Contents
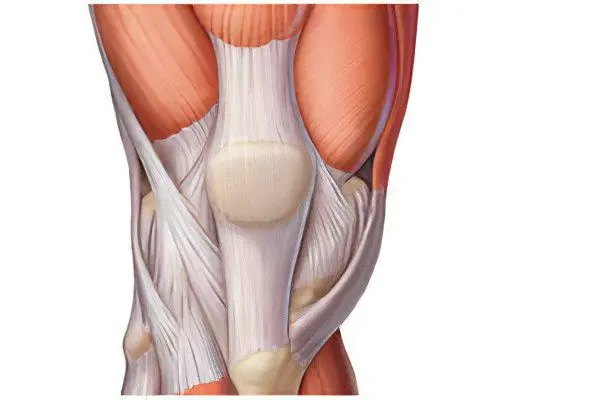
Tendons connect muscles to bones. They are in the form of jumpers that divide the muscle into several sections. And also short, long, wide, narrow. There may be cord-like, rounded, ribbon-like and lamellar tendons. The digastric muscles have intermediate tendons. They pass along the lateral surface of the muscle body and penetrate into its thickness.
Like a muscle, tendons are made up of parallel bundles. The bundles of the first order are surrounded by layers of loose connective tissue and make up the bundle of the second order. A group of beams of the second order forms a beam of the third order. Tendons consist of dense fibrous connective tissue, they contain more fibrous elements than cellular ones.
Due to this, their distinctive property is high strength and low elongation. The tendon part of the muscles grows from 15 to 25 years faster than the abdomen of the muscles. Until the age of 15 tendons are poorly developed, their growth has the same intensity as muscle growth. In the body of the elderly, changes occur in the tissues, the elasticity of the tendons is disturbed, which often leads to injury.
Tendons are protected from rupture during sudden movements and overstresses by the longitudinal elasticity of the tendon tissue. Therefore, in order to prevent tendon injuries, it is necessary to activate, develop and strengthen them, regular sports and certain special exercises will restore their elasticity and strength.
To identify the pathology of the tendons, methods are used – palpation, thermography, ultrasonography, biopsy.
Diseases leading to inflammation of the tendons
There are several types of inflammatory diseases of the tendons, accompanied by a violation of the musculoskeletal system.
1. Tendinitis — inflammatory process is quite common. The causes of its occurrence are always the same, and therefore, in the diagnosis, it is quite simple to identify this pathology. Tendinitis occurs from prolonged chronic overexertion, in which degenerative changes and tendon tears develop. This type of inflammation reduces the strength of the tendon and increases the risk of ruptures.
Tendonitis can also have an infectious nature of the course. Athletes mainly suffer from the dystrophic type, due to heavy physical exertion on muscles, ligaments and tendons. Various rheumatic joint diseases also contribute to the development of such inflammation.
2. Paratenonitis – aseptic inflammation of the peritendinous tissue. It occurs with repeated trauma in the joint area. In this case, in the connective tissue, between the fascia and the tendon, after petechial hemorrhages and the appearance of swelling, deposits of fibrous tissue appear. Knotty seals lead to painful sensations, movements are limited, activity is lost.
The disease damages the Achilles tendon, the extensors of the forearm, the lower third of the lower leg. Paratenonitis can have an acute and chronic course. The treatment for tendon inflammation is immobilization of the hand or foot. Traditional physiotherapy procedures are also effective.
Treatment of acute inflammation of the tendon (tendonitis) involves antibacterial and restorative methods. In the case of aseptic tendinitis, non-steroidal anti-inflammatory drugs are used.
Local treatment consists in fixing the diseased limb. After the acute manifestations of the disease pass, physiotherapy procedures can be prescribed. Warming up should be performed after the acute manifestations of the disease have passed.
This set of procedures includes UHF, microwave therapy, ultrasound, ultraviolet rays. Useful special physical therapy. Soft heat and magnetic fields, improving blood circulation, relieve inflammation, swelling of tissues disappears, and damaged parts of the tendons are restored.
Degrees of tendon sprain, what to do?
Sprain – the most common type of injury, usually occurs in the ankle and knee joint from a sudden movement that exceeds their amplitude. Tendons connect muscles to bones, and ligaments connect bones. These two definitions are often confused. Ligament sprain is in fact always a microscopic rupture with a small stretch, with an average degree of injury, a rupture of individual collagen fibers may occur, if the injury is severe, the entire ligament is torn.
Having a high ability to regenerate, ligaments are restored at any degree of injury. The strongest muscles in humans are found in the lower extremities. This also means that the tendons that attach the muscles to the bones in the legs have to withstand enormous loads. But, unfortunately, there are unsuccessful movements, falls, provoking stretching of the tendons on the leg.
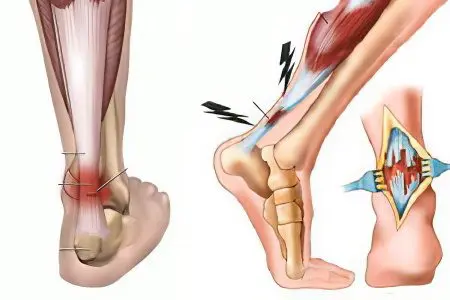
Stretching of the Achilles tendon occurs when there is insufficient warming up of the muscles during sports activities, when wearing uncomfortable shoes, moving on an uneven, rocky surface.
Tendon sprains can be divided into three degrees of difficulty:
The first degree is a slight pain after an injury, aggravated by physical impact.
The second degree is severe pain, swelling of the skin over the damaged tendon. Muscle weakness and increasing pain during exercise are detected.
The third degree is a complete or partial rupture of the tendon, muscle contraction occurs. At the moment of rupture, there may be a sensation of cotton, sharp, severe pain and swelling.
Usually, the third degree of damage to the tendons is restored by the surgical method. Many victims in the first and second degree do not particularly pay attention to treatment and in vain, there may be a weakening of muscle strength, the development of inflammation in the tendon and in the “case” – where there are several of them. Basically, this phenomenon is observed in the tendons of the muscles of the foot and is called tenosynovitis. Chronic inflammation is complicated by an atrophic process that affects the thinning of the tendon fibers, they can be easily torn at low loads.
First aid
When the tendons on the leg are stretched, first aid consists in immobilization, fixation in an elevated position. Then it is necessary to apply ice for 20-30 minutes (repeat 4-5 times a day), after which each time apply a pressure bandage with an elastic bandage to limit the spread of swelling.
Ice will stop bleeding from damaged vessels. Severe pain is relieved by drugs such as diclofenac, analgin, ketanov. On the second day, after the removal of inflammation and edema, if there is no development of a hematoma, the next stage of treatment is used, namely thermal procedures. From exposure to heat, blood flow normalizes, and the damage heals. Effective use of anti-inflammatory ointments.
Recovery
The tendon recovers faster at rest, thanks to the use of foods rich in animal and vegetable proteins. A week later, under the supervision of a specialist, with the help of a set of exercises, they gradually put a load on the sore muscle. Mechanical damage occurs as a result of direct or indirect action of a traumatic agent.
Operation
Surgical intervention is indicated for chronic and habitual dislocations, with a pain syndrome constantly reminiscent of damage, with an obvious change in functional activity. A tendon rupture usually announces itself with a loud crack, unbearable pain and a violation of the motor function of the torn muscle. Open injuries are observed with stab, cut, chopped wounds, with severe injuries. Damage levels:
Avulsion of the tendon from its insertion.
Rupture along the entire length of the tendons.
Rupture of the tendon in the zone of its transition to the muscle. Such phenomena are most likely to occur in older people, and in those whose profession is associated with muscle strain or in athletes.
Rupture and damage to the tendons of the foot
Degrees of damage to the tendons of the foot:
First degree – slight pain, slight swelling of the ankle. You can step on the foot. Unpleasant sensations disappear after a few days of treatment with special ointments and compresses.
The second degree is a medium-sized swelling of the joint, sharp pain when moving the foot.
Third degree – tendon rupture, severe unrelenting pain, significant swelling of the joint.
Rupture and damage to the Achilles or calcaneal tendon (triceps calf muscle), which is attached to the calcaneal tuber and is very thick, appears as a result of strong stress. Usually the gap in this zone is complete. The causes of damage include direct trauma after being hit with a hard object and indirect impact arising from a sharp contraction of the triceps muscle of the leg.
The risk group includes athletes, injury can occur, for example, in runners with a sudden load on the tendon at the moment the foot is taken off the surface at the start, in athletes with a sharp dorsiflexion of the foot during a fall from a height. Partial damage to the Achilles tendon occurs with a direct injury with a cutting object. The victim experiences acute pain, a feeling of a blow to the tendon.
Hemorrhage and edema are observed on the posterior surface of the lower third of the leg. A dent can be seen in the rupture zone. The patient cannot stand on the balls of his fingers, plantar flexion of the foot is impossible. The provision of first aid consists in anesthesia with drugs and its delivery to the trauma department.
Treatment for fresh tears (no more than two weeks) – closed percutaneous suture. A plaster bandage is applied to the affected area for 4 weeks, the leg remains in the same position all the time. After removing the thread from the suture, the leg is fixed for 4 weeks in a different position.
If the injury is old (more than 2 weeks), usually scar tissue has already formed at the ends of the tendons, it is removed, a skin incision is made over the tendon, the ends of the tendon are sutured with a special suture according to the method of Dr. Tkachenko. If there is a tissue defect, plastic surgery is performed followed by a plaster cast for a period of 6 weeks. Full recovery is guaranteed with the use of special exercises and physiotherapy.
The Achilles tendon is the strongest, it stretches when the muscles are tense and allows you to stand on your toe or make a jump. For diagnosis, radiography of the ankle joint in the lateral projection, magnetic resonance imaging, ultrasonic equipment are used. Damage can also be determined using traditional palpation.









