Contents
Leprosy – what is this disease?
Leprosy (or leprosy) is a chronic infectious disease. It affects the skin and nerves located on the surface. The cause of leprosy is prolonged contact with the skin of a sick person. According to some experts, infection can also occur through the air. Contrary to existing myths about the disease, rare touching of the affected areas of the skin cannot cause leprosy. Prejudices include the idea of incurable leprosy and poor prognosis (fatal outcome). It should also be noted that the incidence of leprosy is low among people at risk for whom there is a real risk of infection. No more than 10% of individuals do not have sufficient immunity and cannot resist the penetration of the pathogen, therefore, it is believed that the pathogenicity of microorganisms that cause leprosy is relatively low.
The disease is not very contagious. It affects no more than 7% of people worldwide. The rest of the population (about 95%) is immune to this disease. It does not allow infection to enter the body. Leprosy cannot be inherited, the child does not get the infection from the mother.
The peak of the spread of leprosy was observed in the 12th-16th centuries. Most of the inhabitants of Europe suffered from it. At that time, leprosy was considered a disease that could not be cured. People affected by the infection were exiled. They were expelled from the city, forced to wear a goose foot around their neck, and also to ring a bell if they were going to approach a healthy person.
Now the peak of the incidence has subsided, but cases of infection with leprosy are still being diagnosed. Therefore, doctors need to be attentive to patients with characteristic complaints. In Russia, the disease was last officially registered in a migrant from Tajikistan. It happened in 2015. The man worked in the capital at a construction site.
Facts from history:
The disease in past centuries spread during the Crusades. When sick warriors and knights became infected and infected the inhabitants of other countries.
The plague stopped the leprosy. During the epidemic, people with weak immune systems who suffered from leprosy were the first to fall ill.
In France, there was a decree. According to it, all people with leprosy were subjected to a “religious tribunal.” They were taken to church, buried, and then laid in a coffin. When the coffin was lowered into the grave, they said the phrase: “You are dead to us, not alive.” Then a few shovels of earth were thrown onto the coffin. After that, the person was taken out of the grave and sent to the leper colony. He was not allowed to return to the house. In a specialized institution, he remained until the end of his days. His relatives considered him dead.
People with leprosy were deprived of all social rights. They could not go to church, to places of entertainment, to fairs. It was forbidden for infected people to swim in reservoirs, drink running water, eat with healthy people, and even talk to them.
Catholics allowed couples to divorce if one of the spouses had leprosy, although the Catholic Church rejects divorce as such.
In the Middle Ages, leprosy was called by different terms, including: Phoenician disease, black sickness, lazy or slow death, mournful disease. The name “leprosy” was coined in Russia. This word comes from the old Russian “kazit”, that is, to disfigure or distort.
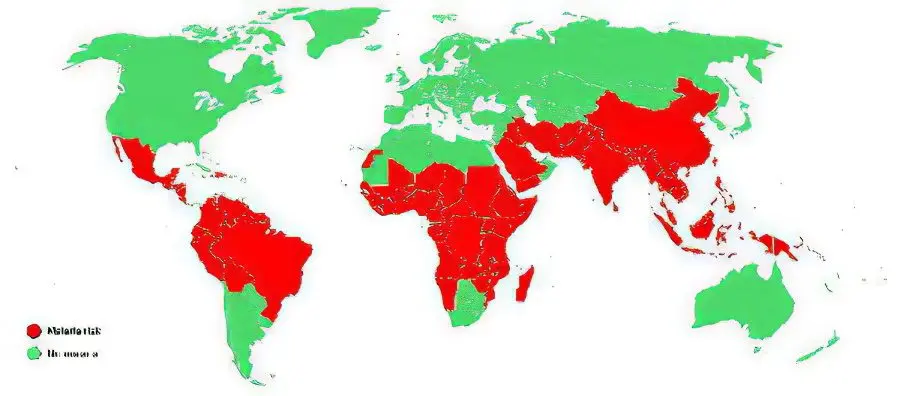
Geography and features of the distribution of leprosy
Today, no more than 2 million people live with leprosy worldwide. The decrease in the number of infected people occurred in the nineties, before that time there were about 12 million. In Russia, according to 2007 data, 600 people with leprosy were registered, 35% of them received treatment in the hospital, and the rest were treated at home.
Today, leprosy is practically not found in regions that are characterized by a cold climate, it is mainly common in the tropics and subtropics. The disease is noted in the countries of Asia and Africa (India, the countries of the former USSR, Japan, Korea and a number of others), as well as in Central and South America.
Leprosy is not a widespread disease, but, nevertheless, it affects approximately 11 million people worldwide (according to WHO). According to statistics, men are three times more likely to get leprosy, but if we take into account the age of those infected, then among children there is a higher susceptibility to microorganisms than among adults.
The infection is spread by a sick person. It can also be carried by armadillos and monkeys. Leprosy bacteria are found in soil and water, but the likelihood of infection through them is extremely low.
The population affected by leprosy depends largely on the economic status of the country. What matters is the level of sanitary and hygienic skills of people, their financial well-being.
The infection can spread in 2 ways:
Airborne way. Bacteria are shed when coughing, sneezing, or talking. At the same time, a lot of pathogenic microorganisms enter the air.
In violation of the integrity of the skin. An infection can be introduced when performing tattoos, or when bitten by insects that feed on blood.
The longer the contact with a sick person, the higher the risk of infection. Thus, the likelihood of infection increases if a person is in intimacy with a patient with leprosy, or lives next door to him. Although statistics indicate that even if there is a patient with leprosy in the family, then close relatives get sick no more often than in 12% of cases.
The incidence is high among children, as their defenses are not yet fully formed. It has been established that black men suffer from leprosy more often than women. Among white-skinned people, this trend is not observed.
If a person with leprosy lived in the apartment, then after his departure, disinfection of the premises is required.
Features of its implementation:
First of all, linen and dishes are disinfected, as well as those places where mucus and sputum secreted by a person can be located.
All objects are boiled in a 2% soda solution. You can also soak them for an hour in a 1% chloramine solution.
Walls and floors in a residential area are sprayed with chloramine at a concentration of 0,5%, or bleach at a concentration of 0,2%.
Leprosy classification
Depending on the type of course of the disease, leprosy is distinguished:
Tuberculoid.
Lepromatous.
Dimorphic (borderline) and undifferentiated.
Stages of development of the disease:
Stationary;
Progressive;
regressive;
Residual.
Causes of leprosy

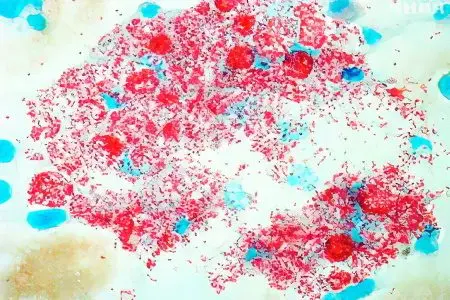
The causative agent of leprosy, Mycobacterium leprae, was discovered by Hansen in 1874. From the time of infection to the onset of the first symptoms of leprosy, it can take from two to 20 years, with an average of 3–10 years.
Mycobacterium leprosy (Mycobacterium leprae), considered the cause of leprosy, has much in common with Mycobacterium tuberculosis, but, unlike them, they are cultivated only on the skin of experimental animals and do not grow on nutrient media of artificial origin.
The bacterium looks like a stick, which has a straight or curved shape. Its ends are rounded. It does not exceed 7,0 µm in length and 0,5 µm in diameter. The bacterium is resistant to alcohol treatment. It is classified as an obligate intracellular parasite that invades tissue macrophages.
The source of the spread of bacteria is a person. It releases it into the environment. Pathogenic flora is present in breast milk, saliva, nasal mucus, urine, feces and semen, discharge from wounds. Mycobacterium enters the mucous membranes or damaged areas of the skin, and then reaches the nerve fibers, blood vessels. Together with the blood and lymph, pathogens spread throughout the body.
If a person is healthy, then he has immunity to bacteria and infection will not happen. At risk are children, people who abuse alcohol, patients with chronic diseases and those with weak immunity.
Symptoms of leprosy

The incubation period of the disease is quite long and ranges from 3 to 7 years, although sometimes it can be shortened to six months or stretched for 15-20 years. There is evidence that leprosy in the incubation period existed for 40 years. At the same time, no symptoms of the disease were observed in a person. Even after the leprosy has left the incubation period, the patient may not have any symptoms of infection for a long time.
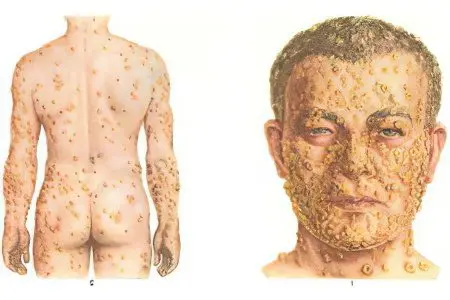
First of all, leprosy affects tissues that come into contact with air. Symptoms of leprosy are damage to the skin, mucous membranes of the mouth and sinuses, as well as nerves located on the surface. In advanced cases, leprosy penetrates into the deep layers of the skin and causes the destruction of nerve fibers, resulting in deformities, and the habitual appearance of a person is distorted.
The causative agents of leprosy are not the direct cause of the death of fingers on the limbs. If not treated in a timely manner, the infection leads to tissue necrosis on the arms and legs. Deprived of blood supply to the fingers, secondary infection quickly develops, which is caused by bacteria that enter the injured skin, thus, it is because of the bacterial infection that the fingers and toes eventually die.
There are two types of leprosy:
Leprosy of the tuberculoid type
Lepromatous form
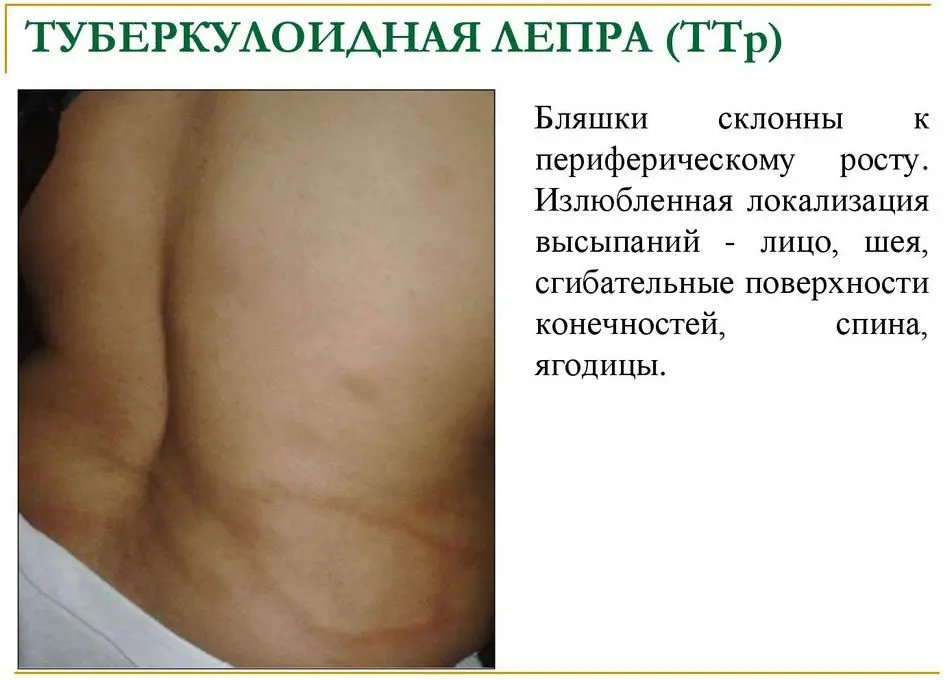
Tuberculoid leprosy
This infection has the most favorable prognosis. A person suffers from skin integuments, as well as nerve fibers passing along the periphery. Sometimes visceral internal organs are affected.
If the disease proceeds according to the tuberculin type, the symptoms of leprosy are flat spots with a red or white tint, or covered with scales. When the disease has just begun to develop, several spots resembling erythema are found on the dermis. Their boundaries are clearly defined. They grow rapidly and coalesce to form plaques that rise above the surface of the skin. In the affected areas of the skin, the sheaths of nerve fibers become denser, their thickening gradually leads to a loss of sensitivity of individual tissues. Then the plaque in the middle becomes dense, the dermis begins to atrophy. Over time, its dimensions reach 15 mm in diameter. Foci are multiple, can be found on the chest, on the lower back, on the back.
With this form of the disease, the nail plates suffer, they lose their natural color, begin to break, exfoliate and collapse. Nails become gray, stripes appear on them.
Neurological symptoms develop early. In those places where there are skin defects, sensitivity worsens, hair falls out, changes the color of the dermis, the glands responsible for the production of sebum and sweat are affected. The skin becomes dry, rough patches appear on them. When the disease has just begun to develop, skin sensitivity either decreases or increases for a short period of time. Then it decreases and disappears completely.
In the case when pathogens penetrate into large nerve trunks, destructive changes in bones and joints occur, most often the limbs suffer. A person hardly begins to move his fingers, contractures appear. Trophic ulcerative defects are formed on the legs. In the future, the fingers, hands and nose atrophy and are rejected. This process is called mutation.
If the facial nerve suffers, then the facial muscles stop moving, the eyelids do not completely close.
In medicine, cases of spontaneous disappearance of symptoms of tuberculin-type leprosy are known.
Leprosy of the lepromatous form
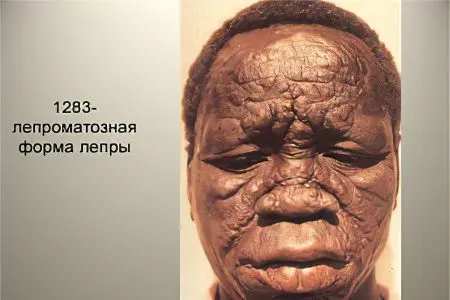
In this form, mycobacteria multiply rapidly in the skin and cause the formation of nodes (leprosy) or plaques with a characteristic scaly structure. Over time, the skin becomes thicker, deep folds appear on it. Most often they can be seen on the patient’s face, which resembles a lion’s face – a symptom characteristic of leprosy.
This disease has a severe course. First of all, the skin of the patient suffers, as well as the mucous membranes. After that, the pathological process spreads to the internal organs and the nervous system.
The main symptoms of lepromatous form of leprosy:
Skin lesion. Symmetrically located spots appear on the skin, which look like erythromatous rashes. In each such spot, a huge amount of mycobacterium leprosy is concentrated. The spots do not have clear outlines. They can appear on the palms, face, legs, buttocks and forearms. At first, the spots have a glossy sheen, from above they are smooth. As the pathology progresses, the spots turn from red to rusty or brown. At the same time, there is no deterioration in sensitivity in the area of their concentration. In this form, stains can persist for many years. Sometimes they disappear, and sometimes they transform into lepromas and infiltrates. In the latter case, the spots look like plaques without a clear limit. If vascular paresis occurs, the spots become brown in color.
Loss of function of the skin. If skin infiltration occurs, the sebaceous glands begin to work in an enhanced mode. Therefore, the dermis becomes greasy, acquires shine. The follicles of vellus hair, the ducts of the sweat glands become wider. Therefore, the skin resembles the appearance of an orange peel. As the pathology progresses, sweat ceases to be released in the area of infiltrate formation. First, vellus hair stops growing, and then a person’s mustache, beard and eyebrows begin to fall out.
Facial injury. The face with the infiltrates that appeared on it begins to resemble a “lion’s face”. All skin folds and wrinkles deepen, the superciliary arches protrude forward, the nose and cheeks become thicker, the lips and chin are divided into lobules.
Formation of leprosy. When the disease has just begun to develop, infiltrates form on the skin of the patient. They are not on the scalp, on the eyelids, in the area of the elbows and in the armpits. Then, at the site of infiltrates, lepromas are formed, which can reach a size of 3 cm. There are especially many of them on the face, on the ears, on the hands, in the forearms, on the shins, on the back and on the buttocks. Lepromas do not hurt, have a smooth surface, and can peel off. Most often, over time, lepromas become soft, but sometimes, on the contrary, they harden. It happens that they dissolve on their own. After them, a depigmented spot remains on the skin, which slightly sinks inward. If a person does not receive proper therapy, then ulcers form on lepromas, which hurt a lot. After their disappearance, scars remain on the skin.
Mucosal damage. The nasal mucosa is especially often affected. If the disease has a severe course, then the damage affects the oral cavity, lips and tongue. The patient has nosebleeds, nasal breathing worsens, as lepromas begin to grow in the nasal cavity. The organ itself is deformed. Sometimes a person loses the ability to speak. This happens when the disease affects the vocal cords.
Other symptoms. In addition to the symptoms of the disease described above, a person’s organs of vision may suffer. Keratitis, blepharitis, iridocyclitis, clouding of the lens, conjunctivitis are often diagnosed. The pathological process may involve nerve fibers, lymph nodes, blood vessels, testicles and liver. As the disease progresses, a person develops paralysis and paresis, and trophic ulcers form. When the liver suffers, the patient is diagnosed with chronic hepatitis. Men can develop orchitis and orchiepididymitis. In the future, the patient’s mammary glands begin to increase in size according to the female type, symptoms of infantilism develop, which is associated with hormonal imbalance.
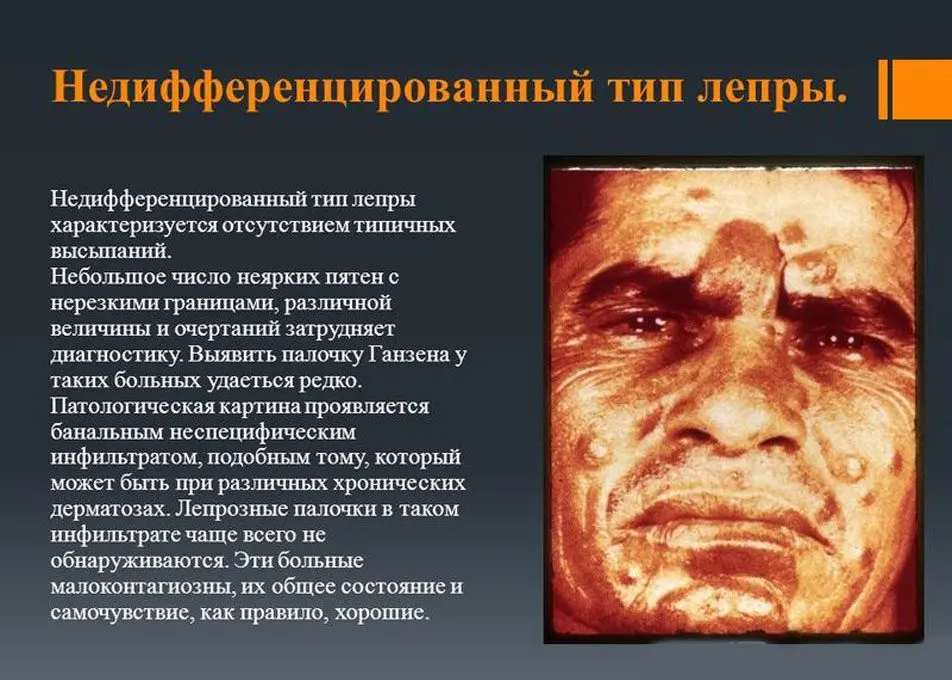
Leprosy of dimorphic and undifferentiated type
If a patient develops a dimorphic type of leprosy, then the clinical picture will combine the symptoms of tuberculoid and lepromatous varieties of leprosy.
The undifferentiated form of the disease may be accompanied by damage to nerve fibers. First of all, the peroneal, ear and ulnar nerve suffer. On the skin of patients, areas with altered pigmentation appear, in these places sensitivity decreases or completely disappears, sweat glands stop working. The more affected the nerve fibers, the more intense the symptoms of polyneuritis. Patients often experience paralysis and paresis, and deformities of the arms and legs may occur. They appear areas of ulceration that do not heal for a long time.
Diagnosis of leprosy

You can suspect the disease based on its manifestations. When leprosy is at an advanced stage, the diagnosis will be obvious to the doctor. Patients have no eyebrows, lepromas form on the body and on the face, limbs are paralyzed, fingers and hands may be missing, the nose is severely deformed, etc.
If the disease has just begun to develop, then the absence of obvious symptoms of leprosy can be difficult in terms of making a correct diagnosis. In this case, the patient can be referred for a consultation with a neurologist, dermatologist, infectious disease specialist or other specialist, since the manifestations of the disease are quite diverse.
To confirm leprosy, it will be necessary to conduct a bacteriological examination of scrapings taken from the fingers, from the earlobes, from the nasal mucosa. For histological analysis, lepromas, the contents of the lymph nodes, or discharge from ulceration sites can be taken. Mycobacterium leprosy will be found in the collected materials.
To clarify the degree of loss of skin sensitivity, functional tests are performed. They are carried out with Minor’s reagent, with nicotinic acid, with mustard and with histamine.
The lepromine test is also used. If his reaction is positive, then the patient develops leprosy according to the tuberculoid type, and if it is negative, then a lepromatous or borderline form can be diagnosed. When the test gives a weak positive reaction, then an undifferentiated variant of the disease is suspected.
Treatment of leprosy
For several centuries, leprosy was treated with haulmoogra oil, which was replaced by sulfone preparations. Diaphenylsulfone (dapsone) has been the main treatment for leprosy since the 1950s. Its therapeutic effect can be seen only after a long period of time. Not being a specific treatment for leprosy, sulfonic drugs inhibit the development of the disease. In mild cases, recovery occurs after two years, in more severe cases, treatment of leprosy takes about eight years.
With the emergence in the 1980s of strains resistant to the main treatment for leprosy, dapsone, complex regimens entered medical practice. Clofazimine is currently widely used in the lepromatous type of leprosy.
Today, leprosy is a curable disease. At the same time, it is important to identify it at an early stage of development, before it leads to disability. A sick person is placed in a leprosarium, or treated at home.
Now only those people who have pronounced skin defects are hospitalized. Inpatient treatment for primary therapy is also indicated. Hospitalize patients with relapse of leprosy. People who have a negative bacteriological test and have few skin rashes can be treated at home.
Patients are prescribed immediately 2 or 3 drugs that have pathological activity against leprosy bacteria. Be sure to carry out therapy aimed at increasing immunity.
Drugs are prescribed for up to six months. If a person tolerates treatment well, then there are no breaks between courses. The patient is prescribed one drug from the sulfonic series and two antibiotics. So that bacteria do not develop resistance, drugs must be alternated every 2 courses. In general, therapy should last at least a year, and sometimes it takes about 3 years. Some patients require lifelong treatment.
If a patient is diagnosed with multibacillary leprosy, then he is prescribed Rifampicin, Dapsone and Clofasamine. Drugs are released to patients free of charge.
Treatment Scheme:
600 mg Rifampicin + 300 mg Clofazimine orally once a month under medical supervision. At home, a person should take Dapsone 1 mg + Clofazimine 100 mg once a day. The course of therapy lasts a year. These recommendations are provided by the WHO.
In America, the treatment regimen is somewhat different. There, patients are offered 600 mg of Rifampicin + 100 mg of Dapsone + 100 mg of Clofazimine 1 time per day. The course lasts a year. If a person is diagnosed with a borderline form of the disease, then he is prescribed Dapsone for 10 years. In the lepromatous form of leprosy, this drug will need to be taken for life.
If a person is diagnosed with oligobacillary leprosy, then WHO recommends that such patients take 600 mg of Rifampicin once a month and 1 mg of Dapsone every day. The course of treatment according to this scheme lasts 100 months. If the patient has a single skin lesion, then he is offered a single dose of Ofloxacin 6 mg + Rifampicin 400 mg + Myocycline 600 mg.
In America, patients are prescribed 600 mg of Rifampicin + 100 mg of Dapsone once a day. The course of therapy lasts a year. If a patient is diagnosed with an indeterminate or tuberculoid form of leprosy, then he is prescribed Dapsone for 1 years. With a borderline form of the disease, the drug will need to be drunk for 3 years.
Dapsone is an inexpensive and safe drug used to treat leprosy. Occasionally, patients develop hemolysis and mild anemia, allergic dermatosis. The last complication can be severe. Dapsone’s syndrome develops even more rarely.
Rifampicin is even more active against leprosy bacteria than Dapsone. However, treatment with its use is more expensive. Side effects include: liver damage, flu-like syndrome, thrombocytopenia, renal failure.
Clofazimine is a safe drug. Its only side effect is a change in skin color, but after completion of the course of therapy, the color of the dermis is restored.
If the patient develops mild skin erythema (first or second episode of inflammation), then Aspirin is offered to patients. In severe erythema, prednisone 40-60 mg is prescribed once a day. Complement antibiotic treatment. When the skin lesion occurs again, then patients are shown taking Thalidomide 1-100 mg 300 time per day. However, this drug is prohibited for women who are planning a pregnancy. Its side effects are leukopenia and constipation.
Antibacterial agents are able to stop the progression of the disease, they do not allow to get rid of deformities that have already appeared, or to correct existing damage to nerve fibers. Therefore, it is so important to start treatment in the early stages of the disease. The drugs are used in a complex scheme, since mycobacteria leprosy are able to quickly develop resistance to one antibiotic.
Answers to popular questions
What is the prognosis for leprosy? If a person at an early stage of the development of the disease begins to receive treatment, then the prognosis is favorable. When leprosy has an advanced form, there is a high probability that the patient will become disabled.
Are there leper colonies in Russia? Yes, there are 4 leper colonies in Russia, which are located in Astrakhan, Krasnodar Territory, Stavropol Territory and Sergiev Posad. Sick people in leper colonies have their own houses, they run the household. Doctors live next to the leper colony.
After recovery, already formed deformities are reversible? No, if a person has lost hands or fingers, they will not grow back. Treatment aims to eliminate the leprosy bacteria in the body. To cope with paralysis, paresis and contractures, the patient is recommended physiotherapy, exercise therapy, sometimes surgery is performed.
What are the complications of leprosy? The main complications include: trophic ulcers, damage to the organs of vision with the development of complete blindness, loss of voice, nose deformity, loss of fingers, paralysis. If therapy is absent, then the person dies from cachexia, asphyxia or amyloidosis.
Can you get vaccinated against leprosy? What are the measures to prevent the disease? There is no vaccine for leprosy. There is evidence that staging BCG significantly reduces the likelihood of infection with mycobacterium leprosy. To prevent infection, you need to support the immune system, and also not to contact sick people. If a person with leprosy lives in a family, then he should have his own personal belongings, from a comb to utensils. All family members should be regularly examined for the detection of mycobacterium leprosy in their body, and carefully observe the rules of personal hygiene.
Which doctor treats leprosy?
Procoasis is treated by a phthisiatrician









