Contents
- What is an intervertebral hernia?
- What you need to know about intervertebral hernia?
- What is the structure of the spine and intervertebral discs?
- Symptoms of an intervertebral hernia
- Pain in the intervertebral hernia
- Relationship between intervertebral hernia and osteochondrosis
- What are the causes?
- Stage of the disease
- Complications and consequences
- Diagnosis of the disease
- Is treatment possible without surgery?
- Surgery
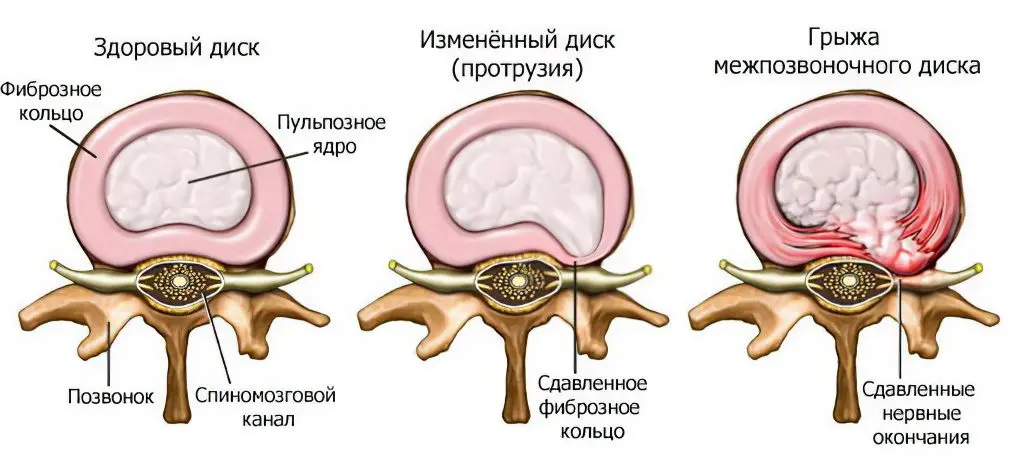
What is an intervertebral hernia?
Intervertebral hernia is a protrusion of the nucleus of the intervertebral disc into the spinal canal as a result of a violation of the integrity of the fibrous ring. It is an inflammatory and degenerative disease that leads to deformation of the intervertebral disc, rupture of the fibrous ring and the exit of the nucleus outside the vertebral body.
In general, this is a relatively rare pathology. According to statistics, it occurs in no more than 0,15% of the world’s population (or about 15 people per 10). However, over the past five years, the incidence has increased significantly (almost 000 times).
The greatest load is on the lumbosacral spine, so it is obvious that it is he who undergoes pathological changes in the first place. About 48% of hernias develop at the level between the fifth vertebra and the sacrum, the disc between the fourth and fifth vertebrae suffers somewhat less frequently (46%).
Hernias located in the cervical spine are much less common, and cases of damage to the thoracic spine are rare.
According to medical statistics, a hernia at one stage or another in most cases causes back pain.
In the leading countries in terms of medical care, from 20 (Germany) to 200 (USA) thousand surgical interventions are performed annually to eliminate a herniated disc.
What you need to know about intervertebral hernia?

Intervertebral discs are a kind of shock absorbers that reduce the impact of the vertebrae on each other when they move and the spine moves.
The nucleus pulposus of the central part of the disc, which has a gel-like consistency, is protected by a hard shell – the fibrous ring.
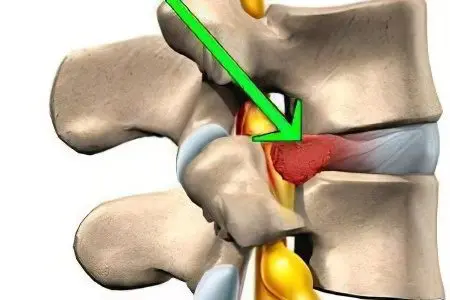
When a crack or rupture occurs in the annulus fibrosus, part of the vertebral nucleus pulposus is squeezed out into the pulpal canal.
Volume intervertebral hernia compresses the spinal nerves located in the same segment of the spine.
Examination of the patient by a neurologist, MRI diagnostics will help determine the volume and features of the pathology.
Most often, conservative therapy of intervertebral hernia is practiced: massage, a complex of therapeutic exercises, traction of the spine with the help of special devices. Surgery is rarely performed.
Surgical treatment is not able to eliminate the cause of the herniated discs, it is used to eliminate serious complications that threaten the patient’s quality of life. Surgery is fraught with irreversible consequences.
What is the structure of the spine and intervertebral discs?
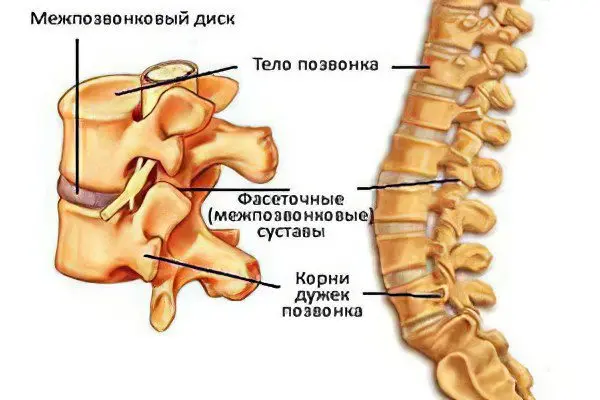
Intervertebral discs are located between the vertebral bodies. The body is the largest part of the spine.
Sections of the spine:
Cervical – 7 cervical vertebrae;
Thoracic – 12 thoracic vertebrae;
Lumbar – 5 lumbar vertebrae;
The sacral region, which passes into the coccyx, is located under the fifth lumbar vertebra.
The spine is a single whole, at the same time being a mobile structure. The most important functions of the spine are supporting the skeleton, protecting the spinal cord located in the spinal canal from damage. Protection from injury is provided by the spinous processes – bony protrusions located behind the spinal cord. The bony body of the vertebra, due to its shape and size, is a kind of platform that softens the load on the spine.
Intervertebral discs are a special structure located between the vertebral bodies. They cushion the pressure experienced by the spinal column during human movements. The structure of all discs is the same for each segment – it is a gel-like nucleus pulposus in the center, surrounded by a solid ring of fibrous tissue. Fibrous rings perform a binding function, connecting the vertebrae to each other. If the fibrous ligaments are damaged due to the destruction or degeneration of the intervertebral disc, the patient feels pronounced pain.
Symptoms of an intervertebral hernia

An intervertebral hernia can theoretically affect absolutely any part of the spine, while the symptoms will vary significantly.
Consider the symptoms of an intervertebral hernia, depending on its location:
Neck department:
Frequent and intense headaches. Headache of unclear localization, throbbing, pressing or arching. The reason lies in the compression of the nerve roots, as well as the vertebral arteries that feed the brain. As a result, serious vertebrobasilar insufficiency with characteristic manifestations may develop.
Dizziness. Due to compression of the vertebral arteries, the cerebellum receives insufficient nutrition.
Visual hallucinations (photopsies, scotomas). Visual disturbances are explained by a lack of blood circulation in the visual center.
Weakness, drowsiness and fatigue. When squeezing the vertebral arteries, the brain receives less oxygen and nutrients. As a result, the body is forced to work less intensively and give a command to all systems to reduce activity.
Pain in the neck. Caused by compression of nerve endings.
Instability of blood pressure. Patients often have false hypertension. The reason is that there are many blood vessels in the neck area. They are abundantly innervated, pinching these blood lines leads to the fact that the brain receives false signals and triggers reflexes, leading to an increase in blood pressure.
There is radiating pain in the shoulder or forearm.
Muscle weakness (shoulders, arms).
Numbness of fingers. Feeling of “running”.
Pale skin, sweating.
Thoracic:
Backache. Localization of pain – at the level of the shoulder blades. Girdle pain, aggravated by physical exertion, coughing, sneezing, deep breathing. They can radiate to the arms, abdomen, neck, lower back, shoulders.
Abdominal pain rarely occurs. It is important to exclude other diseases.
Decreased sensitivity below the lesion. Paresis and paralysis develop. This is due to compression of the spinal cord.
Lumbar:

Acute pain in the lumbar region (lumbago or lumbago). The pain comes on suddenly. It is usually associated with physical activity, weight lifting. It has a sharp, shooting, burning character. The reason lies in the prolapse of the intervertebral disc and irritation of the nerve roots located in the area of the fibrous ring. As a result, a reflex increase in muscle tone occurs and a persistent pain syndrome develops with the inability to change the posture. Most often, this symptom occurs in sick men aged 30 to 40 years.
Ishalgia (sciatica). It is a pronounced pain syndrome associated with the pressure of a hernia on the roots of the spinal cord. Compression of the nerve endings leads to irritation of the large sciatic nerve. This explains such a pronounced pain syndrome. The pains are stabbing, shooting, aching. Often the pain radiates from the site of the lesion down the back of the leg to the thighs, calves, and ankles. As a rule, pain covers one of the legs, depending on the location of the hernia.
Prolonged pain in the lumbar region. They can torment a person for months and years.
The defeat of the motor nerves, which causes a decrease in the tone of the muscles of the legs.
Violation of the functions of organs located in the pelvic region. In severe cases, it is possible to develop urinary incontinence, uncontrolled defecation, impotence in men.
Compression of the nerves responsible for sensitivity. As a result, the sensitivity of the skin of the legs (groin, buttocks, thighs, shins, ankles) decreases, a tingling sensation, “goosebumps” develops.
Blood supply disorders. The reason is compression of the nerves that regulate blood circulation. As a result – pallor of the skin, the appearance of spots on the skin.
Spinal cord injury. It can manifest itself in the form of paresis, paralysis of the lower extremities.
Pain in the intervertebral hernia

The established opinion that the cause of pain in the spine is mechanical compression of the nerve roots has been replaced by the version of “chemical sciatica”. The main goal of surgical treatment is to eliminate the infringement of the spinal nerves. Recently, medical research data on such a cause of pain as chemical inflammation have been actively discussed.
The mediator of these painful sensations is the tumor necrosis factor (TNF) molecule, or tumor necrosis factor-alpha.
Causes of the inflammatory molecule:
Intervertebral hernia;
Fibrous ring fissures;
Narrowing of the spinal canal (spinal stenosis);
Pathology of the facet joints.
The consequences of the influence of the TNF molecule are the appearance of pain and inflammation. However, stopping the activity of the molecule with drugs does not eliminate the need to eliminate nerve root compression and treat herniated discs with traditional methods. An excellent alternative to the expensive and sometimes ineffective treatment of “chemical sciatica” can be hirudotherapy (treatment with leeches).
The most common localization of the intervertebral hernia is the cervical and lumbar spine. This pathology rarely affects the thoracic region. Hernias in the vast majority of cases occur in the posterolateral projection of the vertebra. In this part of the vertebrae, the effect of compression on the fibrous ring is most pronounced, and the support of the posterior and anterior longitudinal ligaments is least felt.
Relationship between intervertebral hernia and osteochondrosis

There is a proven connection between osteochondrosis and herniated discs. A natural consequence of poor-quality treatment of osteochondrosis is an intervertebral hernia. Diagnosis and treatment of varieties of osteochondrosis are similar to the diagnosis and treatment of similar cases of intervertebral hernia.
Prevention and treatment of osteochondrosis will lead to the elimination of intervertebral hernia, that is, both cause and effect are directly dependent on each other.
What are the causes?

The causes of hernia are numerous, among them there are several factors that significantly increase the risk of developing pathology:
Floor. According to studies, cartilage in men is less developed than in women and wears out much faster. Therefore, in the risk group, in the first place, are men.
Age. Over time, the elasticity of cartilage decreases, degenerative processes begin in the spine and joints. Women over 45 and men over 30 are at risk.
Past diseases, injuries and surgical interventions in the spine significantly increase the risk of developing intervertebral hernias.
There are also a number of subjective factors that a person can influence:
Overweight. A large amount of fat relationships contributes to an increased load on the spine. An obese person also has a decrease in muscle tone. Weakened muscles cannot create a reliable “corset” to support the spine. In addition, metabolic disorders lead to a decrease in the flexibility of the spinal column.
Bad habits. First up is smoking. Nicotine reduces the amount of nutrition of the intervertebral discs. As a result, the risk of developing pathology increases.
Physical inactivity. It has been proven that a sedentary lifestyle provokes the development of a pathological process.
The physical nature of the work. Constant lifting of weights, work in conditions of high vibration negatively affect the spine.
Heredity. From the ancestors, the features of metabolism and the genesis of cartilage tissue are transmitted. Therefore, if there were persons in the family suffering from such a pathology, the risk of its development in descendants increases in the range from 20 to 75%.
Stage of the disease

Any intervertebral hernia goes through four stages in its development:
Disk protrusion. A small gap is formed in the fibrous ring of the intervertebral disc. A fragment of the nucleus pulposus comes out. At this stage, you can cope with an intervertebral hernia on your own without special treatment. The doctor recommends strict bed rest. Physical activity, sudden movements are excluded. The fissure of the fibrous ring is gradually “tightened”, the pathological process stops. If the doctor’s recommendations are not followed, the hernia will progress. The pressure of the nucleus pulposus on the annulus fibrosus will increase until the disease progresses to another stage. At this stage, shooting pains are already manifested, the hernia reaches about 3 mm in size.
Partial disc prolapse. The protrusion of the nucleus pulposus increases. The hernia can reach 8-10 mm in size. The pains become persistent and pronounced. The blood supply to the intervertebral disc is reduced.
Complete disc prolapse. The nucleus pulposus extends beyond the fibrous ring, while maintaining its structure. The intensity of pain increases significantly. Pain sensations are shooting and aching in nature, practically do not disappear on their own without taking analgesics. Violated motor function, reduced ability to work. The pain radiates to the lower extremities.
Sequestration. Fragments of the nucleus pulposus fall out of the fibrous ring. The intervertebral disc is displaced. A hernia pinches the nerve roots, causing intense, prolonged pain.
Complications and consequences
Infringement of the intervertebral hernia. From the moment the protrusion is detected, it is necessary for the patient to follow the recommendations of the doctor. The most important of the recommendations is to minimize physical activity: exclude weight lifting, sports. If the recommendations of a specialist are not followed, there is a risk of infringement.
Infringement occurs by surrounding tissues (bone structures, muscles). When an intervertebral hernia is infringed, a deformation of the structure of the affected intervertebral disc occurs. As a result, pinching of the spinal roots and the development of pronounced symptoms are often observed. In the most severe cases, the hernia pinches the spinal cord, causing functional impairment.
As a rule, pinching occurs:
Nerve S1. The nerve is pinched not only in the lumbar, but also in the sacral spine.
Nerve L1. That is, the lumbar nerve between the fourth and fifth segments.
Protrusion It is a deepening pathological process of development of an intervertebral hernia. As the pathology develops, the nucleus pulposus puts more pressure on the annulus fibrosus. At a certain moment, the fibrous ring ruptures and the nucleus pulposus exits the structure. This complication is one of the most dangerous, because it is difficult to predict what consequences the development of a full-fledged hernia will entail. There are frequent cases of the development of a posterior hernia, in which the spinal cord is injured and the motor function is completely or partially lost below the site of the lesion.
Diagnosis of the disease

Diagnostic measures for intervertebral hernias include:
Primary medical examination;
CT (computed tomography);
MRI (magnetic resonance imaging);
radiography;
CT-myelography.
For an initial face-to-face appointment with an intervertebral hernia, you should go to an orthopedist or neurologist.
Doctor’s appointment

During the appointment, the doctor:
Questions the patient and finds out all the facts regarding complaints: the intensity of pain, their frequency and nature, localization, are there any other symptoms;
Conducts an initial examination and palpation of the back or neck (depending on the location of the hernia). The doctor assesses the condition of the spine, determines the stage of the pathological process;
Carries out an assessment of reflexes;
Assesses motor function, muscle strength, skin sensitivity below the affected area (usually the legs);
Carries out the necessary functional tests. The patient is asked to walk around the office, bend back and forth, raise his leg, tilt the body, etc.
Based on the initial examination, the doctor draws a conclusion about the patient’s state of health and develops a further examination strategy.
Computed tomography

Computed tomography is an effective and informative instrumental study. It is prescribed to patients with suspected intervertebral hernia and allows you to most accurately determine the condition of the intervertebral discs and the stage of development of the pathological process (if any).
Thanks to CT, it is possible to obtain x-ray layered images of the spine.
There are a number of relative contraindications to conducting a tomographic study:
Pregnancy, children under 5 years of age;
Severe condition of the patient;
Severe obesity (obese people weighing over 150 kg either do not fit into the scanner, or the table is not designed for such a weight);
Mentally unhealthy patients (with inappropriate behavior);
Patients suffering from fear of closed space (claustrophobia).
In case of urgent need, the study can be carried out, despite contraindications.
Although CT is highly informative, doctors prefer MRI because it is more suitable for assessing the condition of the intervertebral discs.
MRI

MRI is ideal for determining the condition of the intervertebral disc. On MRI images, the anatomical features of the spine are visible in all details.
An indication for examination is the presence of an unconfirmed intervertebral hernia.
There are a number of absolute contraindications to magnetic resonance imaging:
The presence of metal implants or foreign objects inside the body (since during the examination a magnetic field of enormous power is generated);
The presence of functional implants and prostheses that are sensitive to the level of the magnetic field: ear prostheses, pacemakers, pacemakers.
MRI has several undeniable advantages over computed tomography:
Safety – the patient’s body is not exposed to strong x-ray radiation;
The highest efficiency and information content of the diagnostic measure.
X-ray

Unlike tomographic research methods, radiography does not allow assessing the condition of the intervertebral discs. But it is prescribed to patients with a confirmed intervertebral hernia to exclude pathological changes in the vertebrae themselves.
For diagnostic purposes, a picture is taken in two projections: full face and profile.
There are a number of contraindications:
Severe condition of the patient;
Pregnancy;
Intense bleeding.
CT-myelography

The essence of the study is the introduction of a contrast agent into the area around the spinal cord, followed by computed tomography. The main task of the diagnostic measure is to assess the degree of compression of the spinal cord by a hernia. The method requires special skills and is characterized by a rather high complexity, therefore it is carried out only in a hospital setting.
There are two main indications for the study: compression of the spinal cord and impaired outflow of cerebrospinal fluid.
Contraindications are standard for computed tomography, however, individual intolerance to the components of the contrast agent is an additional obstacle.
Is treatment possible without surgery?
Conservative methods of treatment of intervertebral hernia are not as effective as surgical ones, they rather simply relieve pain, but do not have any pronounced effect. These include the use of NSAIDs and glucocorticoids, physiotherapy, homeosiniatry, laser therapy and other techniques.
Conservative methods
In the course of conservative therapy, drugs of two groups are used: non-steroidal anti-inflammatory drugs and topical drugs based on glucocorticoids.
Electrophoresis
The essence of the method is the introduction of drugs into the body through the action of an electric current. For the treatment of pathology, drugs such as papain and caripain are used.
These drugs reduce the protrusion of the hernia, promote the regeneration of damaged tissues and restore normal blood circulation in the area of the damaged disc.
Method of carrying out: two electrodes with different poles (plus and minus) are applied to the patient’s skin. A drug is applied to one of the electrodes, penetrating under the skin. The current parameters are adjusted based on the individual characteristics of the body, so that the patient feels a slight tingling sensation.
Session duration: 10-15 minutes.
A course of treatment: 10 days. The period may be extended at the discretion of the physician.
Indications: confirmed intervertebral hernia during remission (subacute period). It is important that there is no exacerbation.
Contraindications: oncological diseases, heart failure, local inflammatory and infectious processes, skin pathologies, violation of the integrity of blood vessels, elevated body temperature, skin injuries at the site of electrode application, intolerance to administered drugs.
Treatment of intervertebral hernia with a laser
Laser therapy is a relatively new and little known method. In recent years, it has become more and more widespread and gains well-deserved popularity. Its essence is as follows: an endoscope with a built-in needle is inserted into the lesion site. A cable with a laser diode and a built-in video camera is pulled through the lumen of the needle. During irradiation, tissues are heated up to 70 °C. The surrounding tissues are not destroyed, however, the substance of the nucleus pulposus gradually evaporates. As the core evaporates, it contracts and ceases to exert pressure on the surrounding tissues.
Over time, chondrocytes replace the destroyed tissues of the fibrous ring. In this way, it is possible to partially or completely cure the intervertebral hernia.
Surgery
Surgery is a last resort.
Therefore, there are several absolute indications for the operation:
Disorders of the pelvic organs caused by compression of the spinal cord: urinary and fecal incontinence, impotence;
Strong, prolonged pain syndrome against the background of ongoing conservative therapy;
Paralysis, paresis, movement disorders, disorders of muscle tone and sensitivity.
Often doctors insist on surgery even without prior conservative treatment. This is fundamentally wrong. In this way, clinics and doctors profit from patients. It is known that hernias tend to heal on their own, and this is confirmed by the data of numerous studies. For this reason, it is important to find a competent and honest specialist.
In order to cure the pathology, the following surgical methods are used:
Disc prosthetics. The damaged disc is removed completely, then replaced with an artificial implant;
Laminectomy (classic). During the operation, part of the intervertebral arch is removed and the canal of the spinal cord is opened. The operation is complex, traumatic and risky, therefore it is used less and less;
Endoscopic intervention. An endoscope is used to eliminate the pathology. The operation is performed without an incision. Access to the affected area is through a puncture. The advantages of the method are low trauma and minimal rehabilitation period;
microsurgical operation. The point is to use miniature surgical instruments at high magnification. Allows you to remove almost any type of hernia without unnecessary damage to surrounding tissues.










