Contents

The cornea of the eye is one of the most vulnerable structural elements of the organ of vision. The cornea is affected by light, ambient temperature and a number of other factors. Sometimes the cornea is attacked by pathogenic flora. There are also mechanical damages. Therefore, keratitis, that is, inflammation of the cornea, is often diagnosed by ophthalmologists.
Symptoms of keratitis are discomfort in the eyes, the appearance of ulcerative defects on their mucous membrane. A person has photophobia, lacrimation intensifies. If there is no treatment, then severe complications can develop, up to blindness and the formation of a thorn. Therefore, treatment of keratitis should be started immediately.
What is keratitis?
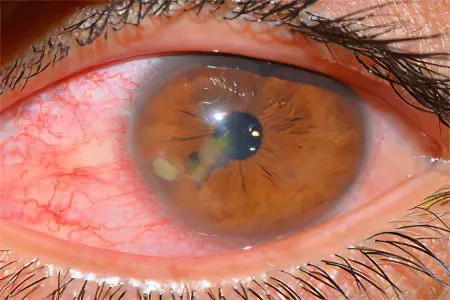
Keratitis is an inflammation of the cornea of the eye. Due to this pathological process, clouding of the cornea occurs. The eyeball itself often acquires a red color, which is due to the expansion of the vessels of the perilimbal region.
Often the cause of keratitis is an inflammatory process, such as conjunctivitis or blepharitis. Bacteria affect the cornea, including representatives of the coccal flora, amoeba, Pseudomonas aeruginosa, etc. The viral and fungal nature of keratitis cannot be ruled out. However, mycotic organisms lead to inflammation of the cornea less frequently than the rest of the pathogenic flora.
People who use contact lenses are prone to keratitis. Such persons need to be especially attentive to the observance of the rules of personal eye hygiene.
If there is no treatment for keratitis, then a thorn forms in the affected area, which causes visual impairment. When therapy is timely and implemented in full, the prognosis is favorable. Most often it is possible to achieve a complete recovery. However, with long-term keratitis, irreversible loss of vision, up to complete blindness, can occur.
Causes of keratitis

The causes that can provoke keratitis can be very diverse. They are divided into internal and external. Most often, it is not difficult to determine them; idiopathic keratitis is rarely diagnosed.
External causes that can lead to the development of keratitis include:
Mechanical eye injury.
Chemical damage to the eyeball.
Thermal injury.
Previous eye infections, such as syphilitic or tuberculous keratitis.
Fungal infection of the cornea.
Bacterial infections, which are most often caused by staphylococci and Pseudomonas aeruginosa.
Wearing contact lenses.
Excessive influence of ultraviolet radiation on the cornea of the eye.
The internal causes that lead to the development of keratitis include:
Damage to the nervous system with deterioration of the innervation of the organs of vision.
Deficiency of vitamins in the body.
Allergy.
Viral infections. This refers to herpes that a person was infected with.
Metabolic disruptions.
Conjunctivitis and diseases of the eyelids.
Erosion of the cornea.
Lagophthalmos, which consists in incomplete closing of the eyelids.
Systemic diseases, in particular, diabetes, rheumatism and gout.
Rarely, the cause of keratitis cannot be determined.
Classification of keratitis

Depending on the cause of inflammation of the cornea, there are the following types of keratitis:
Exogenous keratitis, which develop under the influence of external factors:
Traumatic inflammation. It may be due to physical, mechanical or chemical trauma.
Purulent inflammation that develops due to damage to the cornea by bacteria, fungi or viruses.
Keratitis that occurs against the background of inflammation of the meibomian glands, or against the background of diseases of the conjunctiva.
Endogenous keratitis, which develop for internal reasons:
Infectious keratitis provoked by the herpes virus, mycobacterium tuberculosis, brucellosis, malaria or leprosy.
Non-infectious keratitis, which develops against the background of a systemic lesion of connective tissues.
Neuroparalytic keratitis.
Hypo- and avitaminous keratitis associated with a lack of vitamins in the body.
Allergic keratitis, which is caused by an allergic reaction of the body.
Keratitis with an unexplained etiological factor. These include keratitis rosacea, filamentous keratitis, and corneal ulcer.
Depending on the symptoms of inflammation of the cornea, there are such types of keratitis as:
Nonpurulent.
Purulent.
Catarrhal.
Depending on the location of the inflammation, keratitis can be:
Superficial. In this case, only the corneal membrane, its epithelium, or the anterior plate, which is also called the Bowman’s membrane, will be affected.
Deep. This type of keratitis is also called stromal. At the same time, the entire stroma of the cornea, its posterior membrane and internal endothelium are involved in the process of inflammation.
Depending on the nature of the course of inflammation, keratitis can be:
Chronic.
Subacute.
Sharp.
Depending on the method of accumulation of the inflammatory infiltrate, there are such types of keratitis as:
Central keratitis. In this case, fluid accumulates at the pupil.
Paracentral keratitis, when the exudate is localized opposite the iris.
Peripheral keratitis, when the inflammatory fluid is concentrated at the limbus.
The symptom is keratitis

Symptoms of keratitis will appear the brighter, the more intense the inflammation of the cornea. The pathogenic flora that provoked the development of the disease is also important.
The first symptoms of keratitis include:
Redness of the eyes.
Pain in the organs of vision.
Lachrymation.
The main manifestations of the disease include:
The cornea swells, becomes cloudy.
The eyes lose their specularity.
A person cannot look at the light, it enhances the manifestation of the symptoms of the disease.
Eyes hurt.
Vision is deteriorating.
Blepharospasm develops, which manifests itself in involuntary twitching of the eye muscles.
The vessels in the eyes swell, so the organs of vision will be pierced by enlarged capillaries.
The cornea of the eye loses its former sensitivity.
An infiltrate appears on the cornea. Its color will depend on how the inflammatory exudate is represented. If it is purulent, then the color will be yellow, and if it contains predominantly lymphoid cells, then the color of the infiltrate is grayish.
When an infiltrate accumulates on the cornea, the patient will feel that he has a foreign object in his eye.
The infiltrate can have not only a different color, but also a different location and shape. With significant inflammation, it occupies most of the eye. Sometimes erosion occurs at the site of the infiltrate. It also tends to fall off the cornea.
Separate forms of keratitis

Traumatic keratitis. They occur due to damage to the cornea of uXNUMXbuXNUMXbthe eye.
bacterial keratitis. If the bacteria were brought into the cornea from the outside, then keratitis will develop as a creeping ulcer. In a patient, a defect is formed on the cornea, which has undermined edges. If a person does not receive treatment, the wound grows rapidly. When keratitis develops against the background of syphilis or tuberculosis, the corneal stroma suffers, with its deep vascularization. The overgrown vessels look like brushes.
Viral keratitis. The disease develops against the background of damage to the body with herpes simplex or herpes zoster. The cornea is covered with bubbles or branches. If keratitis has a severe course, then the cornea becomes cloudy, large infiltrates form in it.
Fungal keratitis. With this type of inflammation, the infiltrate will have a white color, it is loose, uneven, with torn edges. Candida, aspergillus, Fusarium fungi are capable of provoking mycotic keratitis.
Allergic keratitis. Symptoms such as lacrimation, itching, redness of the eyes come to the fore. They appear after interaction with the allergen.
Nitric keratitis. Pathology develops with a deficiency of lacrimal fluid. The cornea of the eye becomes very dry, its cells die.
Acanthamoeba keratitis. This type of inflammation occurs due to amoebas that infect the lining of the eye.
Creeping ulcer of the cornea. This type of keratitis is the result of a sharp foreign object entering the organs of vision. The disease is complicated by suppuration.
Phlyctenular keratitis. This disease is a companion of patients with tuberculosis. Inflammation will be concentrated in the place where the vessels of the cornea and sclera merge.
Photokeratitis. The cornea suffers due to damage from ultraviolet rays. This happens when working with a welding machine, or during a long pastime in the sun.
parenchymal keratitis. This keratitis is due to congenital syphilis. The disease can be transmitted through several generations. Persons under 20 years of age suffer from it. Both eyes are inflamed at the same time. The main symptom of the lesion is significant redness.
Neutrophic keratitis. Inflammation can be provoked by an injury to the trigeminal nerve, or an infection that has entered the eye. In addition to inflammation, dystrophic changes in the organs of vision are observed.
Rosacea-keratitis. This disease manifests itself in older people who suffer from facial rosacea. To date, the causes of the development of the disease remain unclear.
Diagnosis of keratitis
To make a diagnosis to a doctor, most often a standard examination is sufficient. Typical symptoms of keratitis allow you to determine the inflammation of the cornea.
The doctor performs an anamnesis, clarifies with the patient what conditions preceded the development of the disease. It is important to clarify whether there has been an injury or other damage to the organ of vision. The doctor then examines the patient.
The main diagnostic methods include:
Visiometry. The doctor evaluates the function of vision using special tables.
fluorescent method. It makes it possible to understand whether the integrity of the cornea is not broken.
Analgesimetry allows you to check pain sensitivity.
Ophthalmoscopy. During the study, the doctor assesses the condition of the eye and fundus, retina, blood vessels, optic nerve. The procedure is carried out on a special device – an ophthalmoscope.
Biomicroscopy. The study is carried out using special equipment. The doctor examines the organ of vision using a slit lamp. It makes it possible to detect even small damage to the eyeball.
Microscopy. During the procedure, a scraping is taken from a person. Its study allows you to determine the type of pathogenic flora that provoked inflammation.
To clarify the nature of keratitis, a whole range of laboratory studies will be required. These include: conjunctival cytology, fluorescent antibody method. Among the serological methods, the most popular are:
RSK.
Neutralization reaction.
Nephelometry with various allergens (viral, bacterial, medicinal, tissue).
Tests are also carried out with tuberculin, herpetic vaccine, brucellin and other antigens.
Treatment of keratitis

After the cause of the development of keratitis is clarified, the doctor prescribes treatment for the patient. In the absence of complications of the disease, therapy is carried out at home. If the organs of vision are significantly affected, then hospitalization is required.
The main directions of treatment of keratitis:
Getting rid of infection.
Stimulation of tissue repair.
Eliminate the symptoms of iridocyclitis.
Dissolving therapy.
To cope with keratitis is most often possible with the help of conservative therapy.
Medical correction involves the implementation of the following methods:
Getting rid of pain occurs with the use of local anesthetics (Diftal).
When keratitis develops due to wearing lenses, or due to their misuse, eye gels are shown to the patient. They allow you to restore and moisturize the mucous membranes.
Using moisturizing drops. They are used for malfunctions in the functioning of the eye glands.
The use of antihistamines is indicated when the inflammation is of an allergic nature. These drugs are used in the form of drops, injections and tablets.
Preparations for the destruction of bacteria: Tobrex, Levomycetin, Floksal, Tsipromed. If treatment with local remedies is not effective, then the tablets are prescribed orally, or injections of antibiotics are given.
Preparations for the destruction of viruses: drops of Ophthalmoferon, Interferon, Zirgan, Zovirax, idoxuridine solution. They are used for herpetic and adenovirus keratitis.
With syphilitic lesions of the cornea, special antibiotics are used, as well as preparations for intramuscular injection. The patient will have to be observed not only by an ophthalmologist, but also by a venereologist.
To dilate the pupil, mydriatics are used: Atropine, Tropicamide, Cyclomed. These drugs are needed in order to prevent the formation of adhesions between the iris and pupil.
Corticosteroids, such as hydrocortisone or dexamethasone. These drugs can relieve swelling and inflammation from the eyes.
Preparations that accelerate the recovery processes in tissues: Korneregel, Actovegin.
When keratitis develops due to a foreign object entering the organs of vision, you need to get rid of it. Then the doctor assesses the degree of damage to the cornea and only then prescribes treatment.
To increase the effectiveness of therapy, the doctor directs the patient to undergo physiotherapy techniques. It can be phonophoresis, magnetotherapy, electrophoresis.
Surgery
The operation is indicated for patients who have an ulcerative defect on the cornea.
The intervention is implemented using modern equipment:
Laser treatment, namely laser coagulation.
Cold treatment, namely cryoapplication.
Replacement of part of the cornea with a graft. Such an operation is performed when the damaged area of the eye has been replaced by scar tissue.
If the disease has a severe course and it was not possible to cope with inflammation by all of the above methods, then the patient is shown the removal of the eyeball.









