Paresis of the intestine or paralytic ileus is a serious transient disorder of the intestinal motility. This disease is often diagnosed after certain surgical manipulations on the intestines, when the water-electrolyte balance is disturbed. Intestinal paresis often manifests itself on the second or third day after surgery. The patient may develop intoxication of the body.
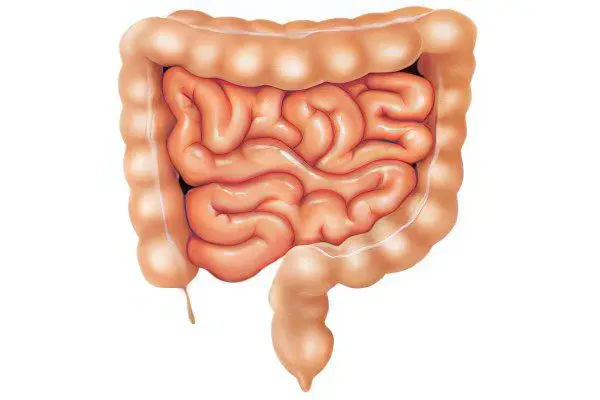
Often with paresis of the intestine, a significant expansion of the stomach can be observed. Paresis can be localized in one place of the gastrointestinal tract or it can capture all its departments. There are many factors that have become a progressive basis for the development of this disease. Among them are many diseases and pathological conditions of the human body. It can be peritonitis, various tumors, hematomas, as well as inflammation in the intestines.
Intestinal paralytic obstruction can occur due to a dangerous urolithiasis or a specific injury to the peritoneum. People who have had myocardial infarction and pleuropneumonia also become possible hostages of this disease.
Patients with metabolic disorders due to a lack of potassium and magnesium, as well as other patients who have undergone poisoning with pesticides, can also develop intestinal paresis. Diabetes, mesenteric thrombosis, and embolism are precursors to paralytic ileus. Intestinal paresis can manifest itself with unhealthy kidneys or dangerous lung diseases. It can be myocardial infarction, pneumonia, as well as various fractures of the ribs.
This disease is characterized by impaired motility of the stomach and colon after operations on the organs of the gastrointestinal tract. A significant recovery process in the colon can take three days. The functioning of the small intestine is rarely completely disrupted. It usually takes several hours to restore her motor skills after the operation.
There are three main stages in the development of intestinal paresis. The first stage is characterized by inhibition of peristalsis, at this stage paralytic ileus occurs. The second stage is characterized by intestinal stasis, when the intra-intestinal pressure increases significantly due to the accumulation of gas and fluid in the intestinal lumen. The third stage is marked by progressive intoxication and severe disruption of the work of all human organs and systems.
What is characteristic of intestinal paresis?
With intestinal paresis, the patient has severe pain and noticeable bloating. The patient may have vomiting, and the absence of stools and gases is not excluded. In some cases, you may notice an uncontrolled release of watery stools. Significant pain sensations spread throughout the intestines, while the pain does not radiate to neighboring organs and is always bursting in nature, there is no peristalsis.
A person has frequent vomiting of the contents of the stomach and intestines. Vomit may be mixed with blood, this often indicates the onset of bleeding from the walls of the stomach and intestines or the presence of acute ulcers. In a patient, due to a strongly swollen abdomen, breathing passes into the chest. Tachycardia is diagnosed and, along with this, a significant decrease in blood pressure. Many patients complain of a strong feeling of thirst.
How to treat intestinal paresis?
The main therapy for intestinal paresis consists in constant naso-gastric aspiration (suction of the contents through a tube), the absolute exclusion of food and liquid intake through the oral cavity, intravenous transfusion, the sparing prescription of psychotropic sedatives, and also in the rejection of opiates.
If this dangerous disease does not stop within a week, then the cause of intestinal paresis may be mechanical in nature. In this case, the patient may be prescribed a laparotomy.
The dynamics of the development of paresis and its transition to acute intestinal obstruction determine the course of treatment. Surgical intervention must be carried out with extreme caution, guided by modern principles of gentle technology, then it will be possible to avoid the dangerous occurrence of postoperative paresis. If the risk of developing paresis is quite high (acute pancreatitis, severe injuries of the abdomen and lumbar), then it is necessary to perform the necessary nasogastric aspiration.
In addition, it is necessary to use a special method of regional shutdown of sympathetic innervation using novocaine. Therapeutic measures for intestinal paresis include various ways of stimulating intestinal motility. For example, a special massage of the abdominal wall or various kinds of compresses. With the help of unique therapeutic enemas and artificial irritation of the rectum with a gas outlet tube, it is also possible to effectively activate the patient’s intestinal motility.
If a patient is diagnosed with volvulus, then drugs and intestinal stimulation will not help here. In this case, an urgent operation is necessary. Surgical intervention should be performed as quickly as possible, because the paralyzed part of the intestine, without receiving the necessary amount of blood, can atrophy.









