Contents
What is infectious arthritis?
Any organism is an open biological system. This means that it constantly interacts with the environment, which affects the life of an individual in different ways: beneficially or negatively. The invasion of infectious pathogens disrupts the functioning of all organ systems and mobilizes defense mechanisms.
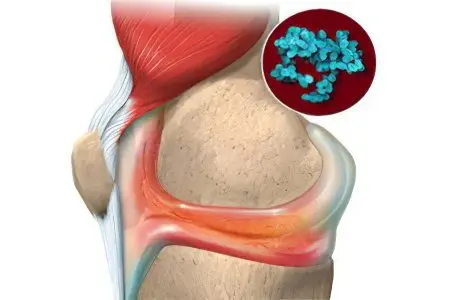
infectious arthritis – This is an inflammatory process in the joints, caused by the penetration of infectious pathogens into the body. Otherwise, this type of arthritis is called purulent, pyogenic (causing the formation of pus) or septic. At the initial stage, pus in the synovial fluid may be absent. Infection with microbes can be local and limited to the joint or general. Sepsis is a general infection of the blood.
Depending on the localization, the following types of arthritis are distinguished:
ankle;
arthritis of the metatarsus or tarsus;
knee;
hip;
sacroiliac – sacroiliitis;
vertebrate;
wrist;
elbow;
brachial;
acromioclavicular and sternoclavicular;
infectious arthritis of the fingers, hands, or feet.
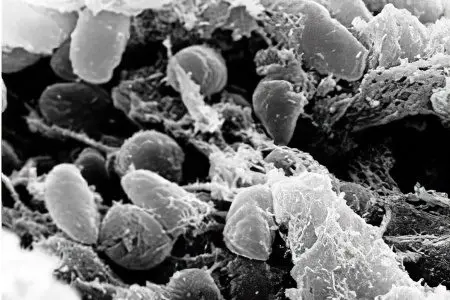
Microorganisms in the synovial fluid (leukocyte count 10-100×109/ l, with more than 90% neutrophils), blood (leukocytosis, increased ESR – erythrocyte sedimentation rate), sputum, cerebrospinal fluid, genital swab or urine are detected using laboratory tests. Gram stain is used for analysis. This research method involves the identification of gram-positive (staining) and gram-negative microorganisms, depending on their reaction to a special solution.
Special diagnostic studies:
radiography in two projections;
biopsy (excision) of a piece of synovial tissue;
Wright reaction tests and Burne tests;
computed tomography – visualization of sequestered bone tissue. Sequester – dead area of bone tissue;
Magnetic resonance imaging;
ultrasonography;
radioisotope scanning.
Incidence statistics: gonococcal infectious arthritis occurs in 0,6 – 3% of women and 0,1 – 0,7% of men with gonorrhea. Predominant age: up to 40 years and after 60 years. In 25-50% of patients with gonococcal dissemination, mono- or oligoarthritis occurs. In the latter, only two or three joints are affected. Infectious arthritis develops in newborns when gonococci from a mother with gonorrhea enter their bloodstream. In about 70% of cases of infectious arthritis, irreversible joint destruction can be avoided.
If the inflammatory process cannot be stopped quickly enough, then complications of infectious arthritis arise:
ankylosis – fusion of articular surfaces;
phlegmon;
bone displacement;
osteoarthritis due to cartilage damage;
fibrositis;
osteomyelitis (“inflammation of the bone”);
spondylitis – inflammation of the spine;
limb shortening due to violation of the bone growth zone in children;
osteochondritis – an inflammatory process in bone and cartilage tissue;
abscess – an abscess;
septic shock leading to multiple organ failure syndrome.
Symptoms of Infectious Arthritis

an increase in body temperature above 38% C (subfebrile value);
chills – a painful sensation of cold;
sweating;
nausea and vomiting (mainly in children) as signs of intoxication;
weakness, lethargy;
muscle aches;
malaise;
joint pain;
limited movement of the diseased limb – stiffness;
redness of the skin in the joint area;
high local temperature at the site of infection;
accumulation in the joint of effusion – fluid from the blood vessels;
swelling;
periarthritis syndrome – dermatitis: migratory polyarthralgia, hectic-type fever (febris hectica), tendosynovitis and dermatitis (“inflammation of the skin”) – maculopapular or vesicular, and then vesiculo-pustular rashes.
If infectious arthritis is accompanied by another disease, then the symptoms will be wider. With periarthritis, inflammation covers the capsule, ligaments, tendons and muscles. Arthralgia is a flying pain in the joints. Tenosynovitis is inflammation of the synovial lining of a tendon. Papule in translation means “nodule”. These are small bumps on the skin. A vesicle is a vesicle with liquid contents. The pustule is the primary element of the rash.
The peculiarity of the course of infectious arthritis is its suddenness and rapid progression. It is impossible to accurately diagnose the causative agent of inflammation of the joint without additional research. Its symptom complex is too similar to the signs of other diseases. These include gout, rheumatic fever, borreliosis and some other pathologies.
Causes of Infectious Arthritis
There are the following causes of infectious arthritis:
penetration of pests through broken skin as a result of a puncture, surgery or injury (bruise, burn, wound, etc.) – primary arthritis;
pathogen transfer along with lymph or blood, i.e. hematogenous way – secondary arthritis.
Any foci of inflammation pose a danger to the whole organism.
The products of the inflammatory process are easily carried to other organs. Risk factors for septic inflammation of the joints:
prematurity;
chronic arthritis;
gonorrhea – a sexually transmitted disease that affects the urinary tract;
furunculosis, accompanied by the appearance of boils;
peritonsillar abscess behind the tonsils;
angina – inflammation of the mucous membrane of the pharynx;
scarlet fever (mainly in childhood);
inflammation of the middle ear;
pneumonia – inflammation of the lungs;
infective endocarditis – inflammation of the inner lining of the heart – the endocardium;
immunodeficiency states;
recurrent septicemia;
joint prostheses;
diabetes mellitus – an endocrine disease due to insulin deficiency;
sickle cell anemia — anemia;
chronic tonsillitis – inflammation of the palatine tonsils;
caries – destruction of tooth tissues;
tumor;
hypogammaglobulinemia – protein deficiency;
alcohol addiction;
drug use.
Types of infectious agents:
bacteria;
viruses;
parasites;
pathogenic fungi.
Bacteria:
staphylococcus;
gonococci;
streptococci;
hemophilus bacillus – Haemophilius influenzae;
gram-negative bacteria, such as Pseudomonas or salmonella – Salmonella.
Types of Staphylococcus:
Staphylococcus aureus;
epidermal staphylococcus – Staphylococcus epidermidis.
Types of Streptococcus:
β-hemolytic streptococcus of group A – Streptococcus pyogenes – is activated in gram-positive flora;
streptococci of other groups.
Viruses:
human immunodeficiency virus – HIV;
rubella;
epidemic parotitis;
hepatitis B;
parvoviruses.
Parasites are the causative agents of the following diseases:
opisthorchiasis;
strongyloidiasis – cochinchin diarrhea;
dracunculiasis – guinea worm disease;
hookworm – a rash of miners, earthen scabies or Egyptian chlorosis;
schistosomiasis;
echinococcosis liver;
filariasis, including wuchereriosis, brugiasis and onchocerciasis;
loiasis causing Calabar tumor.
So, the main varieties of bacterial infectious arthritis, depending on the etiology, are the causes of its occurrence:
gonococcal;
tuberculous primary bone or primary synovial form;
brucellosis;
borreliosis or lyme (for Lyme disease);
yersinia;
dysenteric;
salmonella.
The method of treatment, depending on the type of pathogen, varies slightly, so antibiotics begin to be administered immediately after inflammation is detected. Based on the diagnostic results, the chosen course can be adjusted. So, additionally prescribed, for example, antiparasitic drugs.
Treatment of infectious arthritis

Primary measures are pain relief, antibiotic therapy and fever reduction. Pain is relieved with analgesics and splinting – immobilization of the diseased joint.
Antibiotics and / or antifungal drugs at the beginning of the treatment course are administered intravenously or directly into the joint. Pus is pumped out with the help of drainage. Antibiotics are used for at least two more weeks after the symptoms of inflammation disappear, but they are already taken orally. In some types of infectious arthritis, antiparasitic drugs are also used, compresses are applied to the projection area of the affected joint.
The type and combination of medications are determined by the type of causative agent of arthritis:
Benzylpenicillin sodium salt or Ceftriaxone (against gonococci, meningococci);
Cefalotin, Vancomycin, Clindamycin, Nafcilin (staphylococci);
Benzylpenicillin sodium salt and Vancomycin (streptococci);
Gentamicin and, for example, Ampicillin or Tseporin (gram-negative bacteria);
Chloramphenicol – Levomycetin (microorganisms of the genus Haemophilus).
If there is no positive dynamics, then it is necessary to reconsider the method of treatment. Perhaps the drugs are ineffective or their dosage is incorrectly selected. In case of infection of the prosthetic joint, the removal of the prosthesis and its replacement with a new one is indicated.
Analgesics are prescribed a variety of:
Acetaminophen;
Paracetamol;
Analgin;
Capsaicin;
Tylenol;
Oxycodone;
Methadone;
Tramadol;
Ibuprofen.
Inflammation is removed with the help of non-steroidal agents. They also have analgesic and antipyretic effects:
Acetylsalicylic acid;
Nimesulide;
Movalis or Meloxicam;
Piroxicam;
Celebrex;
Nimesil;
Indomethacin.
Steroid hormones also reduce the inflammatory process:
Hydrocortisone;
Prednisolone;
Triamcinolone;
Kenalog;
Detralex
Cartilage tissue is restored using chondroprotectors:
Chondroitin sulfate;
Glucosamine;
Hondrolon;
Structure;
Arthritis.
Chondroprotectors are taken in long courses even after the end of the main treatment.
They significantly accelerate cell regeneration and slow down the process of cartilage destruction. Forms of medications prescribed for arthritis:
capsules or tablets (eg Diclofenac);
solutions for intramuscular and intraarticular injections (for example, corticosteroids);
gels (for example, Diklak);
cream;
ointments (for example, Bishofit, Nikoflex, Menovazin);
solutions for compresses (for example, Dimexide).
Surgery is used only in very severe cases. Surgical methods of treatment:
arthroscopy – removal of processes from the bone and other manipulations through a micro incision;
endoprosthetics – replacement of joint components with implants;
arthrodesis – complete immobilization of the joint;
arthrolysis or Wolff’s operation – excision of fibrous adhesions;
synovectomy – removal of the affected synovial membrane;
osteotomy – removal of part of the bone in order to reduce pressure on the joint;
resection – removal of a joint or part of it;
arthroplasty — joint replacement.
To speed up rehabilitation, a course of physiotherapy and a special therapeutic and physical exercise complex are prescribed. Of the physiotherapy procedures, the following are used:
magnetotherapy;
amplitude pulse or sinusoidally modulated currents;
electrophoresis, in which drugs are ingested through a direct electric current;
laser;
ultrasound – phonophoresis;
physiotherapy with paraffin or ozocerite.
Only timely treatment can avoid unpleasant complications and disability. Mortality from complications of infectious arthritis is 5-30%.









