Contents
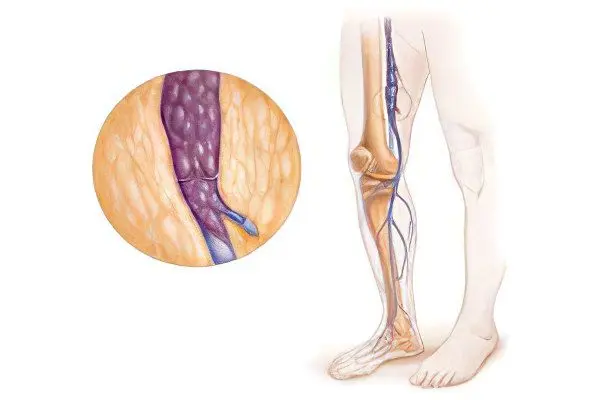
Iliac vein thrombosis is the formation of a blood clot in the vena cava system that interferes with normal blood flow. In the practice of clinicians, thrombosis of the vena cava is more common than thrombosis localized in other parts of the body. Pathology is characterized by pains that have a bursting character, blue skin, reporting of the skin, swelling of the veins of the lower extremities.
The common iliac vein is a large vessel with no valves. It originates in the region of the sacroiliac joint, where the external and internal iliac veins merge. First, the common right iliac vein passes behind, and then laterally, the iliac artery. The left iliac vein runs medially. The internal iliac vein also does not contain valves and is located on the side wall of the small pelvis.
Iliac vein thrombosis occurs in 10-15% of all thrombosis cases. This is a serious condition that requires emergency medical attention, as it poses a direct threat to human life. Thrombosis should not be confused with thrombophlebitis.
Symptoms of iliac vein thrombosis

Symptoms that indicate iliac vein thrombosis have a number of features:
The pain is localized most often in the groin, in the region of the inner surface of the thigh.
The pain may radiate to the calf muscle.
The nature of the pain: bursting, pulling, dull. With iliac vein thrombosis, acute pain never occurs.
Pain first bothers a person only during physical activity, and then begins to appear at rest.
Pain is associated with a number of factors:
The development of periphlebitis in the iliac region (inflammation of the tissue surrounding the iliac vein);
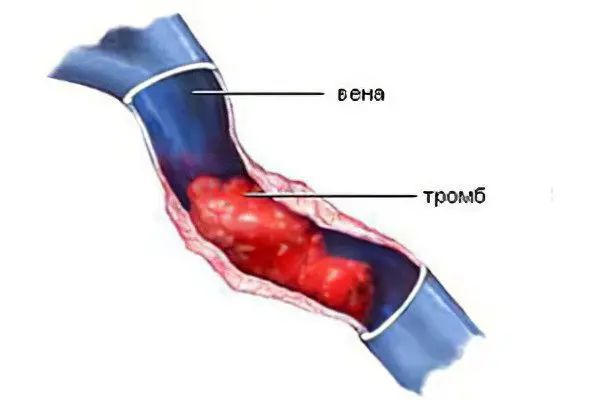
Stretching of the walls of the affected vein by formed blood clots;
Stretching of the walls of the tributaries of the vein due to increased blood circulation;
Increased venous pressure;
Increased blood circulation in the arteries that are associated with the iliac vein that has undergone thrombosis;
Tension of the limbs.
Swelling of the leg on the side of the lesion. A characteristic feature of iliac vein thrombosis is that tissue swelling extends not only to the thigh and leg, but also to the genitals and buttocks. Of course, it is the thigh that swells the most. When you press on the affected tissue, there is no fossa left. The reason for its absence is that the veins during thrombosis are overflowing with blood, so water is contained not only in the subcutaneous fat layer, but also in soft tissues. Edema always occurs, but the degree of its severity varies in all patients.
Degrees of edema
There are the following degrees of edema in thrombosis of the vena cava:

If the femoral part of the limb increases in size by less than 3 cm, then the edema is considered small.
If the femoral part of the leg increases in size by 3-5 cm, then the edema is considered medium.
If the femoral part of the leg increases in size by 5 cm or more, then the edema is considered sharp.
Blue discoloration of the skin of the limb from which thrombosis is observed. The upper part of the thigh and pelvic cavity may also acquire a purplish-red hue, or a milky-white hue (white phlegmasia). With a cyanotic color of the limbs, the pain will be bursting, “tearing” the vein from the inside. If the vein is overfilled with blood, then blisters containing hemorrhagic fluid may appear on the skin, and the skin itself will become black. If there is a complete blockage of the vein, venous gangrene develops. With white phlegmasia, the leg becomes cold, its sensitivity is lost, mobility decreases.
Small brown dots often form on the surface of the skin of the thigh.
There is an increase in the size of the saphenous veins of the thigh. This is most noticeable above the pubis and on the anterior wall of the peritoneum.
Less commonly, patients develop ulcerative lesions of the lower extremities. Ulcerative defects most often develop with multiple thrombosis of the veins of the lower extremities.
Ulcers on the legs with isolated thrombosis of the iliac vein do not form.
With inflammation of the vein and surrounding tissues, an increase in body temperature is possible.
A common symptom of iliac vein thrombosis is enlarged inguinal lymph nodes.
The disease never develops at lightning speed. The process of thrombus formation occurs gradually, with a gradual increase in the intensity of symptoms.
Stage of the disease
Doctors distinguish several stages of the development of the disease:
Prodromal stage, which is always accompanied by pain. They arise in the region of the upper third of the thigh, give to the groin, lower back, abdomen, lower limb from the affected side of the vein. The pain is dull, aching. At this stage, an increase in body temperature is possible. Often, it is unexplained fever that is the only sign of incipient iliac vein thrombosis. This symptom is especially relevant when it occurs in a certain category of patients: in the postpartum or postoperative period, in people immobilized after an injury, etc.
The stage of severe manifestations of the disease. The pain intensifies, spreads, capturing more and more areas, swelling of the thigh and limbs is formed. Possible numbness of the leg on the side of the lesion.
The combination of symptoms can be varied. Sometimes the disease does not occur without any external manifestations.
Causes of iliac vein thrombosis
Iliac vein thrombosis develops under the condition that a combination of several factors occurs:
The wall of the vein was damaged. The cause may be chemical, allergic, infectious or mechanical trauma.
Violations in the process of blood clotting.
Slow down blood flow.
Blood viscosity can increase for various reasons. If there are damages on the walls of the vein, then this will lead to the fact that blood clots will begin to form on them. A small blood clot provokes an inflammatory reaction, which entails further damage to the vessel wall. This becomes a predisposing factor for the formation of new blood clots.
Stagnation of blood and lymph in the veins of the lower extremities is another reason that leads to the formation of blood clots. Stagnation occurs in those people who spend a long time in an immobilized state, or lead a sedentary lifestyle.
Risk Factors
The mechanisms that can trigger the formation of blood clots in the iliac vein are:
Transferred operations. If a person is motionless, congestion of blood in the veins will lead to the formation of blood clots.
Transferred infections.
Being immobilized after surgery or due to illness.
Postpartum period.
Taking hormonal drugs to prevent the development of unwanted pregnancy. Blood clots form due to thickening of the blood.
The presence of a malignant tumor in the body. In terms of the formation of thrombosis, cancer of the lungs, stomach and pancreas is of particular danger. Blood clots form against the background of the fact that these diseases lead to thickening of the blood.
Thrombohemorrhagic syndrome.
Complications

The most formidable complication of the disease is the detachment of a blood clot with pulmonary embolism. This can happen with any physical activity, which is always accompanied by an increase in blood circulation. Parts of the thrombus through the veins move along with the blood flow to the lungs, enter the pulmonary artery and clog it. This causes acute heart and respiratory failure, which is often fatal. If a blood clot enters a small pulmonary artery, then this entails a pulmonary infarction.
Another complication of the disease is chronic venous insufficiency. It is dangerous by malnutrition of the lower extremities, the formation of eczema, trophic ulcers, and the development of lipodermatosclerosis. Therefore, the treatment of the disease should be urgent.
Diagnostics

The phlebologist is engaged in the diagnosis of the disease.
The doctor in service has many methods that allow you to identify the existing problem, including:
Conducting a radionuclide study with labeled fibrinogen.
Duplex scanning of the veins, which is aimed at assessing hemodynamics.
X-ray of vessels with the use of a contrast agent. This allows you to qualitatively assess the condition of the iliac vein and visualize the thrombus.
Of the laboratory diagnostic methods, the most informative is the determination of the level of D-dimer in the blood plasma. Also, modern express tests can be used to determine the level of fibrin monomer in the blood, fibrinogen in plasma.
As a rule, these studies are enough to confirm or refute the diagnosis.
Treatment of iliac vein thrombosis
All patients with iliac vein thrombosis should be hospitalized. This is due to the fact that such patients remain at a high risk of developing serious complications that pose a direct threat to life.
The tasks of the conducted terraria should be the following:
Prevent further spread of thrombosis.
To prevent the development of pulmonary embolism.
Stop the spread of edema, which will avoid the formation of gangrene and save the affected limb.
Carry out therapeutic measures aimed at restoring the patency of the iliac vein.
Prevent recurrence of the disease.
During the week, the patient is administered heparin. After that, they are already transferred to soft coagulants. The patient should take it for six months. If the patient abuses alcohol, he has cirrhosis of the liver, or his age exceeds 75 years, he is prescribed antiplatelet agents.
Relapses of thrombosis occur in the first 3-6 months, but sometimes this period is extended for a year or more. Therefore, in some patients, anticoagulant therapy can be prescribed for life.
Local treatment is reduced to local hemorrhage. In the future, ointments with heparin and a non-steroidal anti-inflammatory component are applied to the affected area.
The patient for 7-10 days must comply with strict bed rest. Immobilization for a longer period is meaningless (if the thrombus does not pose a risk of embolism). In the future, patients are shown dosed walking, performing special gymnastic exercises.
While the person is in an immobilized position, a Beler splint is placed on the limb and the part of the bed where the legs are located is raised.
If there is a risk of separation of a blood clot, surgical intervention is indicated – thrombectomy.
[Video] Cardiovascular surgeon, phlebologist Abasov M. M. – How to get rid of a blood clot in 2 weeks:









