Contents
Herpetic infections are the most common human viral diseases and belong to the group of opportunistic infections. They cause maximum damage to people with imperfect homeostasis. First of all, herpes infections are dangerous for children, especially those with low immune status.
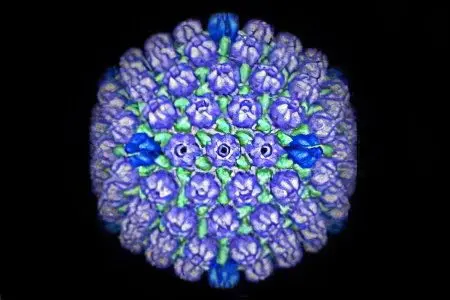
herpes virus in a child
Herpes viruses are intracellular parasites that are localized inside the cells of the nervous system of the body. To date, eight types of herpes pathogens are known to cause human diseases, these are viruses:
herpes simplex (nasolabial herpes), or the first type – HSV-1;
herpes simplex (genital herpes), or the second type – HSV-2;
chicken pox and herpes zoster, or the third type – HSV-3;
Epstein-Barra, or the fourth type – HHV-4;
cytomegalovirus, or fifth type – HHV-5;
the sixth type, or the sixth type – HHV-6;
the seventh type, or the seventh type – HHV-7;
the eighth type, or the eighth type – HHV-8.
Herpesviruses are the most common group of opportunistic infections. The name “opportunistic infection” means a disease that causes maximum harm during the period of a helpless state of the body (childhood, old age, in people with HIV, concomitant pathologies).

The localization of herpes viruses in nerve cells means their inaccessibility to many drugs and a peculiar pathogenesis.
Inaccessibility of herpesviruses. It is provided by a biological barrier around the nerves. Antibiotics of all known pharmaceutical groups, especially during the period of latent infection, do not overcome the blood-brain barrier, which greatly complicates the treatment;
The pathogenesis of herpesviruses associated with the localization of the virus:
in mild cases, these are rashes on the skin, mucous membranes along the nerves.
in severe cases, it is nerve damage (general cerebral, local nerve damage).
The causative agents of opportunistic infections are taxonomically heterogeneous, they are viruses, bacteria, and protozoa. Opportunists have common features that unite different nosological groups of diseases, including herpesviruses.
High contagiousness of pathogens. Herpes overcomes the body’s defenses in all ways of infection.
The latent (hidden) course of infection is provided by immunosuppression (suppression) of the virus, in particular:
at primary contact with herpes – cooperation of all parts of the immunocompetent organism (immunity is imperfect in children, sick adults);
after contact with herpes – the specific protective immunity of a healthy person (protective immunity is not developed enough in children, sick adults).
Damage to the body’s immune defenses makes it difficult to contain the development of the virus. The infection enters the stage of clinical manifestation. The pathogenesis of infection is directly proportional to the level of damage to the immune system. The immune system is most vulnerable in children with chronic diseases.
Against the background of the pathogenesis of an opportunistic infection, secondary immunity deficiency develops.
Herpesviruses, like all opportunistic infections, are a marker of the immunodeficiency state of the body, including in HIV infections.
Symptoms of herpes in a child

Herpetic infections differ in clinical polymorphism. Common, for almost all herpes, symptoms are defined as asthenic-vegetative syndrome.
Against the background of a variety of symptoms, the general clinical symptoms of herpes in children are often detected:
hyperthermia at the level of febrile indicators (38-390FROM);
headache;
fatigue, lethargy, irritability;
pain localized in the skin, joints, muscles.
The most common specific symptoms:
polymorphic skin rashes, the main type of rash is vesicles (vesicles);
damage to the lymph nodes, in the form of single or batch lesions;
damage to the mucous membranes;
organs of vision;
signs of damage to the nervous system (encephalitis, myelitis, encephalomyelitis).
More accurate information about the causative agent of herpes infection is obtained by laboratory methods. Confirmation is carried out using a combination of polymerase chain reaction (PCR) methods – detects the virus genome (including in the inactive phase), enzyme immunoassay (ELISA) – detects specific immunoglobulins IgM (early stage) IgG (reactivation).
Laboratory markers of primary infection:
the presence of DNA of the herpes virus being determined;
detection of specific Ig M antibodies to the virus being determined;
the absence of specific IgG antibodies to the virus being determined.
Laboratory markers of reinfection:
the presence of DNA of the herpes virus being determined;
detection of specific Ig M antibodies to the virus being determined;
early detection of specific IgG antibodies to the virus being detected.
Causes of herpes in children
The causes of herpes differ in the variety of triggers of the disease in children. Distinguish:
congenital, when the child’s body, due to genetically determined reasons, does not have protective antiherpetic mechanisms;
acquired as a result of a decrease in homeostasis after an illness, forced drug therapy aimed at suppressing immunity, and other reasons.
Herpes type 6 in a child

Herpes simplex virus type six (HHV-6) was first isolated in 1986. Primary contact with the virus registers at the age of 6 months to two years. By the age of three, specific antibodies to HHV-6 are detected in 100% of the examined, clinically healthy children.
Signs of herpes type 6 in children
The main signs of the clinical manifestation of HHV-6 in children:
high temperature (fever) above 390From more than two days;
there are no signs of a cold and / or intestinal infection;
sudden rashes on the body – baby roseola (one of the main symptoms) on the face, chest, abdomen, all over the body.
The following signs of the sixth herpes are possible:
convulsions against the background of high temperature;
acute tonsillitis – inflammation of the tonsils;
inflammation of the oral cavity, the mucous membrane is covered with vesicles (aphthae);
neurological signs.
During the initial clinical examination of the patient, the doctor has to take into account many factors that confirm the wide polymorphism of the clinical manifestations of opportunistic infections.
Symptoms of herpes type 6 in children
Symptoms that are clinical markers of HHV-6 and co-infections.
Convulsions in a child with a febrile temperature.
Febrile seizures, with HHV-6, may be signs of other childhood infections, for example, a combination of:
adenovirus infection, its combination with parainfluenza, influenza;
parainfluenza + HVS1,2;
HHV-6+ bacterial infections.
Tonsillitis
Acute inflammation of the tonsils (tonsillitis):
combination of HHV-6 + adenovirus + bacterial infection;
herpes Epstein-Barr.
Stomatitis
Stomatitis (inflammation of the mouth):
combination of adenovirus+HVS1,2;
HVS1,2.
Neurological symptoms
Neurological symptoms of the sixth herpes:
signs of meningoencephalitis;
cerebellar ataxia – a syndrome of “dancing” eyes;
hemiparesis.
Herpes in children on the lips

Herpes simplex (HVS-1) or herpes on the lips is characterized by blisters on the nasolabial area of the face. For a long time, the pathogenesis of the disease caused by herpes-1 was considered banal. After the introduction of modern methods into research practice, a significant effect of herpes on human health, especially children, has been proven.
In case of violations of cellular cooperation of immunity, a connection between HVS-1 and pathologies has been established:
upper respiratory tract;
gastrointestinal tract;
nervous system;
organs of vision;
reproductive system.
The most common form of infection is persistent (hidden). Activation of the virus occurs against the background of a decrease in the immune status, allergies, concomitant infections. Reactivation is possible at any age.
Signs of herpes simplex on the lips in children
Signs of an uncomplicated manifest form of herpes simplex on the lips in children
vesicular rashes on the lips and nasolabial triangle;
rashes on the mucous membranes of the oral cavity;
temperature rise to febrile values 38-390C.
The addition of signs of rashes in other parts of the body, symptoms of toxicosis – depression, lethargy, signs of encephalomyelitis – evidence of a combined infection, the development of severe pathogenesis.
Lethal outcome in severe forms of pathogenesis reaches 50-80%. After promptly provided medical assistance, the virus passes into an inactive, persistent form of infection.
An unfavorable course of HVS-1 children is considered to be recurrence of the disease from 2 to 4 times a year, an acceptable level of infection is a single exacerbation per year, a favorable course of infection if herpes is recorded less than once every two years.
Herpes on the face in children
Rashes on the face of a child accompany diseases such as:
herpes simplex (HVS1,2);
herpes zoster (HHV-3);
chicken pox (HHV-3);
other viral, bacterial infections – scarlet fever, impetigo, congenital syphilis;
allergic pathologies.
The most common pathology of childhood is chicken pox. The infection rate of children with the HHV-3 virus is very high, reaching 1 per 100. The main mode of transmission of infection is airborne. A perinatal route of infection is possible. The incubation period is 10-21 days. After an acute period of illness, the herpes-3 virus goes into an inactive state.
Persistence in the nerve nodes is lifelong. Reactivation of the herpes-3 virus causes a disease called herpes zoster.
In infants, the primary disease is mild. School-age children, adults at the initial contact with the virus, children of all ages with a low immune status are seriously ill.
Signs of chickenpox in children of different ages
Vesicular eruption on the face, then all over the body.
Itching is characteristic of pathogenesis, children over three years old – 70%, infants – 15% of cases.
The disease in infants is manifested by mild catarrhal syndrome (hyperthermia 37-380C for 2-3 days, redness of the mucous membrane of the throat, cough, runny nose).
The disease of children older than three years is manifested by severe infectious toxicosis (hyperthermia 38-390C within 4-5 days, weakness, lethargy, headache, runny nose. On the 3-7th day, from the moment the rash appears, signs of impaired consciousness, auditory hallucinations, and other signs of damage to the nervous system may appear).
The debut of a rash with chicken pox. – Small scarlet-like spots on the first day of the disease against the background of fever. The polymorphism of the rashes is characteristic, that is, at the same time there are different stages of the rash from the primary ones – papule, vesicle; to the secondary – crust. This is due to the constant process of formation, maturation, disappearance of the rash.
Characteristics of vesicles on the face in children
Vesicle – a rash with transparent contents, the main type of rash in herpetic infections. Other possible types of rashes on the face, in this case, are not taken into account.
Herpes simplex (HSV-1) – localization of vesicles in the area of the nasolabial triangle of the face.
Herpes zoster (HHV-3) – vesicles tend to coalesce into a single focus, characterized by severe soreness of the rash.
Chicken pox (HHV-3) – solitary foci, vesicles are scattered over the face, body.
Allergic rash – areas of redness around the rash, severe itching.
A rash with bacterial infections is, first of all, pustular rashes – pustules. Pustules in viral and allergic appear as a secondary pathological process after the seeding of skin scratches with pyogenic bacteria.
Shingles in children

There are isolated reports of the reactivation of Varicella zoster virus and the illness of children, the younger age group, with herpes zoster, the causative agent HHV-3.
Causes of herpes zoster in children of the first years of life – chickenpox:
child in the first year of life;
mother during pregnancy.
The main differences between herpes zoster in children
The course of uncomplicated herpes zoster in children is characterized by:
mild form of pathogenesis;
the absence of acute pain in the area of rashes;
the absence of residual pain after the disappearance of the rash.
In adults, the zoster virus causes more severe manifestations, accompanied by severe pain, often persisting for a long time after discharge from the hospital.
Severe pathogenesis of herpes zoster may be in children with low immune status.
There are such signs of herpes zoster in children:
Vesicular rashes are characteristic:
vesicles with a clear liquid on the cheeks, torso;
usually on one side of the face, body;
the rash is prone to association;
Vesicular rashes in children can form against a background of normal temperature. The appearance of herpes zoster in children is associated with the immunosuppressive effect of other types of herpes viruses (Epstein-Barr, cytomegalovirus).
Herpes zoster in children with immunodeficiency
It is characterized by a persistent course of pathogenesis, with pain during the formation of rashes, after the end of pathogenesis. In about 5-15% of children, motor nerves are involved in the pathological process, with consequences in the form of paresis and paralysis that pass after a while. Pathogenesis, accompanied by necrosis of areas of the skin in places of the rash. Persistent relapses of herpes zoster are a reason to suspect the child’s immunodeficiencies.
Shingles of pregnancy
The disease is complicated by pneumonia, encephalitis. The presence of an established infection is the basis for hospitalization in order to preserve the bearing of the fetus.
Genital herpes in children
HVS-2 is the second serotype of the herpes simplex virus, primarily affecting the mucous membranes of the external genital organs.
The herpes virus-2 belongs to the group of sexually transmitted diseases. Infection with the HVS-2 virus is possible, before puberty, at the stages of embryogenesis, human ontogenesis. The following ways of transmission of herpes-2 from mother to fetus are proven:
transcervical – infection through the amniotic fluid;
transplacental – penetration through the bloodstream of the umbilical vein;
transovarial – infection through the fallopian tubes;
contact – infection during childbirth.
The greatest susceptibility to herpes-2 in children aged 5 months to 3 years, adults -16-25 years. Primary contact with the virus in 80-90% is not accompanied by clinical manifestations. Infection of children before puberty HVS-2 occurs through household contact – underwear, shared towels.
There are such signs of genital herpes in children:
vesicular rashes of the mucous membranes of the external genitalia;
itching, pain in the area of rashes;
hyperthermia 37-380C.
Rashes of genital herpes can appear on the nasolabial triangle, other parts of the body. Genital herpes is prone to relapse. More than 50% of initially infected children are ill again. The frequency of virus reactivation depends on the state of the immune system.
Genital herpes in the clinical stage can occur in:
mild abortive form – up to 90% of all cases of exacerbation of genital herpes;
severe form – up to 10%.
A severe form of genital herpes is accompanied by deep erosions on the mucous membranes of the external genital organs. In severe pathogenesis, the brain of its membrane is affected. Similar lesions can also occur with HSV-1 and other types of herpes.
Genital herpes, in a clinical form, of a pregnant woman ends with abortions:
early terms – 55% of cases;
late terms – 25% of cases.
Clinical forms of genital herpes in newborns
Infection of the fetus on the eve of childbirth is accompanied by a disease in the first hours after childbirth. Infection of the fetus during childbirth is accompanied by a disease of the newborn within two weeks from birth.
There are three forms of genital herpes in newborns:
Localized. (20-40% of HVS-2 disease in newborns). Damage to the skin, mucous membranes of the mouth, eyes. Rash in the form of single vesicles, hyperemia, edema, on the 5th-14th day of the child’s life. If infected at the end of pregnancy, the newborn may be born with a rash. The most dangerous localization in the eye area, damage up to corneal ulcers and atrophy of the optic nerve.
Generalized. (20-50% of newborn HVS-2 cases). The pathogenesis develops 5-10 days after birth. Manifested by septic phenomena (lethargy, regurgitation, respiratory failure, cyanosis, vesicles on the skin, rashes on the mucous membranes, yellowness of the mucous membranes, convulsions, coma). Lethality 80-90%.
Brain damage. (up to 30% of HVS-2 diseases in newborns). Occurs 2-3 weeks after birth. The rapid increase in symptoms (temperature rises, lethargy, alternates with agitation, vomiting, trembling, convulsions, coma). Mortality 50% within 6-7 days.
Herpes in the throat of a child

Herpes in the throat, sometimes referred to as infectious mononucleosis, which is characterized by fever, lesions of the mucous membranes of the pharynx, lymph nodes. The disease is multifactorial. The causative agent of infection can be one of the herpes viruses, as well as other viruses, bacteria, protozoa in the form of mono-and mixed infections.
The main causative agents of infectious mononucleosis:
herpes type IV – Epstein-Barr virus (EBV) – was previously considered the only pathogen;
herpes type V – cytomegalovirus (CMV) – a common pathogen;
herpes type VI – (HHV-6);
herpes I and II types – herpes simplex virus (HVS-1,2);
various combinations of herpes viruses I, II, IV, V, VI types;
adenoviruses;
bacteria;
the simplest.
A variety of pathogens causes a variety of symptoms of infectious mononucleosis. Clarify the diagnosis with the help of laboratory tests – ELISA, PCR. The most promising is the immunohistocytochemical method (IHC).
There are the following typical symptoms of herpes in the throat of a child:
body temperature from 38 to 390WITH;
inflammation of the pharyngeal tonsil – difficult nasal breathing;
angina – inflammation of the palatine tonsils, pain when swallowing;
enlarged regional lymph nodes;
rashes on the body.
Infectious mononucleosis does not have a pathognomonic symptom, the primary signs resemble (ARI, tonsillitis, adenoiditis).
Infectious mononucleosis is more often recorded in the cold season, about 70% of cases. Among children of the first years of life, boys are more likely to get sick. The approximate ratio of sick infants, boys – 72%, girls – 28%. In adolescence, 10-15 years old, the ratio changes, which is probably due to the hormonal characteristics of different sexes. The approximate ratio of the incidence of infectious mononucleosis in adolescents, girls – 66%, boys – 34%.
In the first year of life, the incidence is low, due to the presence of maternal antibodies in the blood of infants. At the age of 2-3 years, the incidence increases sharply. It stabilizes in the population of preschool and primary school age at the level of 1,2 cases per 100 children. The next two-fold increase in the incidence is recorded in adolescence (10-15 years and older). Due to the formation of sexual activity at a young age. Infectious mononucleosis is sometimes called the kissing and student disease.
Causes of infectious mononucleosis
The disease can develop according to the type of primary contact or occur under the influence of internal and / or external factors according to the type of virus reactivation. It was noted that some time before the disease, about 1/3 of the children were examined by a pediatrician for tonsillitis, otitis media, adenoiditis, and herpetic stomatitis. In half of the families with a child with infectious mononucleosis, there are frequent (more than 4 times a year) herpetic diseases.
The most common cause of infectious mononucleosis for all age groups of children is:
mixed infection – approximately 60%
monoinfection – approximately 40%.
Among the causes of monoinfection, the following herpes viruses mainly predominate:
Type IV (EBV) – more than half of the cases of diseases;
Type V (CMV) is a frequently reported cause;
I and II types (HVS1,2);
Type VI (HHV-6).
In the structure of mixed infection in adolescents, a combination of:
EBV+HVS-1,2 – about half of the cases;
VEB + CMV is a common combination.
The pathogenesis of infectious mononucleosis

The most likely trigger is another infection. A severe pathogenesis of herpes combinations in infectious mononucleosis has been established.
VEB + HVS-1,2. It is characterized by a sudden onset, moderate fever, severe intoxication (drowsiness, lethargy), swollen lymph nodes, rapid development of lacunar or ulcerative necrotic tonsillitis, and sore throat. Such symptoms are not typical for mono-EBV and HVS-1,2 infections. It was noted that the fever of the mixed form of infection in comparison with mono-infections of EBV, HVS-1,2 persisted:
9-10 days for mixed infection;
5-7 days for mono-infection with EBV or HVS-1,2
VEB+CMV. It is characterized by pathogenesis in the form of:
swelling of the nasopharyngeal mucosa;
intense hyperemia;
hypertrophy of the tonsils II-III degree
duration of fever – about 13 days – mixed infection, about 5 days – mono infection.
Treatment of herpes in a child
For the treatment of various types of herpes infections, there is no single tactic, treatment regimen. Therapeutic methods are determined individually in each case.
Treatment for sick children includes:
etiotropic treatment during the period of initial contact and reactivation of the virus (specific antiviral drugs of different groups, immunopreparations).
immunorehabilitation during the latent course of infection, with frequent relapses, with the help of fractional courses of immunomodulators that can compensate for the damaged link in the body’s defense
preventive therapy of relapses (medication, physiotherapy, adaptogens, restoration of bifidobacteria biocenosis)
In therapy, antiviral drugs, specific and non-specific immunomodulators that affect individual parts of the immune system, immunoglobulin drugs, immunomodulators are used.
Culture vaccine (inactivated herpes simplex virus type I and II)









