Contents
- Helicobacter pylori eradication therapy scheme
- First line eradication of Helicobacter pylori
- Second line eradication of Helicobacter pylori
- Third line eradication of Helicobacter pylori
- The choice of drugs if it is necessary to conduct a repeated course of eradication therapy
- Protocol for the treatment of Helicobacter pylori in adults

Half a century ago, there were several theories that offer their own version of the causes of stomach and intestinal ulcers. The turning point was 1979, when, as a result of scientific research, it was proved that the primary source of this problem is the Helicobacter pylori bacterium, which normally exists safely in the gastrointestinal tract for more than half of all representatives of mankind. Any decrease in immune defense is a good reason for the reproduction of Helicobacter pylori colonies. For the treatment of heliobacteriosis, schemes have been created for the eradication of pathogenic bacteria from the human body.
Helicobacter pylori eradication therapy scheme
When choosing an eradication therapy regimen in each case, the doctor must take into account the following factors:
Therapy regimen;
Projected duration of treatment;
The clinical picture of this case of heliobacteriosis;
The cost of drugs included in the treatment regimen.
The Russian Gastroenterological Association and the Russian Group for the Study of Helicobacter pylori recommend taking as a basis a combined three-component therapy regimen that satisfies the following principles:
The ability to eradicate bacteria in at least 80% of cases;
Absence of side effects forcing the attending physician to cancel the treatment regimen, or provoking the patient to stop taking the drugs (up to 5% of such cases are allowed);
effectiveness even with a short course no longer than 1-2 weeks.
The methodology for prescribing eradication therapy is based on recommendations developed by the global community of gastroenterologists in Maastricht in 1996 and updated in 2000.
Recommendations of the Second Maastricht Agreement on anti-Helicobacter therapy:
In uncomplicated cases of peptic ulcer after a course of eradication therapy, the use of antisecretory drugs is not required.
Indications for eradication therapy other than peptic ulcer: MALT-lymphoma, atrophic gastritis, close family ties with a patient with gastric cancer, condition after resection for gastric cancer, the patient’s desire.
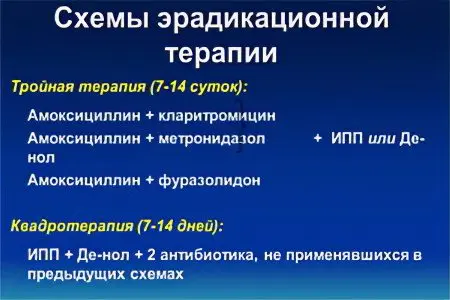
Treatment of Helicobacter pylori infection should take into account the possibility of failure of the first line of eradication therapy and the need to use the second line if the bacterium persists in the body. It is proposed to include 2 antibiotics in the first-line eradication scheme (triple therapy): Clarithromycin + Amoxicillin (or Metronidazole) and a proton pump inhibitor (or Ranitidine). It lasts no more than 7 days. If unsuccessful, it is recommended to use a second-line regimen (quadrotherapy), which includes 2 antibiotics: Tetracycline + Metronidazole, bismuth preparations and a proton pump inhibitor. The duration of quadrotherapy use is 7 days.
Currently, specific antibacterial drugs, probiotics and vaccines directed exclusively against Helicobacter pylori are not used in practice, they are still under development.
The developers of the Maastricht recommendations excluded from the treatment regimen the usual combination for Russia: Amoxicillin + Metronidazole + proton pump blocker due to increased resistance of Helicobacter pylori to nitroimidazole derivatives. Studies by Russian scientists have confirmed the low efficiency of this combination (only 30%). Russian gastroenterologists in first-line eradication therapy often use affordable and effective triple therapy, which includes bismuth + Amoxicillin + Furazolidone. Improvement of anti-Helicobacter therapy continues. In 2005, modern eradication therapy schemes of the first, second, third line were developed in the Netherlands.
First line eradication of Helicobacter pylori
The three-component first-line regimen gets its name from the fact that it consists of three drugs:
antibiotic clarithromycin,
antibiotic Amoxicillin,
proton pump inhibitor based on omeprazole, which regulates the activity of the acidic environment of gastric juice.
Proton pump inhibitors allow you to get rid of many negative manifestations of ulcers and gastritis caused by increased acidity of the stomach environment, as well as to avoid overly strict restrictions introduced into the diet of a patient with peptic ulcer. Nevertheless, restrictions still remain, although not as strict.
It is allowed to replace Amoxicillin with the antibiotic Nifuratel or Metronidazole. According to indications, a gastroenterologist can prescribe a drug based on bismuth derivatives in scheme 4. Normally, such drugs are included in the second-line eradication regimen, but their properties have a positive effect on the course of the process of stopping the inflammatory process. A protective coating is formed on the surface of the stomach, which relieves the symptoms of inflammation and pain.
Lightweight scheme for elderly patients:
Antibiotic Amoxicillin;
proton pump inhibitor;
Bismuth preparation.
To increase the effectiveness of standard first-line therapy, it is proposed to double the duration of its use – from 7 to 14 days. Expected efficiency – up to 95%. If the treatment is ineffective, the doctor recommends switching to the second line of eradication therapy.
Second line eradication of Helicobacter pylori
The four components of a second-line eradication scheme are:
2 antibiotics: Tetracycline + Metronidazole, or Amoxicillin + a drug from the nitrofuran group;
proton pump inhibitor;
Bismuth preparation.
Bismuth-based preparations are excellent cytoprotectors that restore the structure of the cells of the gastric and intestinal mucosa and their resistance to the aggressive effects of acid and waste products of Helicobacter pylori. In addition, they have a bactericidal effect, to a minimum reduce the risk of recurrence of heliobacteriosis. When planning a second-line eradication regimen, it is not recommended to use previously used antibiotics. An effective, affordable and cheap quadruple therapy regimen with bismuth is also not without drawbacks:
A large number of tablets taken (18 pieces per day);
Frequent side effects;
4-fold dosing regimen.
To enhance the effectiveness of therapy with bismuth preparations, fruits, juices, and milk are excluded from the diet for the duration of treatment. The duration of second-line therapy is 10-14 days.
Third line eradication of Helicobacter pylori

It is extremely rare to have to switch to the third line of eradication therapy, but this possibility still exists. Before starting the implementation of the third scheme, the patient is tested for the sensitivity of the Helicobacter pylori strain to antibiotics.
3rd line drugs:
Two antibiotics that have not been used before and have shown the highest degree of effectiveness in laboratory diagnostics;
The preparation is bismuth;
proton pump inhibitors.
Medicines based on bismuth (tripotassium bismuth dicitrate) have a complex effect:
Relieve manifestations of dyspepsia (bloating, heartburn, gastralgia); act against Helicobacter pylori as an effective bactericidal agent;
Stimulate the regeneration of damage to the deeper layers of the walls of the stomach.
Third-line therapy according to the Maastricht recommendations of the third convocation includes drugs from the group of rifamycins (Rifabutin) and quinolones (Levofloxacin). This combination was effective in 91% of cases. The resistance of Helicobacter pylori to Rifabutin is very low, therefore, its inclusion in the treatment protocol together with Amoxicillin and a proton pump inhibitor makes it possible to increase the effectiveness of therapy and even ignore the resistance of the bacterium to Metronidazole and Clarithromycin.
The choice of drugs if it is necessary to conduct a repeated course of eradication therapy

And the first, and second, and even the third regimen of Helicobacter pylori therapy may be ineffective when the percentage of eradication is 80% or less of the cases of the target achievement of the treatment goal. The effectiveness of treatment is reduced due to bacterial resistance to antibiotics, so the researchers of the problem do not stop searching for better regimens.
There is no concern about the resistance of Helicobacter pylori to Amoxicillin (less than 1%), to Tetracycline (close to 0).
The number of resistant strains of bacteria to other antibacterial drugs:
To Clarithromycin – in Europe from 9,9 to 18%, in Moscow – 19,3% in adults, 28,5% in children;
To Metronidazole – in Europe from 20 to 40%, in Moscow – 54,8% in adults, 23,8% in children
This is due to the frequent prescription of macrolide antibiotics in pediatric and therapeutic practice. Of no small importance in the success of eradication therapy are proton pump inhibitors, which create a favorable environment in the gastrointestinal tract for the use of antibiotics. With a low quality of drugs in this group, the effectiveness of antibacterial agents also decreases.
Studies are underway to add a probiotic to standard therapy to reduce stool frequency and flatulence.
A new scheme for the eradication of bacteria has appeared – sequential therapy, which takes 10 days. It is used when the first line scheme fails.
In the first 5 days take:
Proton pump inhibitor – 2 times a day;
Amoxicillin – 2000 mg / day.
In the next 5 days:
Proton pump inhibitor – 2 times a day;
Clarithromycin – 1000 mg / day;
Tinidazole – 1000 mg / day.
According to the study, even in patients infected with Helicobacter pylori with high resistance to Clarithromycin, eradication increased from 29% to 89%. In the remaining patients with unsuccessful first-line eradication, the rate increased from 78% to 91%.
Protocol for the treatment of Helicobacter pylori in adults
The main protocols for eradication of Helicobacter pylori in adults recommended by the Toronto and Maastricht Consensus 2016:
number | Protocol name | Protocol Components | Duration | Показания |
1 | Triple therapy |
| 14 | 1 eradication line |
2 | Bismuth Standard Quad Therapy |
| 10-14 | 2nd line of eradication in regions with low Hp resistance to Clarithromycin |
3 | Bismuth Optimizing Quad Therapy |
| 14 | The same |
4 | Concomitant quadruple therapy without bismuth |
| 10 | 1 line of eradication or 2-3 lines with the ineffectiveness of the previous ones |
5 | Optimized concomitant therapy |
| 14 | The same |
6 | Optimized Sequential Therapy with Levofloxacin | Stage 1 – 5 days:
Stage 2 – 5 days:
| 5 + 5 | 2nd or 3rd line of eradication |
7 | hybrid therapy | Stage 1 – 7 days:
Stage 2 – 7 days:
| 7 + 7 | 2nd or 3rd line of eradication |
8 | Triple therapy with levofloxacin |
| 10-14 | 2nd or 3rd line of eradication |
9 | Levofloxacin quadrotherapy |
| 14 | 2-3 eradication line |
10 | Bismuth quadruple therapy |
| 14 | 1, 2, 3 eradication line |
11 | Triple therapy with Ribafutin |
| 10 | final version with unsuccessful attempts 1,2, 3 lines of eradication |
To increase the effectiveness of treatment, it is recommended to use optimized eradication options – sequential and hybrid therapy. They include higher doses of PPIs (proton pump inhibitors), have a longer course of treatment, and have more powerful potential.
For treatment to be successful, it is important to educate the patient about the benefits of the treatment regimens being used and the possible side effects.









