Contents
Diaphragmatic hernia occurs due to the displacement of part of the esophagus into the chest cavity through the opening of the diaphragm. The frequency of occurrence is 2% of all cases of hernia, diagnosed after X-ray examination. In 5% of cases, a hernia of the esophageal opening of the diaphragm is detected when patients go to the doctor with complaints of gastrointestinal disorders.
Most often, a diaphragmatic hernia is asymptomatic, however, patients may experience signs of gastroesophageal reflux disease, heartburn, acid reflex, retrosternal pain. (Read also: Causes and symptoms of heartburn, how to get rid of heartburn?)
What is a diaphragmatic hernia?
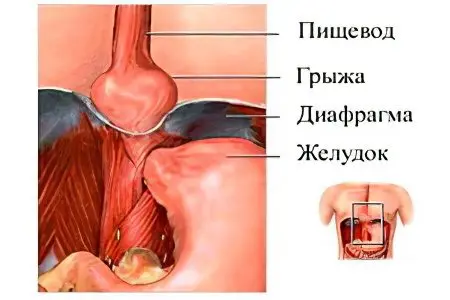
The diaphragm separates the chest and abdominal cavity, consists of muscles, is attached to the spinal column and ribs. The central part consists almost entirely of connective tissue, contains few muscle fibers and normally forms a dome, arching towards the chest cavity.
From the side of the spine, vessels and the esophagus pass through the diaphragm, for which there are holes in it through which protrusion of internal organs and the formation of a hernia can occur.
If part of the stomach exits through the diaphragmatic opening, there may be a malfunction in the esophageal valve, which separates the contents of the esophagus from the stomach. As a result, the acidic contents of the stomach can enter the esophagus, damaging its mucosa and provoking the development of esophagitis and other gastrointestinal pathologies, the symptoms of which are often manifested in diaphragmatic hernia.
Symptoms of hiatal hernia
With diaphragmatic hernias of a small size, there may be no clinical symptoms at all.
If the upper part of the stomach has entered the diaphragmatic opening, then the following symptoms may be observed:
Heartburn after each meal or with sudden changes in body posture, while bending forward;
Pain in the lower third of the sternum or in the hypochondrium;
Pain in the region of the heart, characteristic of coronary disease, radiating to the left shoulder and shoulder blade, which stop after a nitroglycerin tablet. At the same time, the ECG does not show violations of cardiac activity;
Complications of a hernia of the esophageal opening of the diaphragm make themselves felt by a number of symptoms that arise due to solaritis, perivisceritis and compression of the hernial sac:
Subfebrile fever and pain in the area of the xiphoid disorder of the sternum are characteristic of perivisceritis;
Epigastralgia, aggravated by pressure in the area of the solar plexus, is less pronounced when bending forward – signs of solaritis;
Dull pain in the epigastric region and behind the sternum, swallowing air and belching appear when the hernial sac is squeezed.
Other symptoms of hernia complications:
Dull retrosternal pain or tingling in the sternum;
Frequent belching of air or stomach contents, followed by a sour taste in the mouth;
Signs of stomach dyspepsia, violation of food digestion (Read also: Causes and symptoms of dyspepsia);
Intestinal disorders, symptoms characteristic of intestinal diverticulosis and duodenal ulcers;
Symptoms of inflammation of the pancreas and gallbladder; girdle pains characteristic of pancreatitis may occur; (See also: Pancreatitis – how does it manifest? What to do with an attack of pancreatitis?)
Heart rhythm disturbances – tachycardia, extrasystole; in some cases, the patient can be treated for a long time and unsuccessfully by a cardiologist with an erroneous diagnosis of angina pectoris or coronary heart disease.
In half of the cases, a hernia of the diaphragm is asymptomatic, 30% of patients go to the doctor because of symptoms of heart pathology caused by complications of the disease, and in 5-7% of cases, a hernia is diagnosed after an x-ray examination of patients with complaints of gastric disorders.
For the differential diagnosis of a hernia of the diaphragmatic opening of the esophagus, the following symptoms are important:
Pain after heavy meals or during physical exertion, aggravated by bending over and coughing;
The pain is more often manifested in a horizontal position of the body, disappears after vomiting and belching, moving to a vertical position, a sip of water or a deep breath;
Retrosternal pain is often dull and moderate, rather than sharp and severe.
The causes of pain in diaphragmatic hernia are compression of the nerves and vessels of the stomach when its cardial part enters the chest cavity, the effect of the acidic contents of the intestine and stomach on the esophageal mucosa and stretching of its walls.
Reasons for the development of diaphragmatic hernias
The esophagus passes through the diaphragm through its esophageal opening, at the site of its passage there is a thin membrane of connective tissue that separates two cavities – the chest and abdominal. In the abdominal cavity, the pressure is greater than in the chest, but normally the membrane withstands it, and only with dystrophic changes or congenital weakness of the connective tissues does it stretch and a part of the stomach or other parts of the esophagus is displaced into the chest cavity.
The mechanism of development of a hernia of the esophageal opening of the diaphragm is triggered by a combination of two factors – weakness of the connective tissues and increased intra-abdominal pressure. In addition, with dyskinesia of the digestive tract, traction of the esophagus may occur – it is pulled up and, with insufficiently developed connective tissues of the diaphragm, can provoke the formation of a hernia.
Factors that provoke a hernia of the diaphragm:
Weakness of the connective tissue that strengthens the diaphragmatic opening. The ligaments and connective tissues that strengthen the esophagus can weaken with age, losing their elasticity. Therefore, herniated diaphragm most often occurs in elderly patients over the age of sixty. In addition, the disease develops in people with flat feet and Marfan syndrome, with underdeveloped connective tissues from birth.
Chronically elevated intra-abdominal pressure. A number of factors can provoke increased pressure in the abdominal cavity: flatulence, constipation, chronic cough, excessive exercise. Increased intra-abdominal pressure alone cannot provoke a hernia of the diaphragm, however, if the ligaments are not strong enough, then under the pressure of the internal organs they can be deformed, the abdominal esophagus exits through the diaphragmatic opening with the formation of a hernial sac. In 50% of patients with chronic bronchitis, which manifests itself as a constant cough, a hernia of the diaphragm was found in varying degrees of severity. Other causes of increased pressure in the abdominal cavity are pregnancy, frequent vomiting, large neoplasms, and overweight.
Traction of the esophagus in concomitant diseases of the digestive tract.Functional disorders of the digestive system contribute to the development of hypermotor dyskinesia, pathology often develops with stomach and intestinal ulcers, inflammatory diseases of the gallbladder and pancreas. Longitudinal contractions of the esophagus with dyskinesia can pull it up, creating a load on the connective tissues of the diaphragmatic opening. Traction of the esophagus is also provoked by inflammatory and cicatricial processes of its mucosa, as a result of which it shortens, pulling up. If the tissues in the region of the diaphragmatic opening are not sufficiently elastic, the gastrointestinal tract exits into the chest cavity.
Congenital diaphragmatic hernia in children
Congenital hernia of the diaphragm is a severe surgical pathology in which newborns have a serious health condition with a threat to life. Prenatal diagnosis allows you to identify the disease even in the perinatal period and provide timely medical care to the child immediately after birth. For this, a pregnant woman is placed in a specialized center.
There are three forms of congenital diaphragmatic hernia – anterior hernia, hiatal hernia, and diaphragmatic hernia:
Anterior hernias are quite rare, their manifestations are noticeable already in the first month of a child’s life.
Hernia of the esophageal opening of the diaphragm is divided into true and false.
For a true hernia, the formation of a hernial sac is characteristic, while with a false hernia it is not.
Children with a false form of diaphragmatic hernia often die in the hospital, as the organs of the chest cavity are underdeveloped and cannot fully function. This is due to the exit of the abdominal organs into the chest cavity even during gestation. The stomach, intestines, spleen and, in some cases, the left side of the liver are displaced into the chest and squeeze its organs.
The causes of this pathology can be excessive physical exertion, which a woman was subjected to during pregnancy, chronic diseases of the respiratory system, smoking and other bad habits, malnutrition.
Symptoms of a congenital hernia of the diaphragm may be mild if the size of the defect is small. Only a few years later, the child complains of stomach pain, intestinal disorders, feel heartburn and constant belching after eating.
With a significant defect, the child may experience blood in the stool, lack of appetite, vomiting, swelling of the chest with a sunken abdomen, cyanosis of the skin.
prenatal diagnosis
Ultrasound examination shows an abnormal location of the organs of the chest cavity, which requires further diagnosis by echography. Sonography provides more detailed information about the organs of the chest, if anechoic formations are present in this area, then the doctor may suspect the exit of the stomach, intestinal loops or the left lobe of the liver through the diaphragmatic opening. Ultrasound can detect another sign of diaphragmatic hernia – the displacement of the heart to the right, but this symptom is not very pronounced in children in the perinatal period. Bilateral hernia of the diaphragm is very difficult to detect at this stage, often the disease is diagnosed only after childbirth.
Prenatal diagnosis allows you to take all the necessary measures to save the life of the child during childbirth. Children with congenital hernia of the diaphragm often die in the hospital, as this pathology interferes with the full formation of internal organs in the perinatal period.
Diaphragmatic hernia can be detected already in the first trimester of pregnancy, the earliest detection period is 12 weeks, however, in most cases, the pathology is detected at 26-27 weeks, due to the low quality of equipment and the lack of qualified specialists.
Another method of prenatal diagnosis that is used in conjunction with echography is perinatal karyotyping. It provides information about the degree of risk of developing congenital pathologies and hereditary diseases in a child.
What can not be done with a diaphragmatic hernia of the esophagus?

The rules of behavior for a patient with a diaphragmatic hernia should exclude the influence of factors that cause an increase in intra-abdominal pressure in order to prevent further displacement of organs into the chest cavity and the progression of the disease:
Patients are advised to follow a special diet that excludes foods that cause intestinal irritation;
Take food in fractional portions every few hours;
Avoid tilting the body forward, sudden changes in body position – this can cause pain in the sternum and heartburn;
You can not tighten the belt tightly, wear clothes that squeeze the stomach – this creates additional pressure in the abdominal cavity;
Avoid heavy physical exertion, but at the same time regularly perform physical therapy exercises that strengthen the muscle corset and restore the tone of the diaphragm;
Normalize stool – constipation and diarrhea increase intra-abdominal pressure and contribute to the formation of a hiatal hernia.
Before and after meals, it is recommended to drink a teaspoon of unrefined vegetable oil;
Pain and heartburn with diaphragmatic hernia intensify at night and become more pronounced when the body is moved to a horizontal position, therefore, before resting, it is necessary to refrain from eating – the last meal is at least three hours before bedtime.
Prohibited products for diaphragmatic hernia:
Alcohol and drinks containing caffeine – tea, coffee, soda;
Smoked meats, pickled foods, hot spices;
Sour-milk products (to minimize the amount) and sour fruit juices;
Peas;
Fresh bread and pastries – can be consumed dried.
Alkaline mineral waters, such as Borjomi, help to remove the manifestations of heartburn and restore the acid-base balance in the esophagus. The drug used to neutralize gastric juice in diaphragmatic hernia is Almagel. It is drunk on an empty stomach, 20-30 minutes before meals, two teaspoons at a time. Regular intake of the drug allows you to neutralize the negative impact of gastric juice on the walls of the esophagus and prevent the development of complications of diaphragmatic hernia.
Treatment of hiatal hernia
The most common symptom of hiatal hernia (occurs in 98% of cases) is retrosternal pain, usually dull and prolonged, rarely pronounced and intense. The main distinguishing characteristic is the strengthening with a change in the posture of the body, leaning forward, moving to a horizontal position.
Belching with acidic stomach contents, after which a specific taste and burning sensation in the mouth appears, as well as regurgitation of air, is another common (42%) symptom of diaphragmatic hernia.
Dysphagia, or difficulty swallowing, which is often aggravated by eating very hot or cold food, occurs in 31% of patients with diaphragmatic hernia. Dysphagia can manifest itself with hasty eating, its insufficient chewing. This symptom occurs due to inflammation of the esophagus, into which the contents of the stomach enter due to functional insufficiency of the cardia. Dysphagia indicates the development of a complication of diaphragmatic hernia – esophagitis.
Burning in the sternum, heartburn after a heavy meal, worse at night? also refer to the characteristic symptoms of diaphragmatic hernia.
Timely diagnosis and treatment of hiatal hernia is necessary to avoid dangerous complications of the disease – peptic ulcer of the stomach and intestines, bleeding of the part of the stomach that got into the hernial sac, gastroesophageal reflux disease, esophagitis, shortening of the esophagus and inflammatory-cicatricial processes.
There are two main approaches to the treatment of hiatal hernia – conservative therapy and surgical treatment.
Conservative treatment of hiatal hernia
Conservative therapy does not imply a complete correction of the hernia, but it alleviates its negative manifestations and is the prevention of complications from the digestive tract, in particular, it improves the condition of a patient with reflux esophagitis.
Conservative therapy is aimed at reducing the inflammatory process, preventing dyskinesia of the esophagus and stomach, which can provoke traction of the esophagus, as well as normalizing intra-abdominal pressure. Conservative treatment helps to normalize the pyloric tone, restore the function of the valve that separates the transition of the esophagus into the stomach. In the conservative therapy of diaphragmatic hernia, it is not drugs that come to the fore, but a set of therapeutic measures and rules that the patient must comply with.
Treatment measures include a special diet, the purpose of which is to reduce the load on the digestive organs, avoid intestinal irritation and increase the secretory activity of the stomach, as well as weight loss, since obesity is one of the factors that increase intra-abdominal pressure. Refusal of bad habits, adherence to the rules of a healthy lifestyle, limitation of physical activity are important components of the conservative therapy of diaphragmatic hernia.
Drugs that are used in the conservative treatment of hernia are designed to reduce the acidity of the stomach so that when its contents enter the esophagus, damage to its mucosa does not occur. These include alkaline mineral waters, anticholinergics (atropine, platifillin) and antispasmodic drugs (noshpa, papaverine).
Other medicines have an astringent effect, prevent inflammatory processes – these are solutions of burnt magnesia, bismuth nitrate, silver.
As part of the conservative treatment of hiatal hernia, antihistamines, antipsychotics and sedatives are used, physiotherapy is performed using novocaine in the epigastric region.
If all of the above methods are ineffective, then the patient is prepared for surgical treatment, which allows you to completely eliminate the pathology.
Diaphragm hernia removal

Surgical removal of a hernia is performed only in 10% of cases, for this there are such indications:
The size of the hernia is very large, under its pressure, the function of the lungs and cardiac activity are disturbed;
Diaphragmatic hernia provoked an anemic condition in the patient;
Hernia symptoms cannot be corrected with a therapeutic diet and medication;
Against the background of a diaphragmatic hernia, the patient developed peptic ulcer of the stomach or intestines, esophagitis, damage to the esophagus.
The operation consists in pulling the stomach and esophagus from the chest cavity, where they were displaced, into the abdominal cavity, after which the hernial ring (diaphragm defect) is strengthened by special methods.
The two main tasks of the surgical treatment of diaphragmatic hernia are the elimination of the hernial orifice and the creation of an antireflux barrier. Reflux disease develops due to dysfunction of the cardia – a valve that blocks the entrance to the stomach. When a part of the esophagus is displaced through the diaphragmatic opening into the chest cavity, the activity of the cardia is disturbed, the contents of the stomach enter the esophagus, irritating its mucosa and causing inflammation, and esophagitis develops. During the operation, the stomach is returned to an anatomically correct position, lowering it into the abdominal cavity, after which the diaphragmoesophageal ligament is strengthened.
There are two methods of operations used to remove a hernia and restore the functionality of the cardia – laparotomy and thoracotomy:
Laparotomy – an operation during which access is provided transabdominally (through the peritoneal approach),
Thoracotomy – an operation during which access is provided from the side of the chest – is used if the diaphragmatic hernia provoked pathologies of the respiratory and cardiac systems.
Also distinguish:
Transabdominal operations are more easily tolerated by patients (this is important to consider, since diaphragmatic hernia in most cases affects the elderly), while minimizing the severity of pain after surgery. Another important advantage of this operation is the ability not only to eliminate the hernia, but also to surgically treat other pathologies of the digestive tract – cholelithiasis, tumors and duodenal ulcers.
Transthoracic operations characterized by a longer rehabilitation period, during which severe pain may occur. However, thoracic access is necessary if, due to hernia and scarring, the esophagus is shortened and pulled up (traction).
Four groups of operations used for the surgical treatment of diaphragmatic hernia:
Strengthening the diaphragmatic-esophageal ligament and reducing the diaphragm defect;
Operations aimed at restoring the physiological angle of His;
Fundoplication – used to correct such a complication of diaphragmatic hernia as esophagitis, prevent the development of reflux disease while minimizing the risk of recurrence of the disease;
Gastrocardiopexy – the esophagus and stomach are fixed on the subdiaphragmatic structures, restoring the function of the cardia, which also contributes to the prevention of reflux disease.
Diaphragm hernia diet

Diet for diaphragmatic hernia is an important measure on which the successful treatment of the disease depends. The diet for this diet is designed in such a way as to fully supply the patient’s body with the nutrients necessary for tissue regeneration, but at the same time not cause irritation to the intestines and increased secretion of the stomach.
The secretory activity of the stomach increases after eating certain foods (spicy, salty, smoked and fried foods, red pepper, alcohol and sweet soda). With a hiatal hernia, the function of the valve that separates the contents of the stomach is disrupted, as a result of which gastric juice with concentrated acid can enter the esophagus, injuring its mucosa. This provokes heartburn, nausea and belching after eating, and in the long term can contribute to the development of complications of diaphragmatic hernia, provoke esophagitis.
The principles of building a diet for a hernia of the diaphragm:
Fast-digesting, protein-rich food that does not overload the stomach;
Products are subjected to thermal and mechanical processing, dishes must have a liquid, homogeneous consistency (liquid cereals, soups, purees, soufflés);
Drink plenty of water 7-8 glasses of water a day, mineral water with slightly alkaline properties;
Follow the diet without skipping meals, as this can cause bloating and nausea;
The daily diet is divided into 6 small portions, the last of which must be taken four hours before bedtime.
Fried, salty, sour, spicy and any foods that can cause intestinal irritation and increased secretion of gastric juice are excluded from the diet, including those to which the patient has an individual sensitivity.
Food should be taken in small portions, breaking its quantity not three, but into five or six meals a day. This is necessary so as not to create an unnecessary burden on the stomach and digestive organs, not to cause an increase in intra-abdominal pressure, which contributes to an increase in hernia.
The last meal is taken no later than four hours before going to bed. In the first half of the day, it is advisable to refrain from eating such products: milk and dairy products, fresh cabbage, legumes, corn. The use of legumes – peas and beans – is best minimized or completely eliminated from the diet. In addition, foods to which the patient is hypersensitive are removed from the diet – after taking, heartburn, belching, flatulence and bloating occur.
Drinking plenty of fluids is an important part of the diet for patients with diaphragmatic hernia. It is recommended to drink pure mineral water eight glasses a day, Essentuki-17 and Borjomi mineral waters are best suited for this.
Immediately after eating, you can’t exercise and expose the body to stress, however, it’s also not recommended to lie down – in a horizontal position, the patient often develops heartburn, as the contents of the stomach go into the esophagus.
The patient’s diet should be rich in proteins and essential fatty acids, for which it includes boiled chicken or beef, fish, eggs and cottage cheese, as well as vegetable oils – sunflower, linseed, sea buckthorn and fish oil, which are drunk in a spoon a day before meals.
Of the cereals, it is allowed to eat almost everything, except for rice. During the preparation of porridge, it is necessary to take one and a half times more water than usual, so that it turns out to be very soft and boiled. If the porridge is not soft enough and homogeneous, it is additionally crushed in a blender. It is also advisable to use other products in a crushed form – the meat is ground into minced meat and used to make meatballs and meatballs, and the fish is served in the form of a soufflé. Steamed or boiled, fried foods are completely excluded from the diet.
It is forbidden to use seasonings and sugar in dishes for patients with a hernia of the diaphragmatic opening, as this provokes an increased acidity of the gastric juice and creates risks for traumatizing the esophagus.
Traditional medicine recommends drinking decoctions of meadowsweet, sweet hernia and goose cinquefoil to alleviate the symptoms of hiatal hernia.
Fruits that are allowed in the patient’s diet – pears, bananas, peaches, apples can be eaten baked and without peel, since they are quite acidic when fresh and stimulate the secretory activity of the stomach.
With congenital diaphragmatic hernia, discovered during prenatal diagnosis, a diet for a pregnant mother is prescribed by a nutritionist together with an obstetrician.









