Contents
What is embolism?

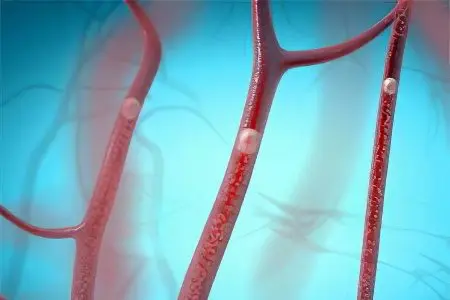
Embolism – this is a pathology, exclusively, of the arterial vascular bed, which is based on the overlap of its lumen at a certain level with partial or complete cessation of blood flow, caused by factors not related to the pathology of the affected vessel. Emboli are those substances of the internal environment of the body or the environment that block the vascular lumen. It means that:
Embolism is caused by the entry or migration of emboli into the arteries of the systemic or pulmonary circulation from other parts of the vascular bed;
Emboli can be of a different nature: blood clots, blood clots, detached atherosclerotic plaques, fat cells and oily solutions, air;
Sources of emboli can be arterial and venous vessels of any localization, as well as the heart;
The diameter of the embolus determines the caliber of the artery that it will block;
It is impossible to predict in which particular pool of the arterial vascular bed the embolus will fall.
The pathogenesis of embolism can take place in three ways:
The source of emboli are arterial vessels. In this case, the pool in which the breakdown occurred is affected. At the same time, a thrombus or atherosclerotic plaque, breaking away from its place in a vessel of large diameter, becomes an embolus and migrates to smaller vessels in the pool of its branching;
The source of emboli are venous vessels. In their role can be blood clots, air, fat cells. Their migration is a little more complicated, since they first enter the heart from the veins, from where they are ejected in any direction (brain, limbs, intestines, kidneys, etc.);
The source of emboli is the heart. These are, as a rule, small blood clots that form against the background of arrhythmias. After they break away from their usual place of localization, they migrate to any arterial vessels.
Embolism is always an acute condition requiring urgent measures. The entry of emboli into arterial vessels leads to the cessation of blood flow. This is fraught with the occurrence of ischemia, which can turn into gangrene or organ infarction (within 6-12 hours). This feature distinguishes it from arterial thrombosis, which is a chronic process that compensates for the lost blood flow due to collateral (additional) vessels.
Types of embolism
The classification of embolisms is based on the type of embolus and its final localization after the cessation of migration. The main types of embolism are shown in the table.
Type of embolism according to the origin of the embolus | Type of embolism according to the location of the embolus |
Thromboembolism (thrombi of arteries, veins and heart act as an embolus) |
|
Air and gas embolism (emboli form when air enters the veins or from bubbles of blood gases) | |
Fat embolism (emboli are fat cells or substances) |
From the table it becomes obvious that, regardless of the nature of the embolus, any of the arterial type vessels can be its final localization.
Fat embolism
Fat embolism occurs as a result of the penetration of fat droplets from molten or destroyed fat cells in the body into the venous bed. This is possible with massive injuries (injuries to bones and soft tissues of the extremities, pancreatic necrosis). Another source of fat embolism can be intravenous fat solutions, which are not intended for this method of administration. Once in the bloodstream, fat droplets are unable to dissolve in the blood. Their spread throughout the arterial bed leads to the accumulation of fatty particles in certain places. If they become larger than the diameter of the vessel, this leads to signs of impaired blood flow. As a rule, fat embolism is relatively mild, as it affects small vessels.
Air and gas embolism
It is the overlapping of the lumen of arterial vessels with air or gas bubbles. This is possible with damage to large veins, especially in the neck. If such a wound is not closed in time, and the vein is compressed, this can result in air being sucked into its lumen, which will enter the heart with blood flow and spread throughout all arterial pools. As for the possibility of an air embolism from air entering the syringe or system during intravenous manipulations, this is practically impossible. For the occurrence of clinical manifestations of air embolism, its amount should be about 20 ml.
Gas embolism occurs without violating the integrity of blood vessels. Sudden changes in atmospheric pressure are to blame for its origin. This is possible in scuba divers and is called decompression sickness. If a diver quickly rises from a great depth, the gas mixture he inhales does not have time to assimilate as quickly as it happened at high depths. As a result – undissolved air bubbles that block small arterial vessels throughout the body.
Pulmonary embolism
One of the most frequent and formidable embolism is pulmonary embolism. In most cases, it is represented by thromboembolism. Regardless of the specific nature of the embolus, the manifestations of the disease in lesions of vessels of a certain diameter will be identical. On this basis, pulmonary embolism is classified as follows:
Embolism of the central trunk of the pulmonary artery;
Embolism of large branches of the pulmonary artery;
Embolism of small branches of the pulmonary artery.
The most formidable condition is the first type of disease. This is due to the possibility of reflex cardiac arrest at the time of embolism as a result of the pulmocoronary reflex. This is only possible with thromboembolism, when large heart clots become emboli and are fixed at the mouth of the pulmonary artery. Air and fat embolism affect only small branches of the pulmonary artery and do not cause severe manifestations. The exception is cases of massive ejection of small blood clots with constant new ejection from the heart. The defeat of large branches of the pulmonary artery often ends in death due to the development of acute cardiopulmonary failure or pulmonary infarction.
Embolism of arteries and vessels
Its most dangerous types are thromboembolic lesions of the arteries of the brain, intestines and kidneys. In all cases of damage to large main vessels, necrosis of the corresponding organ occurs within a short time (kidney infarction, intestinal gangrene, brain stroke). This will either lead to severe disability or death. The embolisms of the peripheral arteries of the extremities are much easier. Usually, they are easy to diagnose, since such conditions occur very acutely and are accompanied by a vivid clinical picture. Timely intervention, surgical intervention, prevents serious consequences. Otherwise, gangrene of the limb occurs.
Causes of embolism
Each type of embolism has its own causes.
For thromboembolism:
Atrial fibrillation and other cardiac arrhythmias;
Myocardial infarction;
Endocarditis;
Aneurysm of the left ventricle;
Hypercoagulability of blood;
Diseases of the venous system of the pelvis and extremities (thrombophlebitis, varicose veins, post-thrombophlebitic syndrome);
Major operations on the organs of the pelvis, abdomen and limbs;
For air embolism:
Traumatic damage to large veins;
decompression sickness;
Gross violations of the technique of intravenous manipulation;
Surgical interventions in gynecology with a violation of the technique of their implementation, abortions and difficult births.
For fat embolism:
Massive injuries to the limbs;
Intravenous administration of prohibited fat-containing drugs;
Severe pancreatic necrosis.
Symptoms of an embolism
The symptoms of embolism are well described in the table below:
Embolism localization | Symptoms |
pulmonary artery |
|
Carotid artery |
|
mesenteric artery |
|
renal artery |
|
Limb arteries |
|
Embolism treatment
Since embolism is an acute disease, its treatment requires urgent measures. The sooner they are provided, the better the prognosis for the patient. Differentiated treatment tactics are shown in the table.
Type of embolism | Complex of therapeutic measures |
Thromboembolism |
|
Air embolism |
|
Fat embolism |
|
Prevention of embolism

Preventive measures consist of several sections.
Prevention of thromboembolism:
taking anticoagulants (aspirin, cardiomagnyl, warfarin);
Control of blood coagulation parameters (APTT, PTI INR), especially in persons at risk for thromboembolic complications;
Timely and adequate treatment of cardiac arrhythmias;
Elimination of venous pathology of the lower extremities;
Installation of cava filters in persons at risk;
Elastic compression of the legs and prophylactic doses of anticoagulants in individuals at risk who are to undergo surgery;
Dosed physical and mental stress.
Prevention of air embolism:
Compliance with the rules for a smooth ascent from high depths by divers;
Correct and fast treatment of wounds with damage to venous vessels;
Proper laying of women on the operating table during gynecological operations, careful and quick ligation of damaged veins;
Strict adherence to the technique of performing intravenous injections;
Prevention of fat embolism:
Injury prevention;
Fast and permanent immobilization of the injured limb;
Early surgical interventions or other methods of reposition, leading to stabilization of bone fragments;
Compliance with the rules of intravenous administration of drugs.









