Contents
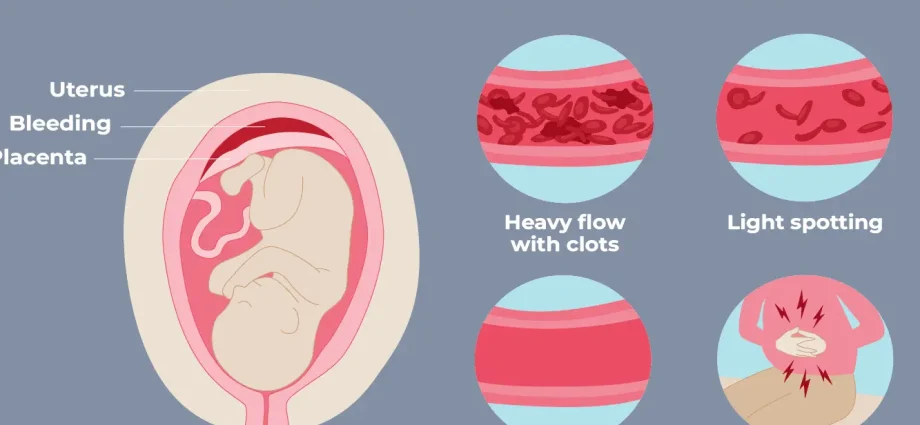
Bloody discharge during early pregnancy is an alarming symptom that causes panic, especially in young women who wanted and planned to become mothers. When contacting a doctor, the gynecologist will conduct an examination, as a result of which he can make a diagnosis – a hematoma during pregnancy.
Pregnancy hematoma or retrochorial hematoma is usually diagnosed in the first trimester of pregnancy, and this often indicates a threatened miscarriage. But with timely measures taken, it is quite possible to prolong pregnancy.
In clinical practice, subchorial (retrochorial and marginal) and subamniotic hematomas are distinguished. The latter are rare and less dangerous, which cannot be said about retrochorial ones.
So what are retrochorial hematomas and why are they dangerous?
What is a hematoma
This is a limited accumulation of blood that occurs when organs and tissues are damaged with the formation of a cavity. The accumulation of blood occurs due to rupture or injury of blood vessels, and liquid or already clotted blood accumulates in this cavity.
With partial exfoliation of the fetal egg between the wall of the uterus and the chorion (embryo shell), a space is formed in which blood can accumulate – this is a retrochorial hematoma. It is known that it is she who causes 18% of cases of all first trimester bleeding.
Causes of hematoma during early pregnancy
In general, we can name a whole list of reasons that can lead to the formation of a hematoma in early pregnancy. The main ones include:
- physical impact on the stomach: accidental falls, bruises or vibration, as a professional factor;
- stress and strong emotional experiences;
- excessive physical exertion;
- diseases of the reproductive system, for example, fibroids, endometritis, etc.;
- disorders of the coagulation and anticoagulation systems of the blood;
- timely not detected and poorly treated sexually transmitted diseases.
There are also predisposing factors that increase the likelihood of hematoma formation in early pregnancy:
- insufficiency of the luteal phase of the menstrual cycle;
- pregnancy stimulation: ovulation stimulation or IVF;
- history of abortion;
- lack of preparation for pregnancy, that is, a set of diagnostic, preventive and therapeutic measures that will help prepare the body for the full conception, bearing and birth of a baby.
Symptoms of a hematoma during pregnancy
The reason to suspect a hematoma during pregnancy will be the appearance of spotting on underwear in the early stages of gestation. But often there is an accidental diagnosis on ultrasound, while there are no symptoms, which can be explained by the location of the hematoma.
For example, with its high location, that is, in the region of the fundus of the uterus, there may be no symptoms, and the resulting aching pains in the lower abdomen remain unnoticed, underestimated. But with its low location, the hematoma often empties and bloody discharge appears on the linen. By their number and volume, one can judge the development of a hematoma: a large amount of discharge indicates damage to the vessel of the uterine wall, while the discharge is liquid and scarlet in color.
Oddly enough, the appearance of dark, brown discharge is a good diagnostic sign. This suggests that the hematoma has emptied and will soon disappear.
Treatment of hematoma during early pregnancy
If a hematoma is diagnosed during pregnancy, treatment involves adherence to bed rest and rest. Sometimes it is difficult to implement this recommendation, so doctors often insist on hospitalization. Indeed, within the walls of the hospital there is an opportunity to provide emergency assistance.
To normalize bowel function and prevent congestion, it is recommended to follow the rules of nutrition: exclude foods that increase peristalsis. The intestines, swollen from gases, put pressure on the uterus, which helps to increase its tone. And this increases the likelihood of complications – an increase in the size of the hematoma and, as a result, abortion.
Drug therapy consists in prescribing drugs that normalize blood clotting, and the hematoma does not increase. Antispasmodics will help relieve uterine hypertonicity, and vitamins will help normalize hormonal regulation.
The duration of treatment is from 2 to 4 weeks and the hematoma resolves after a few days.
Diagnostics
The diagnosis is made on the basis of complaints and ultrasound data. Using this research method, the doctor can identify signs of uterine hypertonicity. The thickened area of the uterus presses on the fetal egg, as a result, it changes shape, becomes elongated. With the help of ultrasound, it is possible to see directly the formation itself – a hematoma, to assess its location, size, behavior and growth. Based on these data, a treatment plan is drawn up.
Modern treatments
Until recently, it was believed that the timely detection of a hematoma during pregnancy and the relief of the process does not pose any danger in the future. However, its appearance is a predictor of complications in the future. Therefore, examination and preventive treatment is carried out at critical periods of pregnancy: 12, 24, 32 and 36 weeks of gestation.
Prevention of hematoma during early pregnancy at home
Given the variety of causes, it is sometimes very difficult to predict the appearance of a hematoma during pregnancy, therefore, it is difficult to talk about any specific prevention. However, as the results of studies show, an integrated approach to the prevention of placentation pathologies reduces the likelihood of its development from 25% to 10%. Preparation for pregnancy as a concept, with the whole list of necessary measures, prevention of physical and emotional stress, timely treatment of infections, improved perinatal results: there were no perinatal losses, the risk of perinatal morbidity decreased by 40%.
Popular questions and answers
We talked about the consequences of a hematoma during pregnancy and alarming symptoms with pediatrician, pathophysiologist and immunologist, WHO/UNICEF expert Alena Paretskaya.
Is it possible to treat a hematoma during pregnancy with folk remedies?
Every woman should strictly follow the recommendations of the doctor leading the pregnancy. And if bed rest is prescribed, it must be observed, household chores can wait. Otherwise, the consequences will not be long in coming.
What are the complications of hematoma during pregnancy?
The risk of serious complications increases with the formation of bleeding at the end of the first trimester. It is known from statistical data that in this case 5-10% of pregnancies end in miscarriage. If the hematoma is 40% or more of the size of the fetal egg, this is an unfavorable diagnostic sign.










Բարև ձեզ ես ունեմ հեմատոմա բժշկուհին ինձ նշանակելա դյուֆաստոն և ֆոլեպերին։Դուք ինչ խորհուրդ կտաք,ինչ անել՞