Contents
Hypovolemia is a condition characterized by a decrease in blood volume in the human body. Hypovolemia can develop against the background of various disorders and health problems, but all of them are accompanied by a loss of fluid, or its exit from the bloodstream into the surrounding tissues.
Normally, a healthy man in the body should circulate 70 ml of blood for every kilogram of weight. For women, this figure is 66 ml. Only when the vessels are filled with blood as expected, the normal level of blood pressure is maintained in the body. If the volume of this life-supporting fluid decreases, then the pressure begins to fall, a person develops hypotension, tissues suffer from oxygen starvation, and the work of all internal organs is disrupted.
In the human body, water is present almost everywhere, and not only in the vascular bed. It is called extracellular fluid. It is necessary to provide nutrition to tissues and to normalize metabolic processes in it. Blood and extracellular fluid are interconnected, so the loss of water by the body will necessarily affect the volume and concentration of blood.
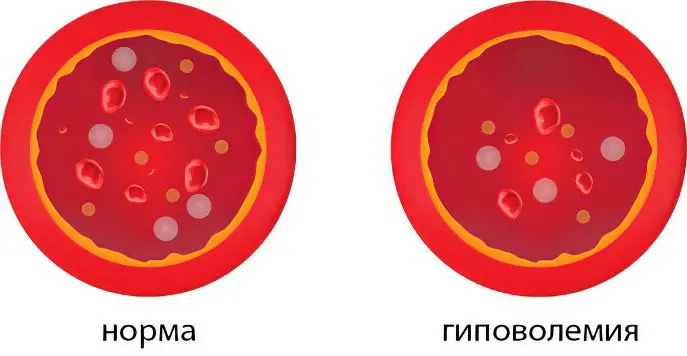
The liquid part of the blood is called plasma, the rest of its volume is represented by platelets, erythrocytes and leukocytes. Depending on the type of hypovolemia, the ratio of the cellular and plasma components of the blood will differ. As a result, the total volume of circulating blood in the body decreases, and the proportions between its main constituent elements (plasma and blood cells) can also be disturbed.
Of course, all doctors are familiar with such a concept as hypovolemia. However, to date, there is no clear scheme for identifying this disorder, which significantly complicates the diagnostic process. The same feature applies to the treatment of hypovolemia. Therefore, often the patient is prescribed an unreasonable blood transfusion, which can harm human health. The doctor, before prescribing treatment, must identify the cause that led to hypovolemia and clearly distinguish this concept from dehydration.
It should be borne in mind that severe hypovolemia can lead to the development of shock conditions that threaten human life. Therefore, sometimes the decision on the method of providing first aid to the patient must be made very quickly. Otherwise, it will not be possible to save his life.
Etiology and pathogenesis of hypovolemia
What can happen in the body with hypovolemia:
The level of proteins and electrolytes in the liquid component of the blood and in the extracellular space changes.
Peripheral vessels expand, due to which the capacity of the vascular bed as a whole increases.
Hypovolemia can develop due to direct excretion of blood cells and plasma from the body.
The causes of hypovolemia can be the following:
Bleeding accompanied by blood loss.
Shock.
The development of burn disease.
Allergic reaction.
The development of dehydration against the background of damage to the body by an intestinal infection.
Pathological or physiological hemolysis.
Vomiting during pregnancy, provoked by toxicosis.
Copious excretion of urine in diseases of the kidneys.
Diabetes and diabetes insipidus.
Inability to consume water, for example, with tetanus or rabies.
Overdose of certain drugs. In terms of the development of hypovolemia, special vigilance should be shown in relation to diuretics.
When the volume of blood in the body decreases, it leads to various disorders in the body. First, he tries to compensate for them with his own strength, and then these violations lead to irreversible consequences. They cannot be corrected even by therapeutic measures. Therefore, hypovolemia should be corrected as soon as it is detected.
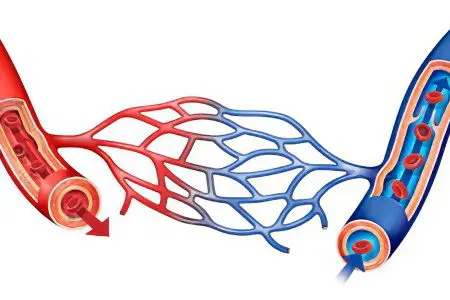
The capacity of the vascular bed and the volume of blood are two concepts that exist in a tight bundle in the human body. With changes in fluid volume, the vascular bed changes its capacity to compensate for its deficiency or excess. If the volume of blood in the body decreases, then it reacts to this with a spasm of capillaries, which makes it possible to replenish its reserves in large vessels. Thus, it compensates (fully or partially) for the onset of hypovolemia.
With allergies and poisonings, when blood volumes do not change, an increase in the vascular bed occurs, so the body also tries to compensate for relative hypovolemia. Indeed, against the background of these reactions, the return of venous blood to the heart decreases. This threatens to disrupt its work and oxygen starvation of tissues.
Hypovolemia can develop with pathologies of the endocrine and urinary systems. Blood volumes decrease due to the abundant removal of water from the body, and along with it, salts come out that are capable of retaining fluid. Diabetes mellitus contributes to the development of hypovolemia due to the presence of glucose in urine, which attracts large volumes of fluid.
Disturbances in the work of the pituitary gland can lead to the development of hypovolemia, since a deficiency of antidiuretic hormone provokes frequent and profuse urination. In this case, hypovolemia will not have a severe course, since the body loses not blood reserves, but extracellular fluid during such a violation.
Burn disease contributes to the development of hypovolemia for the reason that with such tissue lesions, impressive plasma losses occur. The situation is aggravated by intoxication of the body. In addition, with serious burns, blood microcirculation is completely disrupted in the area that was damaged.
Intestinal infections contribute to the development of hypovolemia, as the fluid will be quickly excreted from the body against the background of severe diarrhea. The situation is aggravated by vomiting. About 7 liters of fluid are formed per day in the intestines of a healthy adult, and a certain part of it comes with food, but no more than 2% of these volumes are excreted with feces. Diarrhea can lead to dehydration very quickly.
Diarrhea and vomiting against the background of an intestinal infection in children are very dangerous. The younger the child, the faster it develops dehydration and the more difficult it is to restore fluid reserves. Already after 2 days from the onset of the disease, the child’s condition can become very serious. The situation is especially dangerous if an intestinal infection is accompanied by a high body temperature.
Although a person does not notice this, he loses fluid during breathing, and also when he sweats. When an individual is healthy, then the body completely keeps these processes under its control. The volume of water that a person drinks throughout the day is enough for him to make up for these losses (if he drinks in accordance with his age norm). When you are in the heat, with febrile conditions, with excessive physical exertion, the balance of water in the body may change.
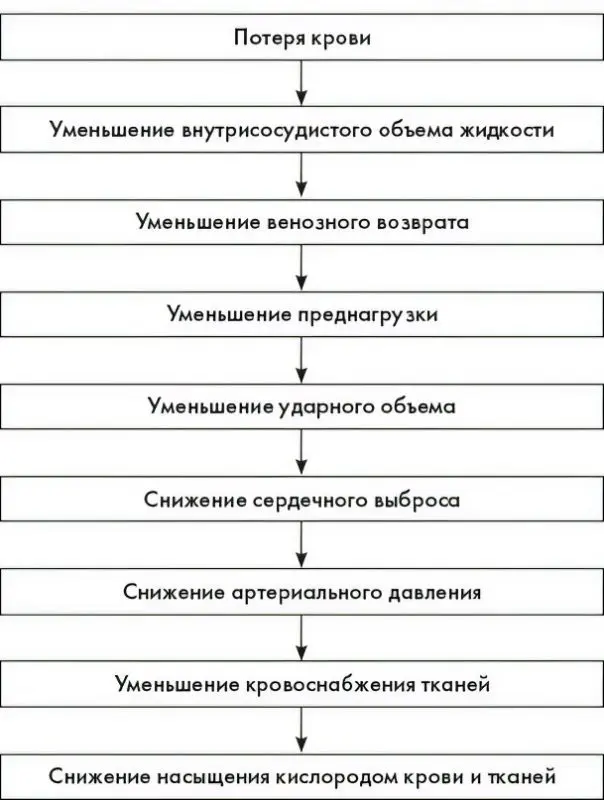
Blood loss is the most common cause of hypovolemia. Bleeding can be external and internal. First of all, blood loss affects the functioning of the heart.
This affects the body in the following way:
Blood pressure decreases, which leads to the supply of blood from reserve reserves – from the muscles and liver.
Urination is delayed to conserve fluid reserves in the body.
The blood clotting system is activated.
Small blood vessels spasm.
The body uses all these mechanisms to compensate for hypovolemia: it uses the blood depot, tries to keep it in large vessels due to capillary spasm, and activates the blood coagulation system to stop bleeding. This allows as long as possible to continue to nourish life-supporting organs with blood: the brain, heart and kidneys.
At the same time, the inclusion of such compensation mechanisms negatively affects the blood supply to peripheral organs. After all, they begin to suffer from hypoxia and acidification of the internal environment. Small vessels are more likely to form blood clots.
Provided that the person is not provided with emergency assistance, he will die from hypovolemic shock.
So, the mechanisms of development of hypovolemic shock are identical, regardless of the cause that provoked it. At first, the body tries to compensate for the existing violation by concentrating blood volumes in life-supporting organs, but over time, the blood flow decentralizes, which leads to disruption in the work of all organs. The state of shock, if it has come, progresses very quickly.
Hypovolemic shock is the terminal stage of hypovolemia. Very often, shock leads to irreversible consequences, is difficult to correct, causes serious changes in blood vessels and internal organs. Arterial pressure is greatly reduced, all tissues experience acute hypoxia. A person develops hepatic, ocular, cardiac and respiratory failure. The patient falls into a coma, which ends in death.
The picture below shows a graph of the development of hypovolemia with a blood peter:
Types and clinical picture of hypovolemia
Hypovolemia is divided into 3 main types:
Normocythemic. In this case, the volumes of circulating blood and plasma decrease, and these substances fall evenly relative to each other. This type of hypovolemia can be caused by bleeding, shock, and vasodilation.
Polycythemic. In this case, there is a loss of plasma, and blood cells remain unchanged. This type of hypovolemia is observed against the background of dehydration of the body, for example, with burn disease, diarrhea, vomiting, etc.
Oligocythemic. This type of hypovolemia is characterized by a decrease in the level of cellular elements in the blood, which is observed against the background of aplastic anemia or during hemolysis.
Sometimes the same disorder can cause various types of hypovolemia, so when a person receives burns, polycythemic hypovolemia may develop against the background of plasma sweating or oligocythemic hypovolemia against the background of severe hemolysis.
Symptoms that occur with hypovolemia are associated with a drop in blood pressure and developing tissue hypoxia. This leads to the fact that the internal organs are not able to function normally. Symptoms of the disorder will be the more intense, the more severe the hypovolemia. These include:
Hypotension.
Strong weakness.
Abdominal pain.
Dyspnea.
The skin of the face becomes pale or even cyanotic, the pulse and respiration rate increase. Depending on the severity of the patient’s condition, the work of the brain will be disrupted to some extent.
The skin loses its ability to normal thermoregulation, it becomes cool to the touch, the person himself freezes, but the thermometer can show high values. As the pressure drops lower and lower, the person becomes dizzy, and fainting may occur. In the future, without adequate assistance, shock and coma develop, and then the death of the body occurs.
In a child, hypovolemia can progress much faster than in an adult. This is especially true for children under 3 years of age. If a child develops severe diarrhea and vomiting, then he will quickly become apathetic, the skin will turn pale, the nasolabial triangle will turn blue. Fingers and the tip of the nose will become cyanotic.
Depending on the stage of development of the disease, the following symptoms of hypovolemia are distinguished:
With weak bleeding, hypovolemia will proceed in a mild degree. The pressure drops by no more than 10% of the usual indicators. The heartbeat slightly increases, the skin turns pale, dizziness occurs, the person is thirsty. He can feel sick, the patient’s condition is characterized as pre-fainting.
With moderate hypovolemia, blood loss will equate to 40%. At the same time, systolic pressure drops to 90 mm. rt. Art. The patient has severe shortness of breath, sticky perspiration appears, he often yawns, as the tissues suffer from hypoxia. Consciousness becomes clouded. The person is thirsty.
In severe hypovolemia, massive blood loss is observed – up to 70% of its total volume. The pressure drops to 60 mm. rt. Art., the pulse is frequent, but weak, the heartbeat is very strong, the skin is pale. At this time, many patients develop convulsions, confusion, and coma is possible.
After the onset of a severe stage of development of hypovolemia, shock can occur at any time. Low blood pressure causes loss of consciousness, or, conversely, psychomotor agitation. No urination, noisy breathing.
In the polycythemic type of hypovolemia, blood clots form in the vessels, and the tissues of the internal organs undergo necrosis against the background of a violation of their blood supply.
Treatment of hypovolemia

A person with signs of hypovolemia should be taken to the hospital. Depending on the severity of his condition and the cause that led to such violations, such specialists as: resuscitators, surgeons, infectious disease specialists will deal with the therapy.
Hypovolemic shock requires urgent measures already on the part of emergency doctors.
The algorithm for their provision:
Stop bleeding, if any.
Placement of a catheter in a peripheral vein.
The introduction of intravenous solutions to normalize the volume of circulating blood.
Providing normal breathing to the victim, oxygen supply.
The introduction of painkillers – Tramadol or Fentanyl.
The introduction of glucocorticosteroids – Dexamethasone, Prednisolone.
Provided that the described measures made it possible to normalize the pressure and it rose to the mark of 90 mm. rt. Art., the patient is urgently taken to the hospital. At the same time continue to carry out infusion therapy. If it is not possible to bring the pressure back to normal, then Phenylephrine, Dopamine, Norepinephrine are added to the intravenous solution.
First of all, the patient needs to restore the volume of circulating blood, which is possible through infusion therapy. This allows you to prevent the progression of hypovolemia and prevent shock from developing.
Drugs that are used to eliminate hypovolemia:
For infusion therapy: saline solutions, such as saline, frozen plasma, Reopoliglyukin or albumin.
To restore the qualitative composition of the blood, a platelet or erythrocyte mass can be transfused.
Intravenously served insulin or glucose in solution.
Corticosteroid hormones are administered intravenously.
Aminocaproic acid or etamsylate can be used to stop bleeding.
For the relief of seizures, Seduxen is indicated.
To prevent hypovolemic shock, Kontrykal is used.
If necessary, prescribe antibiotics.
It is imperative to control blood pressure, make sure that it does not decrease by less than 70 mm. rt. Art. At the same time, crystalloid saline solutions are administered to the patient. You should inject as much fluid as the person has lost blood.
If it is not possible to restore blood pressure with the help of solutions, then infusion therapy is supplemented with dextrans, preparations with starch and gelatin, plasma, vasotonics (Dopamine, Adrenaline, etc.).
In parallel, a person is allowed to breathe oxygen, or they are connected to a ventilator. Albumin and Heparin are administered in order to prevent blood from clotting, that is, to resist the process of blood clots.
It is possible that it will be necessary to eliminate bleeding by surgery, and interventions are also carried out with intestinal obstruction, peritonitis, pneumothorax and other conditions that require the help of a surgeon.
To eliminate hypovolemia, the patient is placed in the intensive care unit, which allows round-the-clock monitoring of the human condition. They control the electrolyte balance of the blood, hemostasis, blood pressure, the amount of oxygen in the blood, and the work of the kidneys. Depending on the data obtained, the treatment is selected and adjusted. Without fail, efforts are directed to the elimination of the cause that caused hypovolemia.









