Contents
Hematemesis
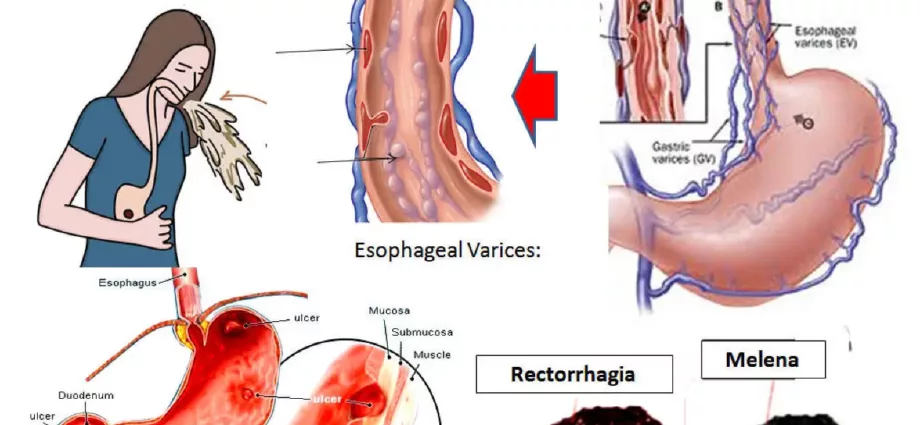
Hematemesis is defined as the rejection of blood, red or black, through the mouth during an effort to vomit. It is often accompanied, a few hours later, by melena, which is an evacuation, through the anus, of black blood characterized by a nauseating odor of “tar”.
Caused by ulcers in nearly 50% of cases, hematemesis is observed by the patient himself, who then goes to his doctor or the gastroenterologist, or even directly to the emergency room in the event of significant bleeding. Several treatments are possible, depending in particular on the pathology that caused this vomiting of blood.
Hematemesis, how to recognize it
What is hematemesis?
Hematemesis, the rejection of red (or black) blood through the mouth during vomiting, is linked to bleeding from the digestive tract. Reason for which, very often, a few hours after this vomiting of red blood, an evacuation of black blood via the anus occurs, by rejection of the blood which has been digested: thus, lower down, in the rectum, the blood linked to the hemorrhage which was first evacuated upwards, by the mouth, is then evacuated downwards, after its digestion. This black blood evacuated by the anus constitutes the melena, characterized by its color but also by its very nauseating odor, of “tar”.
How to recognize hematemesis?
The patient will, on his own, recognize hematemesis when he vomits blood through the mouth. He will then go directly to his general practitioner or a gastroenterologist, if the bleeding is not too severe, or immediately to an emergency department if the bleeding is severe.
Risk factors
“The risk factors for hematemesis are, mainly, stomach or duodenal ulcers, gastric ulcerations, cirrhosis of the liver, esophageal ulcers or even acute gastritis”, reports Doctor William Berrebi, gastroenterologist at the Geoffroy-Saint-Hilaire clinic in Paris.
The causes of hematemesis
Gastric ulcers and ulcers
Hematemesis can be caused by an ulcer, caused by the presence of the bacteria Helicobacter pillory. In addition, gastric ulceration can also be caused by taking anti-inflammatory drugs, NSAIDs (ie, non-steroidal anti-inflammatory drugs). This peptic ulceration can cause this type of vomiting of blood, it is also the major cause of hematemesis, since it represents 40 to 50% of them.
Liver cirrhosis
Cirrhosis of the liver is the second main cause that can cause hematemesis, which will then be linked to ruptured varicose veins in the esophagus or stomach.
Esophageal ulcer
Another cause of vomiting blood is erosions or ulcers of the esophagus. Thus, peptic esophagitis, the inflammation of the lower esophagus (tube connecting the pharynx to the stomach), due to gastroesophageal acid reflux, can also be the cause of hematemesis.
Acute gastritis and duodenitis
The fourth possible cause leading to hematemesis is acute gastritis, affecting the stomach, or acute duodenitis, affecting the duodenum, another part of the digestive system, particularly in cases of acute stress (stay in an intensive care unit by example).
These are the four major causes that can be at the origin of hematemesis. Other etiologies can still cause it, such as, in particular, stomach cancer, or Mallory Weiss syndrome.
Risks of complications from hematemesis
“The risk of major complication, in the event of profuse hematemesis, is hemorrhagic shock secondary to deglobulization (that is to say a decrease in red blood cells in the blood). The other complications are linked to the causal pathology, stomach cancer for example ”, details Doctor William Berrebi.
Hemorrhagic shock results from a decrease in circulating blood mass, which can lead to cardiac arrest.
Acute circulatory insufficiency causes manifestations mainly linked to the deficit of oxygen supply in tissues and organs caused by blood loss (coronary insufficiency, acute hepatic insufficiency in particular: “shock liver”).
In the case of stomach cancer, the associated complications are the extension of the tumor to other organs, metastasis.
But apart from cancerous causes, the major complication of hematemesis is really this risk of hemorrhagic shock linked to the loss of a large quantity of blood in a very short time. In rare cases, this symptom can lead to death. However, increasingly optimized care often makes it possible to curb hematemesis and its complications.
Treatment and prevention of hematemesis
Treatment for hematemesis depends on its cause.
The general measures are:
Transfusion of red blood cells and filling the patient
The patient should be rehydrated and his deglobulization should be corrected. The transfusion of red blood cell concentrates will thus make it possible to recover stable hemodynamics (ie correct volumes and flow rates of the blood flowing through the vessels).
The objective, for maintaining the patient’s hemodynamic state, is to maintain a blood pressure greater than or equal to 80 millimeters of mercury, to preserve a hemoglobin level greater than 8 grams / dl of blood, to maintain a level hematocrit greater than 25% (i.e. the percentage of red blood cells in relation to the total blood volume).
“A patient suffering from a severe hemorrhage resulting in hematemesis will first be treated in an intensive care unit, then in a continuing care unit. Rehydration and transfusion will restore her to a stable hemodynamic state. One of the most important criteria for assessing the extent and whether or not the bleeding is active is the volume of RBC transfused during the first 24 hours to maintain a correct hemodynamic state (greater or less than six RBCs) », Insists Doctor Berrebi, who is also the author of a reference medical book entitled Diagnostics and Therapeutics (8th edition).
Prevention of hematemesis
To prevent hematemesis linked to an ulcer of the stomach or duodenum, it is necessary to systematically treat for the bacteria Helicobacter pillory, with antibiotics and proton pump inhibitors.
These proton pump inhibitors are also used to prevent hematemesis associated with taking NSAIDs (nonsteroidal anti-inflammatory drugs).
In the event of cirrhosis of the liver, prevention consists of “To prevent esophageal or gastric varices, a consequence of portal hypertension, from bleeding”, underlines Doctor Berrebi. This treatment is based on beta blockers, which will decrease the heart rate and to a lesser extent on the rubber band ligation of varicose veins.
Curative treatments for bleeding ulcers
Specific treatments depend on the causes of hematemesis.
Regarding hemorrhagic ulcers, the objective is to achieve endoscopic hemostasis, either by injecting a sclerosing product on the ulcer and its periphery during a digestive endoscopy, or by placing clips, that is to say kinds of staples, applied to the ulcer, in order to close the wound and thus stop the bleeding.
Endoscopic hemostasis is routinely associated with an intravenous proton pump inhibitor, such as omeprazole or esomeprazole. When the patient’s condition improves, they can then be delivered orally.
If the hematemesis persists despite everything, it is then possible to operate, in the event of massive bleeding. This hemostasis surgery is rare. “The treatment consists of suturing the area and can even go as far as resection of the hemorrhagic area”, specifies Doctor William Berrebi, who insists: “It is really a treatment of last resort, once all the other treatments have already been tried”. Indeed, in general, the sclerosis or the clips are sufficient to stop the bleeding.
Curative treatment of ruptures of varicose veins
- Regarding the ruptures of varicose veins associated with cirrhosis of the liver, an endoscopic procedure will consist of ligating the varicose veins (using rubber bands) or injecting glue.
- A vasoconstrictor treatment allows the intravenous injection of a vasoconstrictor for varicose veins, such as, for example, terlipressin.
- Dabbing probes, a kind of inflated balloon used to crush varicose veins, are also used to stop bleeding.
- Finally, the “Transjugular intrahepatic portosystemic shunt”, known as TIPS, are a prosthesis method, placed between the hepatic vein and the portal vein. This prosthesis is placed by the trans-jugular route, that is to say via a vein in the neck.