Contents
One of the forms of focal tuberculosis is infiltrative, which is characterized by an extensive tissue reaction of the lungs. In this phase of the disease, symptoms of infiltration and focal inflammation come to the fore. There are several reasons that lead to such a development of the pathological process.
In most cases, the mechanism of infiltrative-pneumonic pathogenesis is triggered as a result of a too violent reaction of the patient’s body to the causative agent of tuberculosis, as well as hypersensitivity of lung tissues in combination with instability of the neurovegetative and endocrine systems.
Causes of infiltrative pulmonary tuberculosis
The causative agents of tuberculosis are microorganisms that belong to the type of acid-fast bacteria of the genus Mycobacterium. There are seventy-four types of such mycobacteria known to medicine. They can be found in water, in soil, in the body of people and animals.
But a person becomes ill with tuberculosis only when infected with several types of mycobacteria at once. Such a pathogenic complex is called M. Tuberculosis and includes the human type Mycobacterium tuberculosis, bovine Mycobacterium bovis, Mycobacterium africanum, Mycobacterium bovis BCG (BCG strain), as well as Mycobacterium canetti and Mycobacterium microti. The group also includes Mycobacterium pinnipedii and Mycobacterium caprae, which phylogenetically belong to the phyla Mycobacterium microti and Mycobacterium bovis.
The main species characteristic of Mycobacterium tuberculosis (MBT) is their highly pathogenic nature, which is expressed in virulence (infectiousness) that can be modified under the influence of external factors. The manifestations of this virulence depend on the state of the victim’s body at the time of the bacterial attack.
A person in most cases becomes ill with tuberculosis as a result of infection with bovine and human types of mycobacteria. The maximum number of M. bovis excretions is recorded in rural residents, where the main route of transmission of the pathogen is the alimentary method (through food). Avian tuberculosis occurs mainly in carriers of pathogenic microorganisms with reduced immunity.
When tuberculous bacteria affect the lungs, lymph nodes, skin, bones, kidneys, intestines and other organs, a special type of inflammatory process occurs – “cold” inflammation. It is characterized by a granulomatous character and leads to the appearance of a large number of cavities prone to decay.
Pathogenesis
As a rule, primary infection in humans occurs by airborne droplets. Much more rare phenomena are infection through food, household and sexual contacts, as well as intrauterine (transplacental) transmission of the pathogen from mother to child.
Bacteria enter the human body when the so-called mucociliary clearance is disturbed, in which goblet-shaped airway cells create a barrier of mucus that traps mycobacteria, and fluctuations in the ciliated epithelium lead to their subsequent evacuation.
The cause of impaired clearance is usually inflammation in the upper respiratory tract, in the trachea and large bronchi. Toxins also have an effect. As a result, bacteria reach the bronchioles and alveoli, which increases the likelihood of developing the disease.
Due to the fact that mycobacteria do not have the ability to produce exotoxin to stimulate phagocytosis (attack by immune cells), a small number of pathogens do not give rapid manifestations. The structure of the affected tissues remains normal for some time. This is called “latent carriage”.
From any point, bacteria with lymph enter the regional lymph nodes, and from there, with the flow of lymph, they enter the internal organs. This process is called primary (or obligate) mycobacteremia.
Pathogens accumulate where the microvasculature is especially developed: in the lungs, in the lymph nodes, in the cortical layer of the kidneys, in the epiphyses and metaphyses of tubular bones, in the fallopian tubes, in the uveal tract of the eyes. The reproduction of the bacteria continues, but the immunity does not have time to develop.
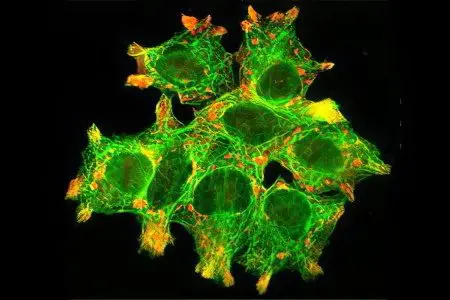
At this time, in places where the most bacteria are collected, phagocytosis begins. The pathogens are attacked and destroyed by polynuclear leukocytes. However, contact with mycobacteria leads to the death of immune cells.
Macrophages, which are included in the phagocytosis of mycobacteria, also turn out to be powerless, since ATP protons synthesized by MBT, as well as cord factors and sulfates, disrupt the functioning of macrophage lysosomes. While inside macrophages, tuberculosis bacteria grow, divide, and this leads to the death of the host cell. And MBT again return to the intercellular space. It turns out “incomplete phagocytosis.”
acquired cellular immunity
Cellular immunity is formed by macrophages and lymphocytes, effectively interacting with each other. Especially important in this process is the contact of macrophages, T-helpers and (CD4+) and T-suppressors (CD8+). After ingesting mycobacteria, macrophages produce antigens and interleukin-1 (IL-1). It starts the work of T-lymphocytes (CD4 +). And T-helpers (CD4+) interact with macrophages and “read” data on the genome of the bacterium. T-lymphocytes (CD4+ and CD8+) are sensitized and start producing chemotaxins, gamma-interferons and interleukin-2 (IL-2).
This causes macrophages to move faster to mycobacteria, and their enzymatic and general bactericidal activity increases. The production of reactive oxygen species and hydrogen peroxide by macrophages is accelerated. An oxygen explosion occurs, which negatively affects the MBT. L-arginine and tumor necrosis factor-alpha together provoke the formation of nitric oxide NO, which has an antimicrobial effect. The result is a decrease in the destructive effect of MBT on the body and the death of the pathogen.
In a situation where the immune response develops adequately, the immunocompetence of macrophages grows in each new generation. They produce mediators that activate B-lymphocytes, which are responsible for the synthesis of immunoglobulins. By producing antibodies, leukocytes envelop the MBT, which as a result stick together. And this facilitates phagocytosis.
The growing enzymatic activity of macrophages can provoke the appearance of cells with delayed type hypersensitivity (HRST) to the antigens of tuberculosis pathogens. As a result, macrophages are transformed into Langhans giant epithelioid cells. They are included in the work to limit the inflamed area.
This leads to the creation of an exudative-productive and productive tuberculous granuloma, which is an indicator of a good immune response to the MBT invasion and the localization of its aggression.
T- and B-lymphocytes, as well as macrophages in the granuloma are especially active. Macrophages are transformed into epithelioid cells, which are responsible for pinocytosis and the synthesis of hydrolytic enzymes. The central part of the granuloma may be characterized by the appearance of a small area of caseous necrosis formed from dead macrophages.
The appearance of the PCCT reaction is fixed two to three weeks after the initial infection. The formation of pronounced cellular immunity is observed after eight weeks.
Mycobacteria begin to multiply more slowly, they become smaller, and the inflammatory specific reaction subsides. However, the pathogen is not completely destroyed. The remaining bacteria are inside the cells (L-form), which prevents the formation of the phagolysosome and makes them inaccessible to the action of lysosomal enzymes. This is a non-sterile form of TB immunity.
Bacteria that remain in the body maintain a population of sensitized T-lymphocytes and provide immunological activity at a sufficient level. So mycobacteria can exist for a long time, sometimes throughout a person’s life. If immunity is reduced, mycobacteria can become active, and the person may become ill.
The decrease in acquired immunity is provoked by AIDS, diabetes mellitus, and stomach ulcers. May be caused by excessive alcohol and drug use. Immunity is negatively affected by starvation, stress, pregnancy, hormone therapy and immunosuppressants. The risk of getting tuberculosis in a person infected for the first time is eight percent during the first two years, then the probability decreases.
Occurrence of clinically expressed tuberculosis
If macrophages are not activated enough, phagocytosis has no effect. Mycobacteria multiply very quickly – exponentially. Phagocyte cells die in large numbers, releasing large amounts of mediators and enzymes of proteolytic enzymes into the intercellular space. Nearby tissues are damaged, “liquefied”. This leads to the formation of a special environment that nourishes mycobacteria outside the cells.
The balance of immune defense is disturbed. There are more T-suppressors (CD8+), and T-helpers (CD4+) lose their immunological activity.
PCZT to antigens rises sharply, and then becomes weaker. The inflammation is spreading. The walls of blood vessels become more permeable, plasma proteins penetrate to the tissues along with leukocytes and monocytes. There is a development of tuberculous granulomas with a predominance of caseous necrosis.
Polynuclear leukocytes, macrophages and lymphoid cells actively infiltrate the outer layer. This leads to the fusion of individual granulomas and an increase in the total volume of the lesion. There is a transition of primary infection to tuberculosis, clinically expressed.
Symptoms of infiltrative pulmonary tuberculosis
Possible clinical and radiological infiltrates of the following types:
broncholobular infiltrate is a focus located in the cortical sections of the first or second segments of the upper lobe of the lungs, has an irregular rounded shape, fuzzy contours, and a diameter of one to two centimeters. Tomography shows two or three or several fresh, merged foci. There are no symptoms, there are no functional changes and bacilli excretion;
Rounded infiltrate means the appearance of foci of darkening, having the shape of a circle or oval with blurred contours, a diameter of one and a half to two centimeters. The focus is usually located in the first, second or fourth segment of the lung. An inflammatory “path” runs from the foci to the root of the lung; against its background, a projection of the bronchus is noticeable. X-ray tomography shows more dense or calcified foci, small decay cavities, changes in the pleura, scars. The development of round infiltrates increases the zone of perifocal inflammation, leads to the disintegration of the caseous center, and a cavity is formed. It includes sequesters and some fluid and is called a pneumonogenic cavern. Bronchogenic seeding leads to the development of foci of pathogenesis in healthy areas of the lung;
Cloudy infiltrate on x-ray it looks like uneven darkening with blurry contours. Opacification is present in one or more segments in the upper lobes of the lungs. This is similar to nonspecific pneumonia, but the difference is that the x-ray changes are persistent, there is a tendency to disintegration and the appearance of cavities;
Lobitis an inflammatory process that captures the whole lobe of the lung. It has a characteristic structure with many caseous foci. The clinical picture is severe. Gradually, the lesion spreads to the entire lobe, on the border of which a clear interlobar furrow appears. According to observations, a small infiltrative focus often develops in front of the lobite;
Periscisuritis, or marginal infiltrate is a cloud-like form, which is located near the interlobar sulcus. This is a triangle with the apex turned towards the root of the lung. At the top, the borders are vague, passing into the lung tissue, which is little changed. The border below coincides with the interlobar pleura and has clear contours;
Caseous pneumonia. A form of the disease that develops in patients with a lack of immunobiological resistance. In the lung tissue, inflammation is observed, where necrosis predominates. Caseous-pneumonic foci spread to the entire lobe or the entire lung.
Various factors provoke caseous pneumonia: malnutrition, pregnancy, diabetes mellitus, extensive damage to the body by mycobacteria with high virulence. As well as pulmonary bleeding, in which blood is aspirated from the MBT. Clinically, caseous pneumonia has a widespread character and intense morphological changes.
In general, the clinical symptoms of infiltrative tuberculosis are expressed depending on the extent of the lesion. As a rule, the disease begins in an acute form: the patient has a fever, and the symptoms may resemble influenza or lobar pneumonia. Manifestations occur against the background of general complete health. Only a thorough survey makes it possible to detect signs of tuberculosis intoxication that arose even before the development of acute manifestations.
A frequent first symptom of this form of the disease is hemoptysis or pulmonary hemorrhage. The acute period may last for several days or several weeks.
Of complaints patients note chest pain on the side where the lung is affected, it is localized in the side or shoulder blades. There is a dry cough or there is a small sputum discharge. Signs of intoxication are clearly visible in the form of poor appetite, sweating, sleep disturbances, increased excitability, tachycardia and general weakness.
With caseous pneumonia the disease begins acutely. The body temperature rises to 40-41 °, there is a big difference between the indicators in the morning and in the evening. Symptoms of intoxication are rapidly increasing. Adynamia develops sharply, profuse sweat appears, pain in the chest, purulent sputum when coughing, shortness of breath. The person quickly loses weight.
Diagnosis of infiltrative pulmonary tuberculosis

Physical examination at the onset of the disease reveals lagging of the chest during breathing in the side of the lung that is affected. The muscles of the chest are tense, the voice begins to tremble.
Negative percussion and auscultation data most pronounced in the case of massive pneumonia of the type of lobitis, as well as when the disintegration of the infiltrate and the formation of cavities begin. On the surface above the affected area, the percussion sound becomes dull, bronchophony appears, bronchial breathing develops, moist and sonorous persistent wheezing of various calibers.
Differential diagnosis of infiltrates
With an acute onset of the disease and the rapid development of a pneumonic process in people without a history of tuberculosis, a diagnosis of “nonspecific pneumonia” is made.
Of particular difficulty is the diagnosis of infiltrative-pneumonic tuberculosis, which is accompanied by influenza syndrome.
Such tuberculosis differs from pneumonia:
Specific signs of tuberculosis intoxication;
The gradual onset of the disease;
The absence of catarrh in the upper respiratory tract;
Relatively satisfactory condition of patients, even at high temperatures.
Nonspecific pneumonia, accompanied by fever, is characterized by a serious condition of patients. At the same time, the specific process (tuberculous) does not have physical manifestations at the start of the disease: they appear only if the process progresses.
Blood tests of patients show small shifts in the leukocyte formula and a slight increase in ESR. With croupous pneumonia, leukocytosis is high and has a shift to the left, ESR is sharply increased.
X-ray examination shows the localization of tuberculous infiltrates mainly in the upper sections – in the first, second and sixth segments. Inflammatory non-specific processes are concentrated in the middle and lower fields.
The pictures show a “path” leading from the infiltrate to the root of the lung. As a rule, isolated focal shadows are visible on the periphery of the main focus. They can also be observed on other parts of the same or different lobe of the lung.
Sometimes a diagnosis of “tuberculosis” can only be made by dynamic observation of the patient and the ineffectiveness of treatment with antibacterial drugs, as well as the presence of mycobacteria in sputum.
The long period during which there is a reverse development serves as a difference between infiltrative-pneumonic tuberculosis and eosinophilic pneumonia: its focus resolves quickly, in a few days, and eosinophilia in the blood reaches 30-45 percent.
Differentiation of tuberculous infiltrate is carried out with malignant neoplasms, with echinococcus and actinomycosis, lymphogranulomatosis, dermoid cysts, pulmonary syphilis and other diseases. Accurately recognize the nature of the process in the lungs allows only a thorough examination.
Treatment of infiltrative pulmonary tuberculosis
Therapy of infiltrative tuberculosis is carried out in a hospital. Antibacterial drugs are used in combination with pathogenetic therapy. Treatment continues until the infiltrative changes resolve completely – about nine to twelve months. In the future, courses of chemotherapy are carried out to prevent relapses – already at the dispensary.
Different methods of treatment are used in combination. If the effect does not last long, in some cases, collapse therapy (artificial pneumothorax) is performed or surgery is performed.
Prevention of infiltrative pulmonary tuberculosis

Being a social disease, tuberculosis is often provoked by certain conditions of the patient’s life. In Russia, among the reasons for the deterioration of the epidemiological situation with tuberculosis include a decrease in the standard of living of the population, an increase in the number of people who do not have a specific place of residence, and the development of migration. According to statistics, men are more likely to get sick – three point two tenths more than women. And among men, the incidence rate is growing two and a half times faster than among women. Most of the patients are aged twenty-twenty-nine years, the second place in terms of incidence is a group of thirty-thirty-nine years.
People who are in prison are XNUMX times more likely to get sick than the rest of the country’s population on average.
In order to prevent it is necessary to carry out the following measures:
Anti-epidemic measures that correspond to the extremely unfavorable TB picture in the country;
Detection of patients at the first stages and financing of drug provision;
Regular examinations of people who get jobs in livestock enterprises, where tuberculosis diseases are observed among cattle;
Allocation of isolated housing to people with an active form of tuberculosis living in communal apartments and hostels;
vaccination of newborns in the first thirty days of life.
Which doctor should be consulted?
If you suspect infiltrative pulmonary tuberculosis, you should contact a phthisiatrician or pulmonologist.
Author of the article: Makarova Evgenia Vladimirovna, pulmonologist









