Contents
Vasculitis is a whole group of diseases that are accompanied by damage to the vascular wall. Vasculitis differs depending on the cause of their occurrence and the mechanism of development.
About 40% of all patients diagnosed with vasculitis are people under the age of 20 years. Hemorrhagic vasculitis in children is found in the period from 5 to 14 years. Most often, men suffer from the disease.
Hemorrhagic vasculitis – what is it?

Hemorrhagic vasculitis is an acquired disease that is accompanied by damage to capillaries, venules and arterioles. Inflammation has an aseptic course, but always leads to damage to the vessel wall and contributes to the rapid formation of blood clots. With hemorrhagic vasculitis, the vessels that nourish the skin and parenchymal organs suffer. Inflammation leads to the fact that elements of the rash appear on the dermis. Therefore, vasculitis is called rheumatoid purpura or allergic purpura.
The disease was first described 2 centuries ago by the doctors Shenlein and Henoch. Therefore, hemorrhagic vasculitis is sometimes called Henoch-Schonlein disease.
Causes of hemorrhagic vasculitis
Scientists continue to argue about the causes of the development of hemorrhagic vasculitis. It is believed that the disease most often develops in people prone to allergies. Under the influence of a number of factors, immunity stimulates the body to produce immune complexes. They are in the blood, accumulate in the vessels that feed the skin and internal organs. These complexes damage the walls of blood vessels, blood elements seep through these damages and remain in the surrounding tissues. Therefore, the patient has a hemorrhagic rash on the skin.
Vasculitis of the hemorrhagic type can occur for the following reasons:
Transferred infections. The danger is represented by herpes viruses, influenza, SARS, mycoplasma bacteria, mycobacterium tuberculosis, staphylococci and streptococci, parasites (Trichomonas and helminths).
Setting up vaccines.
Serum administration.
Insect bites.
Allergy to food.
Burn disease.
Subcooling the body.
Risk factors that increase the likelihood of developing vasculitis include:
Old age.
Childbearing period.
Frequent infectious diseases.
Tendency to allergies.
Received injuries.
Classification of hemorrhagic vasculitis
Depending on the symptoms that vasculitis gives, the following varieties are distinguished:
Simple form (cutaneous vasculitis).
Skin-articular vasculitis.
Renal form of the disease.
Abdominal vasculitis (disturbances from the digestive organs prevail).
Mixed form of the disease.
The course of the disease may vary:
Acute vasculitis. Within a month, the disease is gone.
Subacute course of vasculitis. In this case, the disease lasts 3 months.
Protracted vasculitiswhich lasts 6 months.
recurrent vasculitis. In this case, for several years the patient has 3-4 episodes of inflammation.
Chronic vasculitis. Periods of remission in this form of the disease are replaced by periods of calm.
Fulminant course of the disease. This form of vasculitis develops in children under 5 years of age. The disease lasts for several days.
Depending on the severity of the pathology, there are:
Vasculitis of the first degree. The person feels normal, body temperature does not rise, or may rise, but only slightly. The rash is not intense, there are no other symptoms of the disease. In the blood test, the ESR index is increased, but not more than up to 20 mm / h.
Vasculitis of the second degree. The patient’s state of health is disturbed, the rash is intense, the body temperature rises to 38 °C. The patient complains of headache and muscle pain, severe weakness appears. A person is diagnosed with disorders of the digestive and urinary systems. ESR can reach 40 mm/hour. The level of blood albumin falls, and the number of eosinophils and leukocytes grows.
Vasculitis of the third degree. Intoxication of the body is strongly expressed. There are pathological symptoms from the joints, kidneys, gastrointestinal tract. Often the central nervous system, the peripheral nervous system is involved in the inflammatory process. ESR increases to 40 mm/h, leukocytes are greatly increased, and platelet levels are falling. The patient develops symptoms of anemia.
Symptoms of hemorrhagic vasculitis

The manifestation of vasculitis is acute, the patient’s body temperature increases. Most often this happens after 14 days from the infection.
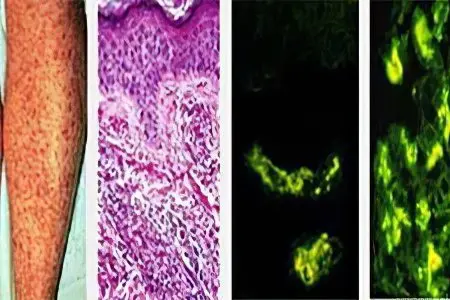
Skin manifestations
The rash appears in the early stages of vasculitis. It has a hemorrhagic character and looks like bubbles. They can spread throughout the body in spots or dots. Their sizes vary, they are 1-5 mm in diameter. When pressing on the elements of the rash, they do not disappear. As the pathology progresses, the rash will merge.
Rashes rise above the surface of the dermis. The maximum number of spots is observed on the extensor surfaces of the limbs. The rash appears on the buttocks and in the area of large joints. Sometimes it affects the face, chest, stomach, back.
Before the rash appears on the skin, it may itch. After a few days, the rash becomes pale. After their disappearance, age spots remain on the dermis.
Some elements of the rash disappear, and new ones appear. This leads to the fact that the dermis becomes variegated. The rashes are symmetrical. The more severe the vasculitis is, the more intense the rash will be.
Sometimes a zone of necrosis appears in the center of nodules or spots. Then a scab is formed at this place, which disappears. This leads to the fact that after the resolution of the element of the rash, the dermis is covered with scars.
Joint damage
Joints are affected in 70% of patients. The person complains of pain and inflammation. First of all, the knees, ankle and wrist joints suffer. If a rash appears on the skin, the pain becomes stronger.
The joints themselves swell and can become deformed. This leads to a limitation of their functioning. The dermis over the joints is inflamed, at first it turns red, and then becomes bluish in color.
The deformity of the joint is reversible, since the inflammation does not persist for more than 7 days.
Abdominal syndrome
About 50% of patients suffer from abdominal syndrome. It is manifested by multiple hemorrhages in the intestines and in the abdominal wall. The pain occurs in attacks, proceeds as intestinal colic. Patients often suffer from vomiting and diarrhea. Blood is visible in the feces and vomit. The pain is concentrated in the navel, and sometimes spreads to the entire abdomen.
The skin becomes pale, the eyes sink, the patient’s tongue is dry, facial features are sharpened.
To reduce the intensity of pain, a person lies on his side and presses his legs to his stomach. Sometimes exacerbation of the disease leads to intestinal intussusception or intestinal obstruction. Less often there is a perforation of the appendix with peritonitis. After 2-3 days, the abdominal syndrome disappears on its own.
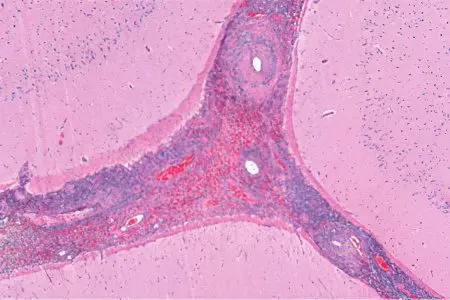
Kidney damage
Vasculitis often leads to kidney damage. They form blood clots, which cause the development of glomerulonephritis. There is blood in the urine. It is possible to identify it during the analysis. The person complains of edema.
Kidney damage does not occur immediately. Organs suffer within a year after the manifestation of vasculitis. Renal syndrome is observed in 40-60% of patients.
Other symptoms of vasculitis
The spinal cord and brain are not often damaged. Even less often, a person develops pneumonia and myocarditis.
Anemia
Anemia is a complication of vasculitis. The patient has low hemoglobin in the blood. He complains of increased fatigue and weakness, fainting may occur. “Flies” flash before the eyes.
pregnancy and vasculitis
Pregnancy can cause the development of vasculitis. It is the trigger of the antiphospholipid syndrome. For pregnant women, this can be dangerous, as it affects the development of the fetus. It also increases the likelihood of miscarriage, the onset of early labor and placental abruption.
In order to reduce the complications of pregnancy, women with vasculitis are prescribed blood-thinning drugs (Aspirin and Heparin).
Vasculitis in children
In children, the disease often occurs without the appearance of a rash. This makes it difficult to make a diagnosis. Children complain of joint pain and abdominal pain. Pathology has an acute course, develops unexpectedly.
If a rash appears, it covers the entire body and looks like subcutaneous bruising. The disease often recurs. In childhood, the likelihood of developing Quincke’s edema increases.
Diagnostics

Standard diagnostics begins with an examination of the patient and with the collection of anamnesis. The doctor analyzes the information received and correlates it with the clinical manifestations of the disease.
Then he directs the patient to take tests:
Changes in the general blood test: an increase in the level of leukocytes and neutrophils, a drop in the level of hemoglobin and erythrocytes. ESR is growing. The intensity of changes in the blood picture depends on the severity of the course of the disease.
Changes in the general analysis of urine: the detection of erythrocytes, protein and cylinders in it.
Changes in the biochemical analysis of blood: the level of fibrinogen, haptoglobulin, sialic acids, alpha and gamma globulin increases.
When conducting a urine sample according to Zimnitsky, its density will be reduced.
Blood may be found in the stool.
The coagulogram remains unchanged.
An immunological study reveals the growth of class A immunological complexes. An increase in C-reactive protein is also likely. It is important to conduct a blood test for hepatitis, as these viral infections can cause the development of vasculitis.
In addition to laboratory tests, the patient is referred for instrumental diagnostics:
Ultrasound of the kidneys, abdominal organs.
Biopsy of the kidneys and skin.
FGDS, colonoscopy, bronchoscopy.
Auxiliary methods of examination are:
Pinch test. When pressing on the skin, the patient develops bruises.
Test using a tourniquet. Subcutaneous bruising is formed when a tourniquet is applied to the shoulder.
Cuff sample. After applying the tonometer cuff, the patient develops subcutaneous hemorrhages.
Treatment of hemorrhagic vasculitis
Treatment of vasculitis is within the competence of a rheumatologist. If the patient develops lesions of other organs, then he is shown a consultation of narrow specialists. When the disease recurs, the patient is admitted to the hospital. At the time of exacerbation of vasculitis, a person must observe bed rest. This prevents the development of complications.
Among the medicines used:
Enterosorbents. They allow you to quickly remove harmful substances from the body.
Anticoagulants. Drugs aimed at preventing the formation of blood clots by improving blood circulation in small vessels.
Antiplatelet agents. Drugs that thin the blood, prevent the formation of blood clots, do not allow it to clot.
Antihistaminesthat stop allergic manifestations.
Glucocorticosteroids. They quickly stop inflammation, but do this at the expense of immune suppression.
Additional treatments:
Drugs from the group of NSAIDs. They allow you to reduce body temperature, reduce the intensity of pain and inflammation. Diclofenac, Indomethacin, Ibuprofen are prescribed for joint damage.
Vitamins A, E, group B make the vascular wall stronger, thereby reducing the likelihood of bleeding.
Cytostatics inhibit the activity of the immune system. These drugs are prescribed for severe illness.
Blood transfusion and blood purification will help relieve the symptoms of vasculitis.
Calcium preparations make it possible to compensate for the deficiency of this microelement in the body.
Symptomatic therapy. Relieve muscle spasm allow drugs such as Papaverine and No-shpa. To minimize damage to the gastric and intestinal walls, the patient is prescribed antacids (Almagel, Maalox). They lower the acidity of the stomach.
Severe complications, such as peritonitis or intestinal perforation, require surgical intervention.
Hypoallergenic diet for vasculitis
All patients with vasculitis must follow a diet. Foods that can provoke an allergic reaction are removed from the menu. The ban includes eggs, coffee, chocolate, citrus fruits, nuts, fish and seafood.
Fatty and fried foods are not consumed during the acute period of the disease. The menu is based on low-fat products. You can eat green apples, cereals, rabbit meat, turkey.
Forecast
If the disease has a mild course, then the prognosis is favorable. In other cases, it gets worse. There is a possibility of developing severe complications: inflammation of the kidneys, kidney failure. The fulminant form of the disease can cause rapid death of a person.
Registration for dispensary registration
Adults with vasculitis are not registered in the dispensary. The rheumatologist observes children for 2 years. In the first 6 months, the doctor should be visited 1 time in 30 days, the next 6 months – 1 time per quarter. Then the doctor is treated once every six months.
A child who has had vasculitis is limited in physical activity, he is prohibited from physiotherapy and spending a lot of time in the sun.
Complications
Vasculitis is associated with the risk of developing intestinal obstruction, peritonitis, and renal failure. Sometimes the heart, liver suffers, bleeding in the lungs can occur. Children have hemorrhagic diathesis.










Salam menim qizim uc ay qabaq vaskulit kecirdi sebebinj bilmedik bilmek isterdimki guclu stress ve yaxyd qorxudan ola biler?
Assalomu alekum mani ukam vaskulitni ohrgi bosqichida nima qilishni bilmi boldik iltmos vaskulitni davosini topkanlar bolsa yoki tuzalganlar bolsa manga aloqaga chiqilar hozir judayam yomon ahvoldaman 948702104