Contents
- What is a hemorrhagic stroke?
- Symptoms of a hemorrhagic stroke
- Causes of hemorrhagic stroke
- Coma in hemorrhagic stroke
- Passage of medical and social examination
- Treatment of hemorrhagic stroke
Timely detection of the first signs of the disease and rapid delivery of the patient to the clinic by about 15% increases the likelihood of a favorable outcome of hemorrhagic stroke.
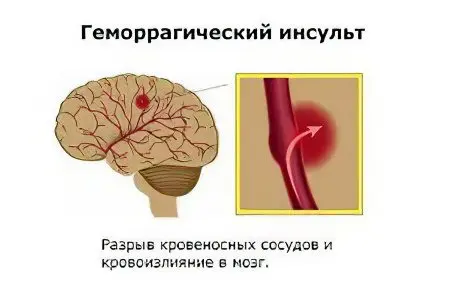
What is a hemorrhagic stroke?
The nosological form includes two terms: “hemorrhage” is a hemorrhage, and the word “stroke” means a heart attack (ischemic necrosis) of a part of the brain.
Hemorrhagic stroke is a hypertensive hemorrhage in the parenchyma of the brain, accompanied by an acute violation of cerebral circulation, loss of the functions of the affected area, the development of pathogenesis in the nucleus and the perifocal (around the nucleus) zone. The disease is manifested by general and local neurological symptoms.
A more severe pathogenesis in comparison with ischemic stroke is associated with a cumulative effect from:
Hemorrhages in the brain tissue, compression of the surrounding vessels;
Inflammatory-necrotic processes in the core of the stroke;
Dystrophic and inflammatory processes on the periphery of the nucleus.
There are two main types of cerebral hemorrhages of different origin:
Hemorrhagic stroke (HI) – hemorrhage / impregnation of the brain parenchyma;
Subarachnoid hemorrhages (SAH) are non-traumatic hemorrhages in the cerebral cortex, not associated with vascular malformations.
During the initial observation of a patient, hemorrhage is diagnosed as an intracerebral hematoma (ICH). Differentiation is carried out in the clinic based on the results of instrumental (MRI, CT) visualization of the structures of the brain and cranium.
There are several options for localization of hemorrhages in the brain, namely:
Putamenal lateral (lateral) – on the side of the internal capsule;
Subcortical (subcortical);
Lobar – in the first lobe of the brain;
Thalamic (medial) – located to the center of the internal capsule;
Mixed;
Cerebellar;
Stem (bridge).
Putamenal strokes are widespread – they account for up to half of all types of hemorrhagic strokes, subcortical and thalamic strokes are less common – about 15% for each type. Hemorrhages in the cerebellum and brain stem are detected much less frequently – up to 8% of all strokes.
The most severe lesions of the body are massive hemorrhages in the hemisphere, trunk or cerebellum of the brain. Hemorrhagic strokes are more likely to develop in men prone to hypertension and having bad habits. The likelihood of cerebral hemorrhage increases with age.
Symptoms of a hemorrhagic stroke
More than a hundred different clinical symptoms of hemorrhagic stroke are known, and the transformation of ischemic stroke into hemorrhagic is also possible. This greatly complicates the differential diagnosis of the disease. The primary signs indicating a stroke should be determined by describing the patient’s sensations, changes in speech, severe headache, impaired consciousness.
Possible precursors of hemorrhagic stroke

Tingling, numbness of half of the face;
Severe sharp pain in the eyes, partial loss of vision;
sudden loss of balance;
Difficulties in understanding speech.
They appear shortly before the attack, but are not mandatory signs of GI.
For hemorrhagic stroke, a sudden onset of the disease is more characteristic. On the eve or immediately before an attack, stress in the form of physical and / or emotional stress is possible.
During a telephone conversation with the operator, it is necessary to clearly describe the signs of a stroke found in the patient.
Signs of a hemorrhagic stroke in a conscious person:
Rapidly increasing headache;
Nausea, vomiting;
Cardiopalmus;
Intolerance to bright light, “circles” and “midges” before the eyes;
paresis, Paralysis of the arms, legs, facial muscles;
Difficult speech.
Signs of hemorrhagic stroke in an unconscious person:
There are four clearly defined stages of the regression of consciousness. They can be defined as follows:
Stunning – an incomprehensible look of the patient, a weak response to others;
Doubtfulness – resembles a dream with open eyes, the gaze is fixed in space;
Sopor – resembles a deep sleep, a weak reaction of the pupils, a light touch on the cornea of the patient’s eye is accompanied by a reaction, the swallowing reflex is preserved;
Coma – deep sleep, there are no reactions.
An epileptiform (similar to epilepsy) seizure is also one of the possible debuts of a hemorrhagic stroke. Typically, this symptom occurs in 10% of patients with a lobar stroke.
In case of impaired consciousness, it is necessary to prevent the retraction of the tongue, to prevent the overlap of the airways. Before the arrival of the ambulance, the victim should be laid in a horizontal position, his head slightly raised.
The probability of death in hemorrhagic stroke, depending on the patient’s condition:
Clear consciousness – up to 20%
Deafness – up to 30%;
Somnolence (slight clouding of consciousness) – up to 56%;
Sopor (subcome – deep depression of consciousness) – up to 85%
Coma – up to 90%.
Causes of hemorrhagic stroke
In about 2-15% of cases, the causes of hemorrhagic stroke remain unrecognized. In the history of 25% of patients there are references to acute disorders of cerebral circulation of unclear etiology.
The main proven causes of hemorrhagic stroke:
Arterial hypertension;
Smoking;
Diabetes;
Dyslipidemia;
Atrial fibrillation;
Diseases of the cardiovascular system;
Asymptomatic stenosis of the carotid arteries;
sickle cell anemia;
Obesity;
Sedentary lifestyle.
Causes of GI that a person can correct on their own
Simple regular stroke prevention, based on knowledge of the pathophysiology of the cardiovascular system, reduces the risk of strokes and premature death by 10-30% in people who take care of their health.
Arterial hypertension
Prolonged hypertension is accompanied by atherosclerosis, loss of elasticity, forced expansion of blood vessels, thinning of their walls. A sharp jump in blood pressure can provoke a rupture of the walls of cerebral vessels.
American classification:
The risk of atherosclerotic vascular damage begins to increase already when the blood pressure goes beyond 115/75. Therefore, normal blood pressure was specifically reduced by 1 unit so that you pay attention to this:
Normal blood pressure – 119/79 mm Hg.
Prehypertension – 120/80 to 139/89.
Hypertension 1 degree – 140/90 to 159/99.
Hypertension 2 degree – 160/100 to 179/109.
Hypertension 3 degrees – 180/110 and above.
European classification:
Optimal blood pressure – 119/79 mm Hg.
Normal blood pressure is 120/80-129/84.
“Highly normal” blood pressure is 130/85 over 139/89.
Hypertension – 140/90 and above.
Drug correction of blood pressure is an important factor in the prevention of stroke. Decrease in pressure by 5 mm Hg. reduces the risk of stroke by 14%, the risk of death by 7%.
Correction must be started at pressure:
above 140/90 if you do not have cardiovascular disease;
above 130/85 if you have diseases: ischemic heart disease, diabetes, kidney disease, cerebrovascular disease.
For self-monitoring of blood pressure, automatic and semi-automatic blood pressure monitors are recommended, with a shoulder or wrist cuff (Omron, Nissei, AND, others). The choice of drugs should be agreed with the cardiologist. Referrals to a cardiologist “according to the quota” can be obtained from a general practitioner at the local polyclinic. The examination can also be done for a fee at the cardiology center.
Dyslipidemia
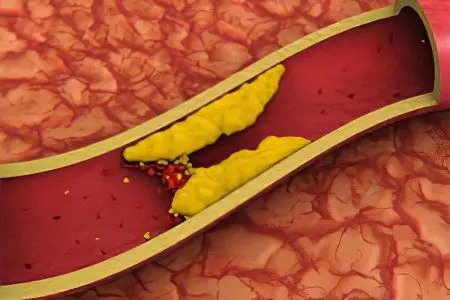
Violation of lipid metabolism with an excess of low-density cholesterol leads to a narrowing of the lumen of cerebral vessels, deterioration in the nutrition of the nervous tissue, a decrease in the function of brain activity and the development of atherosclerosis.
Atherosclerosis, including at the subclinical stage, is the cause of the onset of hemorrhagic stroke. Normal level:
total cholesterol – up to 5,0 mmol / l;
low density lipoproteins (LDL) – 2,6-3,3 mmol / l;
high density lipoproteins (HDL) – 1,03-1,52 mmol / l.
With an elevated level of LDL, the choice of drugs must be agreed with the therapist. Correction of cholesterol levels is carried out by pharmacological agents – statins, fibrates, niacin. Statins are very effective in ischemic strokes, less effective in cerebral hemorrhages.
Diabetes
Fasting plasma glucose levels:
less than 6.1 mmol / l – normal level;
from 6.1 to 7.0 mmol / l – a harbinger of carbohydrate metabolism disorders;
more than 7.0 mmol / l – diabetes mellitus (clinical confirmation required).
Whole blood glucose levels vary. Portable devices for self-monitoring of blood glucose levels are commercially available. The devices have a built-in high/low glucose notification function. In Russia, portable glucometers of the OneTouch series, Omelon and others are recommended for use. Therapeutic adjustment of carbohydrate metabolism will be agreed with the doctor, the choice of pharmaceuticals depends on the type of diabetes.
Pregnancy and postpartum

Subcortical hemorrhages are more common, less often – hemorrhages in the parenchyma. Hemorrhages are usually caused by massive birth blood loss and related disorders in the work of the cardiovascular system. Treatment is carried out taking into account the nature of the identified pathology.
Smoking
Smoking is one of the main causes of stroke. The stimulating effect of nicotine on the pathogenesis of atherosclerosis has been proven. Quitting smoking significantly reduces the risk of stroke. (See SCORE Cardiovascular Risk Chart)
Sedentary lifestyle
The call to play sports applies more to young people. For seniors and the elderly, it is enough to do moderate exercise as part of a group of people of the same age, or to walk regularly in the fresh air.
Acute period of hemorrhagic stroke
Upon admission of the patient to the clinic, neuroimaging of the brain and a clinical assessment of the patient’s condition are performed before urgent therapeutic measures are taken.
Symptoms of the acute period of GI that are important for determining the prognosis of the disease
The following symptoms are considered unfavorable (except for disorders of consciousness):
The volume of hematoma in the substance of the brain is more than 7 cm3;
The volume of intraventricular hemorrhage is more than 2 cm3;
Age group of the patient from 60 years and older;
Arterial hypertension;
Concomitant chronic pathology;
dislocation syndromes.
Dislocation syndromes are clinical manifestations of acute brain disorders that develop as a result of a pathological expansion of the brain volume when its normal location (location) in the skull changes.
Nine variants of displacement of the medulla in the cranium relative to the usual location are known, including two main ones that are of vital importance in strokes.
The displacement of the brain towards the anatomical formations is characterized by the following symptoms:
Temporo-tentorial, cerebellar-tentorial herniation – accompanied by nystagmus (rhythmic movements of the eyeballs), paresis of the gaze (the gaze is unable to follow the movement of the object), decreased response to light, muscle atony, arrhythmia on the ECG;
Cerebellar tonsils into the foramen magnum – accompanied by pathological types of arrhythmic breathing, the disappearance of the pharyngeal reflex, a decrease in muscle tone and blood pressure.
Other symptoms of poor prognosis of intracranial hemorrhage

The study should be carried out only by a trained doctor, since incompetent manipulations can aggravate the patient’s serious condition.
Symptoms are as follows:
Anisocoria – different pupil diameters;
Decreased pupillary response to light;
Positive oculocephalic reflex – in a person in a coma, with a violent turn of the head, the pupils are displaced in the opposite direction from the tilt;
Bulbar syndrome – impaired speech, sound pronunciation and swallowing, lethargy of the muscles of the tongue and lips;
Pseudobulbar syndrome – the same signs as with bulbar syndrome, but there is no lethargy of the muscles of the tongue and lips, but there is an unreasonable crying and laughter of the patient.
The patient’s condition is studied in the dynamics of pathogenesis. Hemorrhagic strokes are characterized by two peaks of exacerbation of the disease, which coincide with the maximum mortality of patients:
On the second or fourth day – the peak is associated with the onset of pathogenesis in the focus of hemorrhagic stroke;
On the tenth-twelfth day – the peak is due to the addition of complications of pathogenesis.
Coma in hemorrhagic stroke
Disorders of consciousness are characteristic of many pathologies, manifested by inhibition of the functions of the reticular formation of the brain.
Brain dysfunction develops under the influence of:
Endo- and exotoxins – derivatives of the end products of metabolism;
Oxygen and energy starvation of the brain;
Metabolic disorders in brain structures;
Expansion of the volume of the substance of the brain.
Acidosis, cerebral edema, increased intracranial pressure, impaired microcirculation of brain fluids and blood are of the greatest importance in the development of coma.
The state of coma affects the functioning of the respiratory system, excretion (kidneys) and digestion (liver, intestines).
Getting out of a coma at home is impossible, and very difficult even in intensive care.
The clinical definition of coma is carried out according to the GCS (Glasgow Coma Scale), some other methods that are important for clinicians are used. Allocate precoma and four stages of coma. The easiest is the first, and the hopeless state of the patient corresponds to the fourth stage of coma.
A patient who has had a stroke is defined as a person who has temporarily lost his ability to work (VUT). With an unfavorable labor prognosis after 3 months from the start of treatment, the question arises of sending a person to a medical and social examination (MSE) for examination for:
Disability (there are no prospects for the restoration of functions);
Continuation of treatment on sick leave (there is a possibility of positive dynamics and restoration of functions).
The ITU Bureau makes a decision based on the data of an objective examination of the patient, the results of instrumental and laboratory studies.
What should be considered before the examination for disability?

Which doctors do you need to see?
Clinical conclusions required by the ITU Bureau:
Cardiologist;
Endocrinologist;
Oculist;
Neurologist/therapist.
List of laboratory and instrumental studies required by the ITU Bureau:
General and biochemical parameters of blood;
ECG, rheoencephalography (REG), electroencephalogram (EEG);
Computed tomography (CT), magnetic resonance imaging (MRI);
X-ray in different projections of the cranium and cervical vertebrae, including with contrast;
Doppler ultrasound of the vessels of the neck and brain (USDG) / transcranial Dopplerography (TCDG);
Lumbar puncture (according to indications).
Specialists of the ITU bureau conduct an examination of the patient’s ability to work according to several indicators, including the following:
The severity of pyramidal disorders (the ability to move, the ability to overcome obstacles, the coordination of body position in space, the severity of paresis;
The severity of extrapyramidal disorders (problems with speech, slowness in performing habitual actions, chorea, athetosis, choreoathetosis, hemiballismus, myoclonus, facial hemispasm);
The state of the functions of the organs of vision (hemianopsia, narrowing of the visual field, amaurosis, amblyopia, visual agnosia, decreased detailed vision);
The state of brain functions (aphasia, motor deficit, difficulty in communication);
Attacks of epileptic seizures (focal / partial, generalized);
Violation of mental functions (asthenia, dementia, decreased intellectual status, cognitive defects).
Factors taken into account by the ITU commission before making a decision:
Unfavorable course of the disease, the possibility of recurrence of stroke;
Unclear labor prognosis, preservation of brain activity disorders, slow recovery of functions;
The inability to return to work, the decrease in intellectual and physical capabilities below the level required to continue working under the same conditions.
Groups of disability in hemorrhagic stroke:
Group III involves a return to work, while taking into account the need to create facilitated working conditions;
Group II assumes the presence of restrictions on the ability to move, orientation and the possibility of self-service;
Group I involves pronounced disorders, loss of the ability to self-service and the ability to move around, a decrease in intelligence.
Treatment of hemorrhagic stroke
There is a generally accepted algorithm for choosing a method of therapy for hemorrhagic stroke.
Surgery

Surgical tactics are indicated for:
Lobar and lateral hemorrhages of medium and large volume;
Deterioration of the patient’s condition in the dynamic study of CT / MRI;
Hematomas of the cerebellum and brain stem, causing neurological symptoms.
Surgical contraindications:
Deep coma with stem dysfunctions (100% lethality);
Medial hematomas of any size (mortality rate 90-100%).
Conservative therapy is indicated for:
The stable condition of the patient and the absence of neurological deficit;
Small supratentorial hematomas.
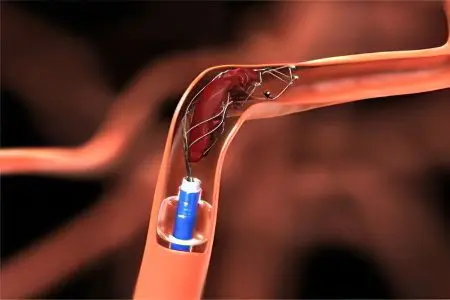
There are two main approaches to the operation, namely:
Classical microneurosurgical interventions;
Endoscopic techniques of microneurosurgery.
Visual verification of hematomas before surgery includes CT, MRI studies, angiography of cerebral vessels and other studies according to indications.
Surgical intervention is prescribed according to the results of neuroimaging:
The volume of HMG is more than 30 ml;
Dislocation of brain tanks;
Deterioration of clinical and neurological status.
Taking into account the qualification training of the surgical team, the best results are shown by the endoscopic technique (sparing, makes it possible to visualize the operation cavity). The classical method of microsurgical intervention is good for difficulties in controlling the homeostasis of the brain tissue.
Conservative therapy and prevention
Here we present drugs of different pharmacological groups used for the treatment of the acute period of hemorrhagic stroke. Regulation of blood pressure and angiospasm is necessary in the acute period of hemorrhagic stroke.
Antihypertensive drugs:
Selective beta-blockers (Atenolol, Metoprolol, Betaxolol, Bisoprolol, Nebivolol, Esmolol, Acebutolol);
Non-selective beta-blockers (Anaprilin, Nadolol, Sotalol, Timolol, Oxprenolol, Pindolol, Penbutolol);
Mixed beta-blockers (Carvedilol, Labetalol).
calcium antagonists:
First generation (Isoptin, Finoptin, Fenigidin, Adalat, Corinfar, Kordafen, Kordipin, Diazem, Diltiazem);
Second generation (Gallopamil, Anipamil, Falipamil, Isradipine/Lomir, Amlodipine/Norvasc, Felodipine/Plendil, Nitrendipine/Octidipine, Nimodipine/Nimotop, Nicardipine, Lacidipine/Lacipil, Riodipine/Foridon);
Third generation (Klentiazem).
Antispasmodics:
Direct action (Papaverine, No-shpa, Drotaverine, Nitroglycerin, Otilonium bromide, Mebeverine, Halidor, Gimekromon);
Indirect action (Aprofen, Ganglefen, Atropine, Difacil, Buscopan).
ACE inhibitors (angiotensin-converting enzyme):
Sulfhydryl group (Benazepril, Captopril, Zofenopril);
Carboxyl group (Cilazapril, Enalapril, Lisinopril, Perindopril, Quinapril, Ramipril, Spirapril, Trandolapril);
Phosphinyl group (Fosinopril).
The following auxiliary medicines are used to treat hemorrhagic stroke:
Sedatives (Diazepam, Elenium, Phenobarbital);
Hemostatic (Dicinone / Etamzilat, Rutin, Vikasol, Ascorbic acid);
Antiprotease (Gordoks, Kontrykal);
Multivitamins with micro and macro elements (Calcium pantothenate, calcium gluconate);
Antifibrinolytic (Gamma-aminocaproic acid, Reopoliglyukin);
Nootropic (Cortexin);
Laxatives (Regulax, Glaxena).
Preparations for the regulation of intracranial pressure and cerebral edema:
Diuretics (Mannitol, Lasix);
Corticosteroids (Dexamethasone);
Plasma substitutes (Reogluman).
Thus, hemorrhagic stroke is a severe form of acute disorders of cerebral circulation, which is characterized by a high level of mortality and disability. The recovery period can last up to two years. Rehabilitation is aimed at teaching the patient how to overcome the neurological deficit. Disability is accompanied by a significant decrease in the quality of life of the patient and his environment.









