Contents
Endoprosthetics of the hip joint is one of the most modern methods of surgical treatment of diseases of the musculoskeletal system. During the operation, pathologically altered tissues of the structures that make up the hip joint are replaced with artificial prostheses.
Structure and function of the hip joint
The hip joint is considered the largest articulation of the bones of the human body. The loads that he has to experience in the process of life are very large. After all, it connects both lower limbs to the pelvis.
The following are involved in the formation of the hip joint:
The head of the femur is the spherical upper end of the thigh;
The acetabulum is a deepening of the pelvic bones in the form of a funnel, in which the femoral head is fixed;
Articular cartilage – soft cartilage tissue with a jelly-like lubricant that facilitates movement;
Intra-articular (synovial) fluid – a jelly-like mass that nourishes the cartilage and softens friction between the articular surfaces;
The ligamentous apparatus and joint capsule is a dense connective tissue that holds the articular surfaces and ensures the stability of the hip joint.
Muscles and their tendons, attached in the area of the hip joint, while contracting, provide movement in it. A healthy hip joint is quite mobile, and produces movements in almost all planes and directions. This range of motion is sufficient to adequately provide the function of support, walking and performing strength exercises.
Why is arthroplasty required?
It is quite natural that there should be strong indications for performing a hip replacement with an artificial prosthesis. They are based on such a destruction of the components of the joint, in which a person either experiences excruciating pain, or is unable to perform elementary movements with the affected limb. In other words, the joint ceases to correspond to its physiological purpose and becomes an unnecessary part of the body, as it sharply worsens the quality of life. In such cases, arthroplasty is the only way out of their situation.
Among the diseases that can provoke destructive changes in articular structures, the most common are:
Deforming osteoarthritis of the hip joint (coxarthrosis), which occurs simultaneously on both sides with grades 2 and 3 of the disease;
Coxarthrosis grade 3 with deformity of one joint;
Unilateral deforming arthrosis of the hip joint of 2-3 degrees in combination with ankylosis (complete immobility) of the knee or ankle joint of the affected limb;
The defeat of one hip joint with coxarthrosis of 2-3 degrees in combination with ankylosis of the same joint on the opposite side;
One- and two-sided ankylosis of the hip joints in Bechterew’s disease and rheumatoid arthritis;
Destruction of the femoral head (aseptic necrosis) due to trauma or circulatory disorders;
Traumatic injuries of the head and neck of the femur in the form of a fracture or false joint in persons over 70 years of age;
Malignant tumors in the ankle joint requiring surgical treatment. After resection of the tumor, one-stage arthroplasty is performed.
Contraindications to surgery

Unfortunately, people who need hip arthroplasty are not always able to perform such an intervention.
The main restrictions include:
Clinical cases when a person is unable to move independently for any reason. The performed endoprosthetics in them does not eliminate the existing defect and is therefore considered inappropriate;
Chronic pathology, which is in the stage of decompensation (heart failure, severe heart defects and arrhythmias, cerebrovascular accidents with neurological deficit, liver and kidney failure). The operation is associated with a high risk of exacerbating existing problems;
Chronic pathology of the lungs, accompanied by severe ventilation and respiratory failure (asthma, pneumosclerosis, bronchiectasis, emphysema);
Any inflammatory processes of the skin, soft tissues or bones in the area of the hip joint;
Foci of chronic infection in the body, requiring remedial measures;
Septic conditions and reactions. The operation is not performed even for those patients who have suffered sepsis for several years, since there is a high risk of suppuration of the prosthesis;
Paresis and paralysis of the limb to be arthroplasty;
Severe osteoporosis and insufficient bone strength. Such patients, even after a perfectly performed operation, can break the femur or pelvic bones during normal walking;
Severe cross-allergy to various medications;
Pathological conditions accompanied by the absence of a medullary canal in the femur.
Types and types of endoprostheses
The endoprosthesis, which will replace the pathologically altered hip joint, must have sufficient strength, reliability of fixation, high functional abilities and be sufficiently inert in relation to the tissues of the human body. All these requirements are met by products made of high-quality metal alloys, polymers and ceramics. As a rule, one endoprosthesis contains a combination of all these materials. This is due to the fact that in its appearance and qualities the product should resemble a human hip joint.
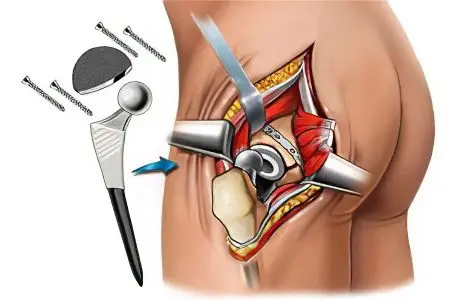
Its components are:
Endoprosthesis cup. This is the part that should replace the acetabulum of the pelvic bones. It is usually made from ceramic. But there are cups made of polymeric materials;
prosthesis head. It is a metal spherical part coated with a polymer. In this way, it is possible to achieve the most soft sliding when the head rotates in the cup of the prosthesis during the movement of the limb;
Leg of the prosthesis. It is made exclusively of metal, as it experiences the greatest loads compared to other parts of the endoprosthesis. If the head of the prosthesis imitates the head of the femur, then its stem replaces the neck and the upper third of the femur.
Another fundamentally important heading in the classification of products for prosthetics of the hip joint is their division into unipolar and bipolar. The first type is represented exclusively by the stem and head, which replace the corresponding structures of the femur. In this case, the joint will be represented by an artificial lower part and a natural acetabulum. Such interventions have been widely performed before. Due to poor functional results and a large number of destruction of the acetabulum with the failure of the endoprosthesis into the pelvic cavity, modern orthopedists practically do not perform such operations.
Bipolar endoprostheses are more often called total. This means that the composition of the product is represented not only by the part that prostheses the femur, but also by the cup that acts as the acetabulum. Such endoprostheses are perfectly fixed in the bone tissues and are maximally adapted, which significantly increases the effectiveness of the operation and reduces the number of complications. This is especially true when performing endoprosthesis replacement in elderly people with osteoporosis and in young physically active individuals.
Cemented and cementless arthroplasty

A very topical issue, both for specialists and for their patients, is the choice of a method for fixing the endoprosthesis. In this regard, everything is not so simple. After all, metal and ceramic materials must be firmly connected to the bones. Only under this condition is it possible to perform the functions of support and walking with a diseased limb.
Having determined the correct type of endoprosthesis and its size, the doctor selects the method of connecting the prosthesis with tissues during surgery, guided by the following tactical decisions:
Fixation of the endoprosthesis with cement – a special biological glue, which, after hardening, will firmly connect the bone tissues with the structures of the endoprosthesis;
Cementless fixation. These products have a special design and are arranged in such a way that on their surface there are many small protrusions, recesses, bumps and holes. Over time, the bone tissue grows into them, and the prosthetic bone becomes one with the endoprosthesis;
Hybrid or mixed fixation. It involves a combination of cement and cementless methods. In this case, the leg is fixed in the femur with cement, and the cup is screwed into the acetabulum.
Long-term observation of patients by specialists after such interventions made it possible to draw the following practical conclusions:
Cement when cooled creates a very high temperature. This leads to accelerated destruction of the surrounding bone tissue, which can cause the prosthesis to fail and fall into the pelvic cavity;
Cement fixation accelerates rehabilitation and reduces the recovery time of patients, but its use is limited in patients with osteoporosis and the elderly;
Cementless arthroplasty is associated with a lengthening of the full rehabilitation period. Patients must observe a limited motor mode for much longer due to the high risk of violation of the stability of the prosthesis;
The most optimal is arthroplasty by combined methods of fixing different parts of the product. This rule is the gold standard of treatment tactics for patients of all age groups.
Preparing for an operation

All patients in need of arthroplasty, and who have passed the necessary studies to determine the condition of the hip joint (X-ray, MRI, ultrasound), are also required to undergo a comprehensive examination. This is necessary in order to exclude the presence of possible contraindications.
The complex of diagnostic measures includes:
General clinical blood and urine tests;
Determination of blood glucose levels, and for people with diabetes – glycemic profile;
Biochemical blood test;
Determination of blood electrolytes (potassium, magnesium, sodium, calcium, chlorine);
Study of blood coagulation (coagulogram, prothrombin index, clotting time and duration of bleeding);
Determination of blood group and Rh factor;
Blood test for RV and Australian antigen;
ECG;
Study of the functions of external respiration;
X-ray examination of the lungs;
Consultations of narrow specialists in the presence of a corresponding chronic pathology.
Special preparatory measures before hip arthroplasty are not required. If no contraindications are found during the examination, the date of the operation is set. A light dinner is allowed the night before, but not earlier than 8 hours before the intervention. In the morning, the skin in the area of the hip joint and thigh is carefully shaved. Eating and drinking water is prohibited. Before transporting the patient to the operating room, an elastic bandage of the legs is performed, a prophylactic dose of an antibiotic is administered, and premedication is performed.
What happens during the operation?
After the patient is delivered to the operating room and placed on the operating table, anesthesia is performed. Usually, the method of anesthesia is chosen by the patient together with the anesthesiologist. Since the duration of the operation is from 1,5-2 to 3-3,5 hours, either spinal anesthesia or full-fledged combined anesthesia with controlled breathing and complete muscle relaxation are considered optimal. The first method is less harmful, therefore it is preferable for elderly patients.
After anesthesia, surgeons process the surgical field and access the hip joint. The size of the incision that passes through the central part of the articulation is about 20 cm. Then the joint capsule is opened and the femoral head is brought out into the wound. It is resected along the transtrochanteric line until the medullary canal is exposed.
The bone is modeled in accordance with the shape of the endoprosthesis, which is fixed in it in one of the optimal ways (most often with cement). Then the acetabulum is processed with a drill with a special nozzle in order to completely remove the articular cartilage from its surface. The prosthesis cup is installed and fixed in the prepared funnel.
The prosthetic surfaces are aligned and strengthened by suturing the dissected tissues. An active aspiration drainage is installed in the wound, through which the discharge will flow. A bandage is applied.
Possible complications

Endoprosthesis replacement of the hip joint refers to extensive and complex interventions.
Its complications can be:
Bleeding from a postoperative wound;
Formation of blood clots in the veins of the lower extremities with migration into the vessels of the lungs and pulmonary embolism;
Suppuration of the postoperative wound and endoprosthesis;
Hematoma of the operated area;
Failure of the endoprosthesis and its rejection;
Problems of the heart and brain in the presence of chronic pathology (CHD, atherosclerosis, dyscirculatory encephalopathy, etc.);
Dislocation of the endoprosthesis.
Real results
According to statistics based on long-term follow-up of operated patients and personal experience of leading specialists in hip arthroplasty, most patients are satisfied with the results of treatment. If the operation is performed in somatically healthy individuals of a relatively young age who do not have concomitant diseases, the functional abilities of the hip joint are almost completely restored. This allows a person to walk and engage in physical activity. Sports and movements associated with the power tension of the lower extremities are impossible. Patients are either unable to perform them, or in the course of execution, a violation of the integrity of the endoprosthesis occurs.
Like any operation, arthroplasty is not without complications and unsatisfactory results. They are mainly associated with advanced age, comorbidities and non-compliance with the treatment regimen by patients in the early and late postoperative period. More than 20% of operated patients expected better results from arthroplasty compared to those that were obtained.
Endoprosthetics using the MIS method – patient’s review









