Contents
Hemolysis is the process of completing the four-month life cycle of erythrocytes that are destroyed naturally or by exposure to poisons, infectious agents, antibodies, and drugs on their membranes.
Where does hemolysis take place?
Types of hemolysis depending on localization:
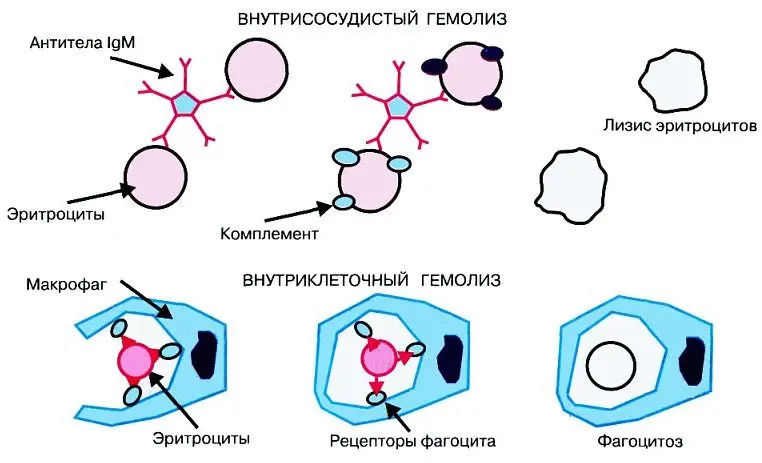
intravascular hemolysis. Occurs in the circulating blood, where the erythrocytes are affected by the environment.
intracellular hemolysis. Occurs in the liver, spleen, bone marrow – organs involved in hematopoiesis or in the accumulation of blood cells.
In some cases, hemolysis can occur outside the human body when the blood clot dissolves and stains the plasma in a laboratory setting.
Causes of hemolysis in blood tests:
non-compliance with the biomaterial sampling technique, the rules for its storage;
intentionally provoking the process of erythrocyte lysis, necessary to obtain a population of other blood elements.
For hemolysis, the properties of blood plasma and serum, their differences, are very important. Plasma fibrinogen (hereinafter referred to as fibrin) is the basis of a blood clot that sinks to the bottom of the test tube, turning plasma into serum. In the circulatory system, blood does not normally clot. This happens in exceptional cases – with disseminated intravascular coagulation, when a person’s life is at risk. But even there, serum is not formed, it is formed only outside the human body from fibrin filaments, which are converted into a blood clot.
A blood biochemistry test taken with an anticoagulant, or taken in a dry tube without the use of anticoagulants, will have incorrect results due to hemolysis of red blood cells.
The natural process of hemolysis is the norm
During natural hemolysis in a healthy body, the physiological death of old red blood cells occurs. This process takes place in the red bone marrow, in the liver and spleen.
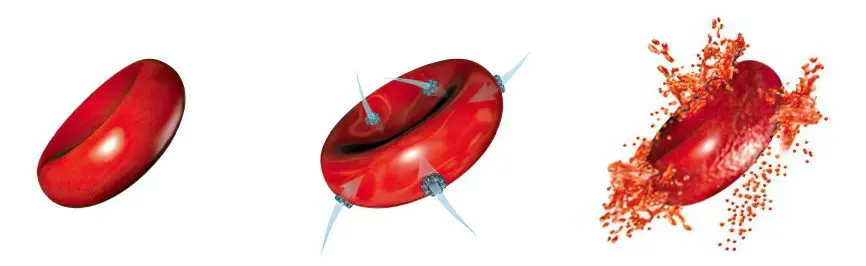
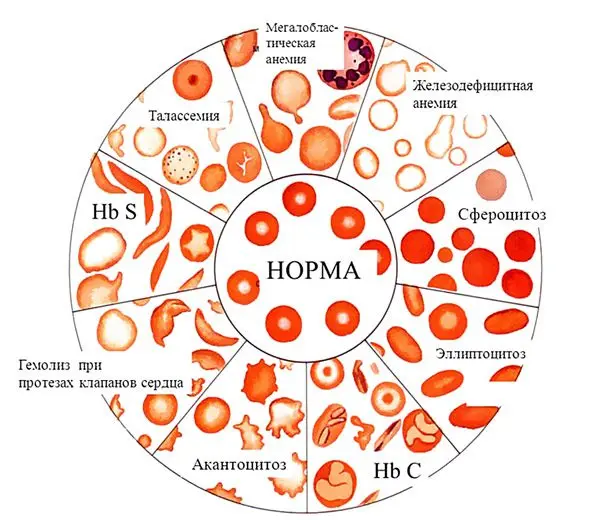
In pathological hemolysis, red blood cells die prematurely due to stretching and rupture of the cell membrane. Discocytes are affected by adverse factors, due to which hemoglobin from the membrane is released into the blood plasma.
Manifestation of hemolysis
Chronic hemolysis that accompanies diseases such as leukemia, sickle cell anemia, proceeds without severe symptoms, like many other physiological processes.
Causes of Acute Hemolysis Requiring Emergency Care:
Transfusion of blood incompatible by group and Rh factor;
Autoimmune hemolytic anemia, or anemia caused by poisoning;
Hemolytic disease of the newborn, where each breath of the newborn worsens the situation.
If the patient is conscious, he experiences the following symptoms:
feeling of heat;
Strong compression of the chest;
Pain in the lower back, possibly in the chest and abdomen.
Other symptoms:
A sharp decrease in blood pressure;
Hyperemia of the skin of the face, turning into cyanosis;
Spontaneous urination and defecation;
According to laboratory studies, intravascular hemolysis occurs in the circulatory system.
With radiation and hormonal therapy, during anesthesia, the signs can be erased. After a few hours, the acute symptoms subside, leaving lower back pain.
After a short time, a relapse occurs with the following manifestations:
Hyperthermia;
Jaundice of the skin and sclera of the eyes;
Severe headache;
Kidney dysfunction: protein and hemoglobin in the urine, cessation of urination, then anuria, uremia, death.
Coagulogram indicators:
Anemia caused by the release of hemoglobin into the plasma after the destruction of red blood cells;
Thrombocytopenia;
High levels of bilirubin;
Violation of blood coagulation processes.
Urine becomes red or black, it contains protein, potassium, hemoglobin.
Treatment of hemolysis

Appointments:
Exchange transfusion (for hemolytic disease of the newborn);
The introduction of blood-substituting solutions;
Plasmaphoresis;
The introduction of hormones;
Hemodialysis.
The effectiveness of the measures is monitored by constant laboratory tests.
Pathological hemolysis: causes and types

Types of hemolysis and the causes that caused it:
Immune. Caused by autoimmune diseases, hemolytic anemia, incompatibility with blood transfusion.
Mechanical. It occurs when tissues are crushed, extensive injuries, careless handling of blood samples.
Thermal. It is caused by freezing and heating solutions.
Chemical. Occurs upon contact with aggressive media that have penetrated through the respiratory or digestive system, as a result of injections. In the laboratory, samples can be damaged by contact with acid or alkali.
Электрический. Occurs with electric shock, in the laboratory – when blood is placed in an electric field.
Biological. It develops due to exposure to poisons of animal or plant origin: snake bite, contact with pale grebe and other poisonous mushrooms, penetration into the body of malarial plasmodium.
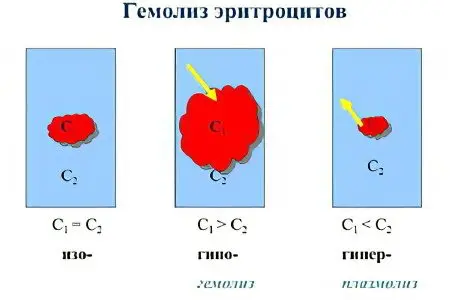
Osmotic. It occurs due to the effect on red blood cells of a hypotonic solution (0,48%, 0,32%) of sodium chloride, used to increase the volume of circulating blood and destroy red blood cells.
Analysis of osmotic resistance of erythrocytes
This blood test is aimed at determining the resistance of red blood cells when placed in a hypotonic solution.
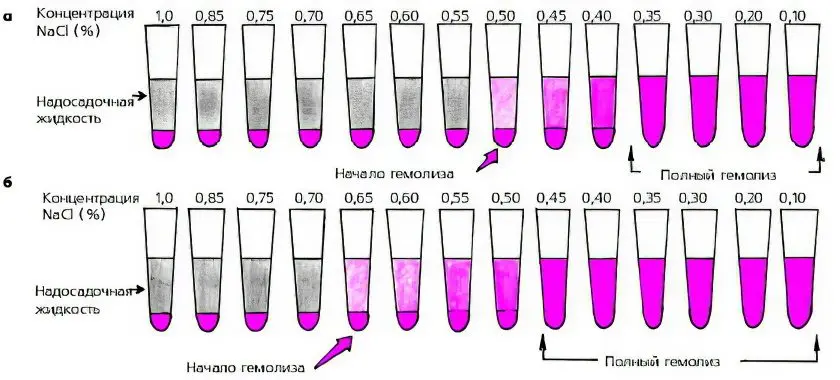
Study parameters:
Minimal SSE – erythrocytes are destroyed in 0,45-0,48% solution of NaCl;
Maximal OSE – the destruction of erythrocytes occurs in 0,32-0,34% solution of NaCl.
Indicators of osmotic resistance depend on the shape of the cells and their degree of maturity. Normally, the ratio of thickness to diameter (sphericity index) is 0,27-0,28.
Mature erythrocytes, which are on the verge of their existence, have a spherical shape, low membrane strength. With hemolytic anemia, a large number of spheroid forms indicates the imminent death of erythrocytes, reducing their life by 10 times, up to 12-14 days.
The spherical shape of red blood cells in anemia indicates an increase in the sphericity index – a symptom of premature death of red blood cells.
The most resistant to hypotension are reticulocytes that have recently emerged from the bone marrow. They have a flattened disk shape, a low level of sphericity. The analysis of osmotic resistance can serve as an indicator of the activity of the red blood brain.
Drug therapy and hemolysis
Some drugs accelerate the destruction of red blood cells, hemolysis is their side effect. When the drug is discontinued, this process stops.
Drugs that cause hemolysis:
Analgesics and antipyretics (Aspirin, Amidopyrine);
Diuretic (Diakarb) and drugs of the nitrofuran series (Furadonin);
Sulfonamides (Sulfalen, Sulfapyridazine);
Drugs to lower blood sugar (Tolbutamide, Chlorpropamide);
Anti-tuberculosis drugs (isoniazid, PAS);
Drugs for the treatment of malaria (Quinine, Akrikhin).
Problems caused by the use of drugs should be reported to the attending physician.
Video: experience – hemolysis of red blood cells under the influence of alcohol:









