Contents
What is acute gangrenous appendicitis?
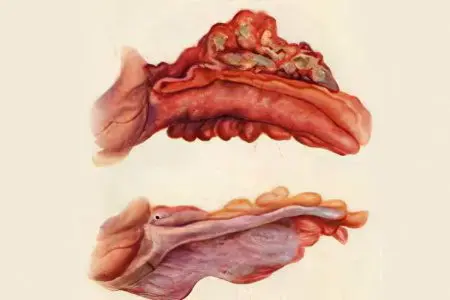
Acute gangrenous appendicitis – this is a kind of purulent inflammation of the appendix, which is based on irreversible destruction (destruction) of its wall. Therefore, it is referred to as one of the types of destructive appendicitis.
Such a diagnosis can be established only after an intraoperative visual assessment of the appendix: against the background of sharply edematous, loose, covered with fibrin and purulent layers, the walls are determined by areas of dark necrosis.
Any manipulations with the gangrenous-altered appendix end with its rupture.
Causes of gangrenous appendicitis
The etiopathogenesis of gangrenous appendicitis is determined by the mechanism of inflammation in the appendix. Risk factors for the development of the primary gangrenous process are:
Senile age and age-related changes in blood vessels;
Children’s age and congenital hypoplasia of the appendicular arteries;
Atherosclerotic lesions of the walls of the arteries of the intestine;
Formation of blood clots in the arteries and veins of the appendix;
These data suggest that the immediate causes of acute gangrenous appendicitis are microcirculatory disorders. Their result is a violation of blood circulation in the process and, as a result, its necrosis (gangrene). All other elements of pathogenesis: infection, violation of the outflow of appendicular contents, autoaggression of immune cells join secondarily, aggravating the course of the process.
It also happens that the cause of gangrenous appendicitis is the transition of simple forms of appendicitis (catarrhal and phlegmonous) to destructive with inadequate and untimely surgical treatment. In this case, the appendix is simply subjected to purulent fusion.
Consequences of gangrenous appendicitis

If gangrenous appendicitis is operated on before spontaneous rupture of the appendix, then this does not threaten the patient. The only thing that is noted a little more often than with other forms of appendicitis is suppuration of the postoperative wound.
But in case of refusal of the operation, in all cases, serious consequences develop:
Perforation of the appendix with leakage of purulent contents and feces into the abdominal cavity;
Self-amputation of the appendix (its complete detachment from the caecum);
Purulent and purulent-fecal peritonitis;
Abdominal sepsis;
Multiple abscesses of the abdominal cavity and pelvis;
Sepsis and pylephlebitis (spread of purulent infection into the systemic circulation).
All these conditions are characterized by a progressive and fulminant course, causing extremely severe intoxication with multiple organ failure. Such pathological changes end in irreversible disruption of the functioning of vital systems and the death of the patient.
Gangrenous-perforated appendicitis
If, against the background of gangrenous changes in the inflamed appendix, there is a violation of the anatomical integrity of one of its walls, they speak of gangrenous-perforated appendicitis. The allocation of this form of destructive appendicitis is necessary in order to emphasize its danger. After all, the presence of perforation of the appendix is a direct evidence of the entry of its aggressive infected contents into the abdominal cavity. The risk of postoperative complications is significantly increased. Therefore, this fact must necessarily affect the volume of surgical intervention and postoperative management of the patient.
Postoperative period

Management of patients with gangrenous appendicitis in the postoperative period differs from simple forms of appendicitis:
The need for powerful antibiotic therapy (cephalosporins or levofloxacin, amikacin, ornidazole);
Adequate pain relief (narcotic and non-narcotic analgesics);
Infusion detoxification therapy (saline solutions, glucose, rheosorbilact, xylate, refortan, fresh frozen plasma, albumin);
Prevention of thromboembolic complications and stress ulcers of the stomach and intestines in people at risk (elastic bandaging of the legs, anticoagulant drugs (fraxiparine, clexane), blockers of gastric secretion (omez, kvamatel);
Daily blood tests;
Dressings. They are carried out daily. Bandages are being replaced, wounds and drains are washed, glove-gauze graduates are replaced. The wound healing process and the presence of purulent complications are assessed;
Exercise therapy, massage and breathing exercises. Their volume is determined by the general condition of the patient and the actual ability to walk. Early activation is one of the postulates of surgery for gangrenous appendicitis.
Diet for gangrenous appendicitis

With gangrenous appendicitis, disturbances in the peristaltic activity of the intestine occur. If the disease is complicated by any form of peritonitis, this leads to an even greater aggravation of peristalsis. Surgical trauma of the abdominal organs in gangrenous appendicitis is more pronounced than in its simple forms. All this leads to a slowdown in digestive processes, which is reflected in the characteristics of nutrition:
On the first day food should be kept to a minimum. Usually the appetite of patients during this period meets this requirement. You can and should drink purified and mineral water without gas, weak sweet tea, dried fruit decoction, low-fat kefir, pureed soup with potatoes and a small amount of cereal, seasoned with butter or weak chicken broth. it is better to eat 6-7 times a day for several spoons or sips;
Second days. If the postoperative period proceeds smoothly, the diet can be supplemented with mashed potatoes, mashed dietary meat of low-fat varieties, cottage cheese casserole, boiled sausages, liquid cereals with butter. In case of poor peristalsis or clear signs of persistence of the inflammatory process in the abdominal cavity, the diet is left at the same level;
Third day. Usually, during this period, the intestines are fully launched and the patient has the first bowel movement in the postoperative period. In this case, nutrition can be expanded as part of dietary table No. 5. The main rule in it: exclude spicy, fatty, smoked dishes, marinades and spices, observe a fractional, regular meal.









