Contents
Pararectal fistula occurs due to a violation of metabolic processes in the fiber around the ampoule of the rectum. Most often, this occurs against the background of paraproctitis or proctitis, a symptom of which is a fiber abscess.
The main manifestations of the fistula of the anus are purulent or spotting, pain, itching, irritation of the epidermis of the perianal region.
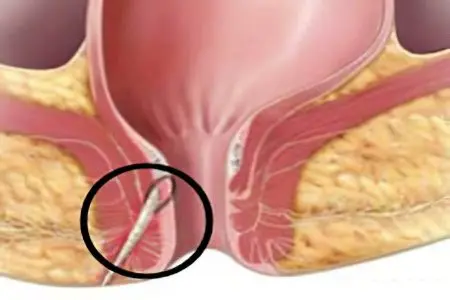
Regardless of the location, a pararectal fistula is a canal that connects the ampulla of the rectum or the area near the anus with nearby hollow organs.
Causative agents of paraproctitis:
coli,
staphylococcus,
Streptococcus,
clostridia,
Tuberculosis.
A fistula of the rectum is a consequence of acute or chronic proctitis, covering the anal crypts (anal sinuses), the space between the sphincters and the tissue around the rectum. The anal crypt, affected by proctitis, becomes one of the fistula openings, located in the thickness of the fiber.
Pararectal fistula is characterized by frequent relapses, it torments the patient, proceeds with severe local symptoms, and significantly worsens the general state of health. If the disease lasts long enough, the patient’s anal sphincter is deformed, and the risk of developing an oncological lesion of the lower intestine increases.
Classification of pararectal fistulas
Depending on the clinical picture, the following forms of pararectal fistula are distinguished:
Incomplete fistula – a variety that does not have access to the surface. The channel ends in pararectal tissue, this is an intermediate stage before the formation of the full form. If purulent processes develop, an incomplete fistula finds a way out, transforming into a complete one.
A complete fistula has one or more inlets that start on the wall of the rectum and one outlet that ends in the skin near the anus.
Classification by localization relative to the sphincter:
Intrasphincteric localization – the fistula has a straight channel, an internal opening in one of the crypts, an external opening near the anus.
Transsphincteric localization – the fistula has branched passages, purulent pockets in the pararectal tissue, scars form in the surrounding tissues. The fistula channel is located under the skin, on the surface or deep in the sphincter.
Extrasphincteric localization – a fistula occurs as a result of acute paraproctitis, has a long tortuous course, several exits. The internal opening opens in the area of the anal sinus (crypt).
The degree of complexity of extrasphincteric fistula:
The first degree – the fistulous course is straight and narrow, there are no scars, no infiltration, no abscesses.
Second degree – the inner hole is surrounded by scar tissue, there are no signs of inflammation.
Third degree – there is no scar tissue, an inflammatory process develops in the fiber with the formation of pus.
Fourth degree – the fistula has an enlarged internal opening, infiltrates, scar tissue.
Causes of the fistula of the rectum

The vast majority of cases of pathology is a complication of acute paraproctitis. Due to the penetration of infection into the pararectal tissue, an abscess forms in the wall of the rectal ampulla. When it opens, a fistulous tract is formed. Such a complication is diagnosed if the patient does not see a doctor in time, or the surgeon limits the radius of the surgical intervention.
Diseases or conditions leading to the appearance of a fistula:
Trauma or resection of the rectum;
Complication of childbirth;
Breech presentation of the fetus, ruptures of the birth canal;
Complication after gynecological operations;
Crohn’s disease;
Tuberculosis of the rectum;
Rectal cancer;
Diverticulosis of the rectum;
AIDS;
syphilis;
Chlamydia.
Symptoms of an anal fistula

At the beginning of the disease, a fistulous opening appears on the skin near the anus. Pus and ichor are released from it, they stain the linen, and these traces cannot be overlooked. The patient has to use pads, wash the perianal area, take a sitz bath. These symptoms are accompanied by itching, maceration of the skin due to constant exposure to secretions, and an unpleasant odor.
With good drainage of the fistula, the pain is felt weakly. It intensifies with chronic inflammation of an incomplete fistula, becomes intense with defecation, coughing and long walking.
Periods of exacerbation are followed by periods of remission. An exacerbation occurs if the fistulous passage is clogged with a purulent mass, necrosis and granulation products. As a result, an abscess is formed, it spontaneously opens, and the separation of pus and ichor is temporarily reduced. Despite this, the external opening of the fistula never heals, after some time the exacerbation is repeated.
During remission, if the patient carefully observes hygiene, he does not feel severe pain or unpleasant symptoms.
However, a long-term disease with frequent exacerbations leaves the following symptoms:
Insomnia,
hyperthermia,
Weakness,
Nervousness,
Headache,
Asthenization.
Tissue changes resulting from a long course of complex forms of the disease:
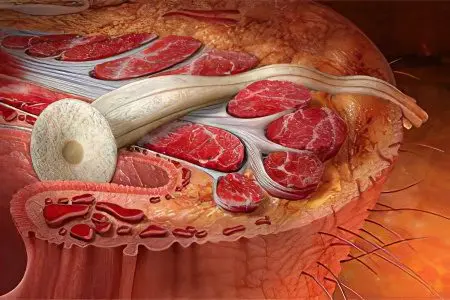
Insufficiency of the anal sphincter;
Deformation of the anal canal;
Scarring of the sphincter muscles;
Pectenosis – scarring of the anus canal;
Anal stricture.
Diagnostics

A complete fistula can be diagnosed by visual inspection. On the skin near the anus of the patient there is a fistula opening, from which pus and bloody mucus are discharged. If the fistula has one hole, this is a consequence of acute paraproctitis. Two openings of the fistulous canal to the right and left of the anus are symptoms of a horseshoe-shaped pararectal fistula.
The dependence of the nature of the discharge on the form of the fistula:
Odorless yellow pus – condition after paraproctitis;
Abundant liquid discharge – tuberculous lesion;
Scanty crumbly discharge – fistula after actinomycosis;
Bloody or sanious discharge is a possible consequence of the malignancy of the fistulous process.
If the fistula has become incomplete, rectal digital examination reveals a single internal opening. Women suffering from this disease must be examined by a gynecologist to exclude a fistula of the vagina.
Additional diagnostic methods and their purpose:
Probing – determining the direction and branching of the fistula, its localization relative to the sphincter;
Anoscopy – the study of the shape and extent of the fistulous canal;
Fistulography – an x-ray study with a contrast agent to determine the volume of the fistula;
Sigmoidoscopy – assessment of the condition of the mucosa, detection of tumors;
Irrigoscopy – differentiation from diseases with similar symptoms (pararectal fiber cyst);
Sphincterometry – the study of the functionality of the anal sphincter;
Ultrasonography is a complex diagnostics.
Treatment of a fistula of the rectum

For a complete cure for a fistula, there is only one radical method – this is surgical intervention. The operation is not performed when closing the holes during remission, because in this case it is impossible to assess the affected area, it is possible to damage healthy tissues, or not completely excise the fistulous tract.
With an exacerbation of paraproctitis, the surgeon opens the abscess, eliminates pus, and prescribes treatment with antibacterial agents to the patient. Additionally, physiotherapeutic procedures (UVI, electrophoresis) are used. As soon as the inflammatory process subsides, the fistulous canal is excised.
Methods of surgical intervention:
Dissection of the fistula into the lumen of the rectum;
Opening of purulent streaks;
Drainage of infiltrates;
Sphincter closure;
Closure of the fistula opening with a flap of its own muscle and mucous tissue.
The surgeon chooses the technique of the operation depending on the degree of damage and localization of the fistula relative to the sphincter.
After surgery, there may be complications in the form of insufficiency of the anal sphincter, as well as relapses of the disease. Their probability is significantly reduced with timely treatment and the correct operation technique.
Forecast and prevention of adrectal fistula
They respond well to treatment and rarely recur in intra- and transsphincteric fistulas of low localization. Deep extra- and transsphincteric fistulas are characterized by a long course of the disease and frequent relapses.
To avoid the appearance of pathology, you need to try to exclude injuries to the rectum, treat paraproctitis in a timely manner.









