out only for women who have already given birth to children.
Cryodestruction
Cryodestruction involves the treatment of the affected area with cold. The efficiency of this method reaches 94%. Pathologically altered tissues are exposed to liquid nitrogen. Cells crystallize, their walls are destroyed and pathological tissues die. The processing time depends on the area of the lesion. The whole procedure lasts about 2-5 minutes.
The positive aspects of cryodestruction include:
Absence of pain.
High efficiency.
No bleeding.
The possibility of implementation in nulliparous women.
No scar after the procedure.
However, cryodestruction has certain disadvantages. For example, there is a possibility of recurrence of the disease. In addition, the cervix may become shorter in size, making it more difficult to conceive naturally.
Laser treatment
Treatment of leukoplakia with a laser is the most popular method. Carry out the procedure in the first phase of the menstrual cycle. For its implementation, the introduction of painkillers is not required.
There is no direct contact of tissues with the device. altered cells are burned out with a laser beam. The fluid from the cells evaporates, due to which they are destroyed. After such cauterization, a thin film is formed on the surface of the mucous membrane. It prevents pathogenic flora from entering the treated area. If leukoplakia has spread to the vagina, then the treatment is implemented in 2 stages. First, the affected cells are removed from the cervix, and then from the vaginal walls.
The advantages of the procedure include:
Absence of pain.
High efficiency.
The possibility of treating nulliparous women.
Absence of blood.
Fast recovery. Tissues completely regenerate in 16-40 days.
However, not every clinic is equipped with equipment for the procedure. In addition, its cost is quite high.
Radio wave treatment

Treatment of the cervix with radio waves is carried out using the Surgitron apparatus. This method of treatment is highly effective and safe. There is no direct contact of tissues with the apparatus. A special device is inserted into the cervical canal, which is a source of radio waves. They destroy pathological cells due to the evaporation of moisture from them.
The advantages of radio wave therapy include:
Absence of pain.
Absence of blood.
No scar.
Fast regeneration.
There are no downsides to the procedure. The only drawback of the method is that specialized equipment is not available in all medical institutions.
Chemical coagulation
This method of treatment comes down to applying a special drug to the cervix – Solkovagin. It contains acids that cauterize the affected tissue.
Such treatment can be recommended to nulliparous women. It is not associated with pain and bleeding. The effectiveness of therapy is 75%. However, the drug penetrates to a depth of no more than 2,5 mm. Therefore, with severe leukoplakia, it will not allow to cope with the disease. In addition, large areas of mucous membranes cannot be treated with the drug.
Rehabilitation
After treatment of leukoplakia, intimacy should be abandoned for 6 weeks. It is forbidden to swim in hot water, lift heavy objects. You should not visit the sauna and bath.
A woman should refrain from inserting tampons, she should not douche. Intimate hygiene must be performed impeccably.
In the first week after treatment, liquid discharge may appear from the vagina. This is a natural reaction of the body to the therapy.
Answers to popular questions
Is it possible to completely get rid of leukoplakia and what is the prognosis? It is possible to achieve a full cure in 99% of cases. The prognosis is as favorable as possible if the pathology was detected in the early stages of the development of the disease. If the risk factors are not eliminated, then there is a possibility of relapse. Malignancy of the process is observed in 15% of women.
Is it necessary to be registered with a dispensary with such a diagnosis?? After treatment, all women are registered. Every 6 months she will need to visit a gynecologist and take a smear for cytology. Be sure to perform a colposcopy and an HPV test. If after 2 years the recurrence of the disease did not happen, then the woman is removed from the register.
Can you get pregnant with cervical leukoplakia? Leukoplakia is not an obstacle to conception. Pregnancy may not occur for other reasons, for example, due to hormonal failure or sexual infection. You can plan a pregnancy only after getting rid of the pathology.
Can I get vaccinated against cervical leukoplakia? Yes, Gardasil or Cervarix can be given. They help to avoid infection with HPV, which causes the development of both leukoplakia and cervical cancer.
Is intimacy possible with leukoplakia? Yes, it is possible. However, experts recommend not to delay the treatment of this pathology.









