Contents
G6PD and favism: what are the risks in the event of a deficiency of this enzyme?
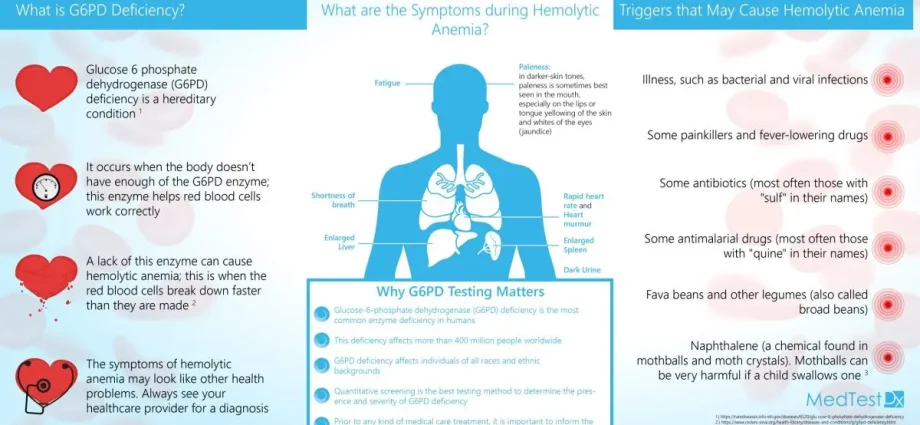
Glucose-6-phosphate dehydrogenase or G6PD is an enzyme essential for the survival of red blood cells. G6PD deficiency, or favism, is an inherited genetic disease that can be responsible for hemolytic anemia resulting from acute hemolysis (destruction of red blood cells) in oxidative stress. Certain foods such as beans or oxidizing drugs can cause this hemolysis and should therefore be avoided.
What is G6PD?
G6PD, or glucose-6-phosphate dehydrogenase, is an enzyme, present in particular in red blood cells. It plays an essential role in the reduction of oxidizing agents, such as hydrogen peroxide, highly toxic to the cell, resulting in their bursting.
If G6PD is deficient, it can no longer play its protective role, against oxidizing agents, of the main constituents of red blood cells, namely the membrane and hemoglobin. This can result in the destruction of red blood cells, also called hemolysis. Denatured hemoglobin precipitates inside the cell to form corpuscles called Heinz bodies, which in turn generate toxic oxygen free radicals. This phenomenon can be, in certain cases, very serious, even fatal, in the absence of an emergency care.
G6PD deficiency is the most common genetic anomaly, affecting around 450 million people worldwide, with a higher frequency in certain countries such as:
- those around the Mediterranean Sea: in Sardinia, for example, 25% of boys are said to have this deficit;
- from North Africa;
- sub-Saharan black Africa;
- the Near and Middle East;
- Caribbean ;
- populations of African and Hispanic origin in North and South America;
- Southeast Asia;
- South China;
- The Indies.
Until recently, the deficit was considered in France as a rare disease. We now know that it is a frequent affection, given the migratory flows to France. The number of people with a G6PD deficiency is estimated in France between 250 and 000. Men are 450 times more affected than women. Each year, 000 newborns are said to be affected by G10PD deficiency.
What are the causes of favism?
G6PD deficiency is the most common hereditary enzyme deficiency of the red blood cell. This genetic condition is linked to sex, it originates from an abnormal gene carried by the sex X chromosome, causing a range of G6PD activity from normal to severely deficient.
It is especially boys who are carriers. Indeed, women have two X chromosomes and men have an X chromosome that comes to them from their mother and a Y chromosome that comes to them from their father. The mother transmits an X to each child and the father transmits to each child either an X (he will then have a girl) or a Y (he will then have a boy). In most cases, it is the boys who are deficient in G6PD via an abnormal gene on their X chromosome that came from their mother. Girls are most often the only transmitters of the genetic defect. But there are rare cases of girls in which both X chromosomes will carry the abnormal gene.
This is a genetic peculiarity of a normal child. Indeed, the child carrying this deficit will only be sick from his deficit if he suffers from external attacks called “oxidative” caused by the ingestion of certain foods or drugs, or by a viral or bacterial infection. In this regard, G6PD deficiency is not considered a disease since the person is said to be “normal” as long as they do not encounter an oxidative agent that can trigger hemolysis.
Trigger foods
People deficient in G6PD are likely to develop acute hemolysis after ingestion of certain foods such as:
- Vicia faba beans, the vegetable that gave the disease the name of favism, regardless of their method of preparation and consumption;
- drinks containing quinine;
- vitamin C-based food supplements.
Drugs and chemicals
Certain drugs and chemicals, which produce peroxides and lead to oxidation of hemoglobin and the red blood cell membrane, may be responsible for hemolysis in people who are deficient in G6PD:
- the primaquine;
- salicylates;
- sulfonamides;
- nitrofurans;
- the phénacétine;
- naphthalene;
- certain vitamin K derivatives;
- la dapsone;
- the phénazopyridine;
- nalidixic acid;
- methylene blue.
Some of these drugs have been associated with cases of acute hemolysis when used in doses above the recommended doses. Also, it is all the more important with these drugs to strictly follow the dosage and never exceed the maximum recommended doses. In all cases, it is recommended to be vigilant as to their composition. Medicines may contain several active substances, including a risky active substance. Any self-medication is therefore not recommended. It is best to seek the advice of a doctor or pharmacist before taking any over-the-counter medication.
What are the symptoms of favism?
The vast majority of people with G6PD deficiency remain asymptomatic. Indeed, in the absence of “oxidative” aggression, there is no consequence of this enzymatic deficit.
When it occurs, the extent of hemolysis depends on the extent of the G6PD deficiency and the oxidizing power of the trigger product. Indeed, given that more than 200 G6PD variants have been identified, the manifestations of this deficiency are very different from one person to another and the foods or drugs that trigger them may not be the same in all patients. . A haemolytic accident can occur late in the life of a deficient subject and even after several prior exposures to oxidizing agents without apparent consequences. Conversely, a newborn or deficient infant, who is breastfed, can be reached through maternal exposure to oxidizing agents.
The World Health Organization has classified G6PD deficits into 3 classes according to the level of residual G6PD activity:
- class 6 G1PD deficiency, which corresponds to the lowest level of residual activity. Exceptional (1 to 2%), it is severe and results in chronic hemolytic anemia with a sometimes dramatic decrease in the blood’s capacity to transport oxygen;
- Class 2 (3 to 10%) and 3 (10 to 60%) deficits are characterized by a risk of acute hemolytic accident secondary to oxidative stress and a risk of neonatal jaundice (jaundice) caused by the degradation of the hemoglobin contained in red blood cells.
When hemolysis is significant, it can lead to:
- severe and rapid onset anemia, shock, and severe cardiac and renal consequences;
- chronic hemolytic anemia, of varying severity from one patient to another;
- neonatal jaundice, with, in the most severe and untreated cases, neurological sequelae.
Symptoms leading to a consultation
A few hours, or even one or two days after taking a triggering agent (food or medication), a sudden hemolysis crisis can occur with the appearance of:
- fever;
- pallor;
- headache;
- tired ;
- unexplained anorexia;
- faintness (sudden discomfort without loss of consciousness);
- loss of consciousness ;
- abdominal and lower back pain;
- emission of dark urine in red “port” or even black, sign of hemoglobinuria, that is to say of the elimination of hemoglobin in the urine.
How to cure a favism?
Prevention
Management is essentially based on prevention. Individual tolerance being unpredictable, subjects deficient in G6PD must imperatively follow the recommendations of the lists of drugs and dangerous foods:
- excluding certain foods: beans, whatever their form (especially raw beans), drinks containing quinine such as Gini © or Schweppes ©, high doses of vitamin C (fortified drinks, food supplements );
- by avoiding, as far as possible, the taking of certain drugs: some of them, such as sulfonamides, are formally contraindicated and should never be prescribed in a deficient; others, such as aspirin, are only dangerous if prescribed in doses higher than usual doses;
- avoiding certain substances or products, such as naphthalene or henna;
- in lactating women, mothers of a child carrying or suspected of G6PD deficiency, the intake of any treatment or food likely to expose to a risk of hemolysis should be avoided;
- in heterozygous pregnant women or having had a child diagnosed with G6PD deficiency, the same prohibitions and precautions apply as a precautionary measure since the fetus may be deficient in G6PD.
These drugs, health products and foods that are dangerous for people with G6PD deficiencies must appear on a document that each deficient and their parents must carry with them in order to be systematically presented to any health professional who will be required to treat the person (attending physician , surgeon, dentist, nurse, pharmacist, school doctor, etc.). There is an official care, information and emergency card.
Management of hemolysis
The hemolytic accident linked to G6PD deficiency usually resolves spontaneously within a few days thanks to the production of new red blood cells by the bone marrow. Transfusion is only necessary in severe cases. In the most severe forms, it may be necessary to have recourse to exsanguino-transfusion in addition to intensive care.
Management of jaundice
Moderate neonatal jaundice is treated with phototherapy, that is, treatment by exposure to light rays. Exsanguinotransfusion may sometimes be necessary in certain severe forms.