Contents
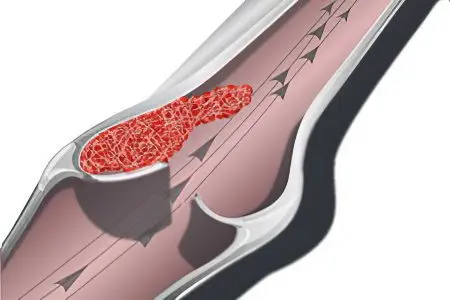
Ileofemoral thrombosis is a blockage of the deep femoral and iliac veins by a blood clot. The disease is singled out as a separate nosological form, as it has a severe course and poses a direct threat to human life. Ileofemoral thrombosis is often complicated by pulmonary embolism. Therefore, if signs of pathology are detected, the patient should be provided with emergency medical care.
The left limb suffers from ileofemoral thrombosis 3-4 times more often than the right.
Causes of ileofemoral thrombosis
The causes of ileofemoral thrombosis can be varied, among them are:
Injuries of the veins and soft tissues of the lower extremities.
Introduction of a bacterial infection into the body.
Prolonged bed rest, for example, after surgery or against the background of a serious illness.
period after the birth of a child.
DIC syndrome.
The presence of a malignant tumor in the body. Of particular danger in terms of the development of thrombosis are neoplasms located in the pelvic area: cancer of the sigmoid colon, kidneys, adrenal glands, cervix, as well as retroperitoneal sarcoma.
Aneurysm of the abdominal aorta, femoral or iliac arteries.
The presence of a popliteal cystic neoplasm.
Pregnancy.
Any purulent processes that are localized in the pelvic area, in its cellular spaces and organs.
Iatrogenic venous disease.
retroperitoneal fibrosis.
Most often, ileofemoral thrombosis is an ascending pathology that originates in the popliteal or femoral segment.
Symptoms of ileofemoral thrombosis

The course of the disease is divided into two phases: prodromal and acute (stage of severe symptoms).
The prodromal stage is characterized by the following features:
An increase in body temperature to subfebrile marks.
Pain in the sacrum and lower back, in the lower abdomen, in the legs. Particularly severe pain will be from the affected vessel.
Pain occurs unexpectedly for a person, is dull and aching in nature.
Sometimes the pain appears only while walking.
The acute stage of the disease is expressed by the following symptoms:
An increase in body temperature to feverish values.
Increased pain, which becomes very intense, covers the groin, thigh and calf muscle.
The appearance of a feeling of heaviness in the limbs. Patients indicate that their leg is bursting from the inside.
The occurrence of edema, which extends to the entire leg, starting from the foot and ending with the inguinal fold. Possible swelling of the buttocks.
Edematous tissues exert strong pressure on the vessels, resulting in their spasm. This is expressed in acute malnutrition of the lower limb, in sharp pains, deterioration of sensitivity.
The skin changes color. Sometimes there is a pronounced pallor of the lower extremities (white pain phlegmasia), and sometimes cyanosis occurs (blue pain phlegmasia). White phlegmasia is a consequence of arterial spasm, and blue phlegmasia develops when the blood flow in the femoral and iliac veins is completely blocked.
In the inguinal region, the veins begin to strongly “shine through” through the skin, the vascular pattern intensifies.
The general condition of the patient worsens significantly when serious complications develop: thrombosis of the inferior vena cava, pulmonary embolism, venous gangrene, phlegmasia.
The posterior muscles of the limbs respond with pain when trying to palpate. Painful infiltrates can be found in the immediate vicinity of the great vessels.
Lymph nodes in the groin area increase in size and become painful.
A person cannot make active movements of the lower limb. Passive movements cause pain.
Separately, it should be noted that pale phlegmasia is an extremely severe complication of ileofemoral thrombosis. It often ends in the death of the patient. Against the background of persistent arterial spasm, collapse develops with partial or complete loss of consciousness, a sharp drop in pressure, and an increase in body temperature up to 40 ° C. The size of the leg increases by 2 times, the skin is cold to the touch, the pulse on the legs is not palpable.
If it is possible to save the life of the patient, then the consequences of white phlegmasia will disturb him for a long time. This is expressed in dystrophy of the muscle fibers of the lower extremities, which develops against the background of prolonged edema. The joints lose their former mobility, the active movements of the leg will be sharply limited.
Blue phlegmasia is characterized by complete blockage of all main and auxiliary venous arteries of the thigh and lower leg. The leg increases in size by 2 times, the skin becomes cyanotic, covered with subcutaneous hemorrhages, the muscles are tense. In this case, the body temperature rises to 40 ° C, shock may develop with shortness of breath, tachycardia and loss of consciousness.
If the patient can be saved, then after 2-3 days the leg tissues begin to undergo necrosis, blisters with liquid appear on it, and sensitivity is completely absent. In the future, symptoms of hemolytic jaundice join. On the 4th-7th day, the tissues of the fingers undergo necrosis, and then the patient develops gangrene of the foot. During this period, about 45% of all case histories end in death.
Diagnostics

Diagnosis of the disease begins with the examination of the patient. According to the characteristic set of symptoms, the doctor will be able to suspect ileofemoral thrombosis.
The following instrumental methods are used to confirm the diagnosis:
Duplex or triplex scanning.
X-ray contrast phlebography.
Radionuclide phlebography.
Scanning with labeled fibrinogen.
Be sure to distinguish between ileofemoral thrombosis with erysipelas, with renal and heart failure, sciatica, arthritis, bursitis.
Treatment of ileofemoral thrombosis
Without exception, all patients with an established diagnosis of “ileofemoral thrombosis” are necessarily hospitalized in an angiosurgical hospital. The patient must be transported in a supine position. Until the moment of medical assistance, he must adhere to the strictest bed rest. If it is not possible to perform a qualitative examination of the victim, then he is prescribed anticoagulants, fibrinolytics and thrombolytics for up to 10 days.
General recommendations for the management of patients with acute ileofemoral thrombosis:
Anticoagulant drugs.
Elimination of pain, removal of the patient from a state of shock.
Removal of spasm from blood vessels, normalization of hemodynamics.
Thrombolysis drugs. However, it should be remembered that the use of thrombolytic drugs is always associated with the risk of bleeding and death of the patient. Therefore, thrombolysis drugs are prescribed only for patients under the age of 50 who have experienced acute thrombosis no later than 7 days before contacting a doctor. At the same time, cava filters should be installed in patients, otherwise there is a high probability of the spread of small particles of a blood clot through the bloodstream and the development of a pulmonary embolism.
Fibrinolysis activators.
Normalization of rheological parameters of blood.
If inflammation develops, antibiotics are indicated.
An operation for ileofemoral thrombosis is prescribed only for vital indications: if the patient is diagnosed with floating thrombi, which pose a threat of pulmonary embolism, or with the development of complications of thrombosis. These include: embologenic thrombosis, high risk of developing gangrene against the background of blue phlegmasia, ascending thrombosis.
There are also relative indications for surgery, including:
Lack of effect from drug treatment for 2-3 days.
The duration of thrombosis is more than 8 days.
old age.
Thrombectomy is the main method of surgical intervention for ileofemoral thrombosis. It should be remembered that with blue phlegmasia, conservative therapy is useless in 100% of cases. The prognosis for blue phlegmasia is largely determined by how timely the surgical intervention was performed (before the development of gangrene). In this case, radical thrombectomy is indicated for patients. The risk of PE increases with thrombectomy in the right iliac vein.
[Video] Cardiovascular surgeon, phlebologist Abasov M. M. – How to get rid of a blood clot in 2 weeks:









