Contents

Hypoxemia is a decrease in the level of oxygen in the blood. Hypercapnia is the accumulation of carbon dioxide in the blood. Both of these conditions develop under the condition that the inhaled air contains an insufficient amount of oxygen. If its level is not restored to normal, then hypoxemia and hypercapnia will provoke hypoxia. It is these two conditions that are considered the main symptoms that indicate the development of respiratory failure.
In the acute form, respiratory failure can be hypercapnic and hypoxemic. In the first case, respiratory failure develops with an increase in the level of carbon dioxide in the blood, and in the second case, an insufficient supply of oxygen to the blood leads to it. Often, a person with acute respiratory failure has both hypercapnia and hypoxemia, but it is important for the doctor to determine which condition prevails, since the tactics of managing the patient depend on this.
The pathogenesis of hypercapnia and hypoxemia
So, if the level of carbon dioxide in the blood is elevated, then a person is diagnosed with hypercapnia. With a decrease in the oxygen content in the blood, they speak of hypoxemia.
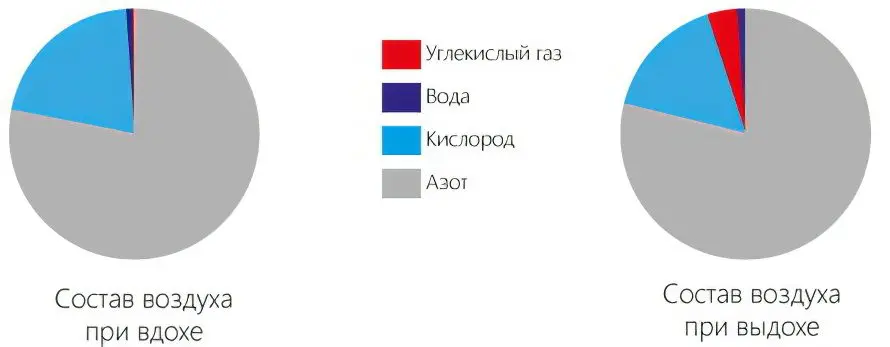
Oxygen, which enters the lungs along with the inhaled air, is carried with the blood flow throughout the body with the help of erythrocytes, binding to hemoglobin. Hemoglobin that carries oxygen to tissues is called oxyhemoglobin. When it reaches its destination, oxyhemoglobin gives up oxygen, after which it becomes deoxyhemoglobin, which can reattach oxygen, or carbon dioxide, or water. However, normally, in the tissues where hemoglobin has delivered oxygen, carbon dioxide is already waiting for it. It picks it up and brings it out of the tissues into the lungs, which, during exhalation, rid the body of carbon dioxide. The hemoglobin that carries carbon dioxide is called carbohemoglobin.
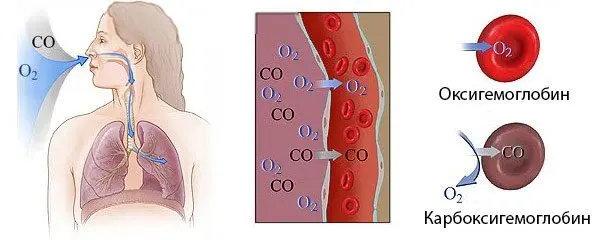
If we consider this process in the form of a diagram, then it will look like this:
Hb found in red blood cells + O2 from the air = HbO2 (this reaction occurs in the lungs, from which oxygen-rich hemoglobin is sent to the tissues).
HbO2> Hb + O2, while oxyhemoglobin gives oxygen to tissues.
Hb + CO2 (deoxyhemoglobin takes carbon dioxide from the tissues) = HbCO2 (this karogemoglobin is sent back to the lungs to get rid of carbon dioxide).
HbCO2 from tissues breaks down in the lungs into Hb and CO2. In this case, CO2 is removed, and Hb takes a new O2 molecule to again deliver oxygen to the tissues.
The cycle repeats again.
In this formula:
Hb – hemoglobin.
HbO2 is unstable oxyhemoglobin.
O2 is oxygen.
CO2 is carbon dioxide.
HbO2 is an unstable carbohemoglobin.
Such a reaction of the exchange of oxygen and carbon dioxide occurs on the condition that a person inhales clean air, in this case, the tissues do not experience oxygen starvation. However, it is known that reduced hemoglobin can attach any molecule to itself, since it does not have strong bonds. In simple terms, it attaches any component that it comes across. If there are few oxygen molecules in the lungs, then hemoglobin will take carbon dioxide molecules and send them to the tissues along with arterial blood. As a result, a person develops hypoxia, that is, oxygen starvation.
Hypoxia, hypoxemia and hypercapnia are the three symptoms that are characteristic of acute respiratory failure.
Causes of oxygen starvation of the body
Hypoxia can be caused by many factors.
However, depending on the nature of its origin, two types of hypoxic reactions are distinguished:
Hypoxia is exogenous. In this case, hypoxia develops as a result of the fact that the level of oxygen in the inhaled air becomes low. Therefore, human blood is not saturated with O2, which leads to oxygen starvation of tissues. Exogenous hypoxia develops in people who fly at high altitudes, climbers, conquerors of mountain peaks, scuba divers. Also, exogenous hypoxia develops in any person who inhales air with harmful inclusions.
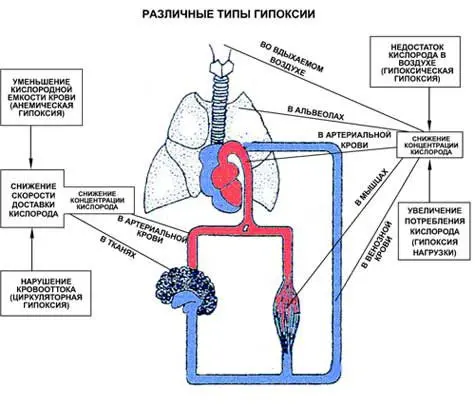
Hypoxia, which develops against the background of various pathologies of the respiratory or circulatory system.
Such hypoxia is divided into 4 subspecies:
Respiratory hypoxia, which manifests itself in violation of the function of external respiration. At the same time, the actual volume of ventilation of the alveoli per unit of time is lower than what the body needs. Respiratory hypoxia is caused by chest injuries, impaired airway patency, a decrease in the working surface of the lung tissue, inhibition of the respiratory center (against the background of taking medications, with pulmonary edema, with inflammation of the lung tissues). Respiratory hypoxia may be the result of diseases such as pneumonia, emphysema, pneumosclerosis, chronic obstructive pulmonary disease. It can also develop against the background of poisoning the body with toxic substances.
Circulatory form of hypoxia, which develops against the background of acute or chronic insufficiency of the circulatory system. Such disorders can lead to congenital heart defects, for example, an open foramen ovale.
Tissue hypoxia develops with poisoning. In this case, the tissues simply refuse to take in oxygen from the blood.
Blood hypoxia, which develops against the background of a drop in the level of red blood cells or hemoglobin in the blood. The most common cause is anemia, which is a consequence of acute blood loss or other pathological conditions.
Symptoms such as cyanosis of the skin, tachycardia, drop in blood pressure, convulsions, and fainting indicate severe hypoxia. With severe hypoxia, the patient rapidly develops symptoms of heart failure. If the victim is not provided with emergency assistance, he will die.
Causes and symptoms of hypercapnia

With hypercapnia, carbon dioxide accumulates in the tissues of the body and in the blood. The indicator of such accumulation of PaCO2. The level of this indicator should not exceed 45 mm. rt. Art.
Causes of hypercapnia can be as follows:
Violation of lung ventilation against the background of airway obstruction. Sometimes a person deliberately takes a breath less deep, for example, if during breathing he experiences pain (with a chest injury, with operations on the peritoneal organs, etc.).
Violations in the functioning of the respiratory center, which affects the regulation of respiratory function. This can occur with brain injury, with its destructive lesions, with drug poisoning.
Weak muscle tone of the chest, which happens in various pathological conditions.
So, the main pathologies that can cause hypercapnia are:
Acidosis.
Chronic obstructive pulmonary disease.
Atherosclerosis.
Infectious diseases of the respiratory system.
Also, the peculiarities of a person’s professional activity can cause hypercapnia. So, bakers, divers, steelworkers often suffer from it. An unfavorable ecological situation in the area where a person lives, inhalation of tobacco smoke and a long time spent in unventilated rooms can lead to excessive accumulation of carbon dioxide in tissues and blood.
Hypercapnia is indicated by the following symptoms:
Increased heart rate.
Difficulty in falling asleep. Daytime sleepiness.
Dizziness, headaches.
Increased intracranial pressure, up to cerebral edema.
Increased blood pressure.
Dyspnea.
Pain in the chest area.
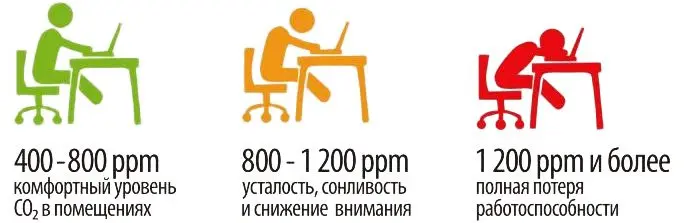
If the level of carbon dioxide in the blood significantly exceeds the permissible limits of the norm, then the development of hypercapnic coma is possible. It is dangerous by stopping the heart and breathing.
Causes and symptoms of hypoxemia

Hypoxemia develops when arterial blood is not saturated with oxygen in the lungs. The level of oxygen in the blood is indicated by such an indicator as PaO2. Its normal level is 80 mm. rt. Art., but no less.
Causes of hypoxemia:
Alveolar hypoventilation, which most often develops when there is insufficient oxygen in the air. However, other reasons may also lead to it.
Violations of ventilation-perfusion connections, which is observed in various lung diseases.
Right-to-left shunting, when venous blood enters the left atrium, bypassing the lungs. The cause of this condition is often one or another heart defect.
Violation of diffusion in the alveolar-capillary membrane.
Causes of impaired ventilation-perfusion connections in the lungs and diffusion capacity of the alveolar-capillary membrane
Gas exchange in the lungs is provided by ventilation of the lungs and blood flow in a small circle. But perfusion and ventilation occur in different proportions. So, some parts of the lungs are better ventilated, but not supplied with blood. In some areas, on the contrary, the blood is actively flowing, but there is no ventilation, for example, this is observed in the alveoli of the tops of the lungs. If there are many such areas that take part in gas exchange, but are not sufficiently washed with blood, then this entails first hypoxemia, and then hypercapnia. Such relationships are called ventilation-perfusion.
Violation of this ratio can be observed in the following cases:
Pulmonary hypertension.
Sudden loss of blood in large volumes.
Shock of various origins.
DIC syndrome with the formation of small blood clots in the bloodstream.
Pulmonary embolism.
Vasculitis.
The diffuse capacity of the alveolar-capillary membrane can increase and decrease depending on the specific circumstances. For example, what is the intensity of compensatory-adaptive mechanisms in a particular person during physical activity, with a change in body position, etc. The diffuse ability of the alveolar-capillary membrane begins to decrease in people after 20 years, which is a physiological norm for each person. Its significant decrease is observed in pathologies of the respiratory organs, for example, with pneumonia, with emphysema or obstructive pulmonary disease. All this becomes prerequisites for the development of hypoxemia, hypercapnia and hypoxia.
Signs of hypoxemia

Hypoxemia can increase rapidly or gradually.
Its symptoms are:
Cyanosis of the skin. The more intense it is, the lower the level of oxygen in the blood. If hypoxemia is weak, then cyanosis of the skin does not develop, the person just looks paler than usual.
Tachycardia or palpitations is a compensatory mechanism of the body, which thus tries to compensate for the lack of oxygen.
Drop in blood pressure.
Fainting, which develops with a decrease in the PaO2 index to 30 mm. rt. Art.
Insufficient oxygen content in the blood leads to the development of chronic fatigue syndrome, deterioration of memory and attention, sleep disturbance, night snoring, etc.
Treatment of hypercapnia and hypoxemia: what’s the difference?
These two conditions have a strong relationship; only a specialist can diagnose the prevalence of a particular pathological process. To do this, he will need to perform a blood gas test.
The general principles of therapy are:
Carrying out oxygen therapy, that is, the supply of oxygen through the respiratory tract. Its dosage is selected individually.
Performing artificial lung ventilation. This procedure is indicated in severe conditions, when a person is unconscious or in a coma.
Carrying out antibacterial treatment, prescribing drugs that promote bronchial expansion, prescribing diuretics and mucolytics.
If the patient’s condition is satisfactory, then he may be shown a chest massage, therapeutic exercises.
Be sure to start from the cause that led to hypercapnia or hypoxemia. Only in this way will it be possible to choose a truly effective therapy and reduce the negative impact of these conditions on the body.









