Contents
With the external form of hydrocephalus, excessive formation of cerebrospinal fluid occurs, which normally circulates in the structures of the brain and spinal cord and protects it from mechanical damage. In addition, cerebrospinal fluid supplies the brain with food and removes metabolic products into the blood. As a result of pathological pressure, brain tissue atrophies, negative symptoms occur, and complications increase the risk of coma and death.
Classification of forms of the disease
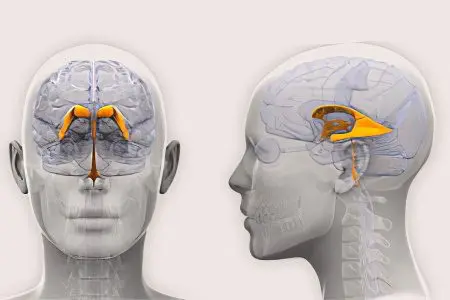
External hydrocephalus is a form of dropsy of the brain, which consists in excessive accumulation of cerebrospinal fluid (CSF) in the subarachnoid and subdural space of the brain. The subarachnoid cavity is located between the pia mater and arachnoid membrane of the brain and spinal cord. The narrow slit-like subdural cavity is located between the dura mater and the arachnoid. It is permeated with connective tissue fibers.
Types of external hydrocephalus:
Open form – communication of CSF circulation pathways is not disturbed, changes affect the mechanism of absorption of cerebrospinal fluid;
Closed form – there is no message between the spaces in which the cerebrospinal fluid is concentrated and the ways of its circulation;
Hypersecretory form – the production of cerebrospinal fluid is excessive;
The external replacement form – the medulla (parenchyma) is transformed, undergoing atrophy, and cerebrospinal fluid takes its place.
Classification of external hydrocephalus according to the rate of flow:
Acute – from the first signs to the initial decompensation, no more than 3 days pass;
Subacute – lasts for a month;
Chronic – lasts from 3 weeks to six months or more.
According to the level of pressure of the cerebrospinal fluid, it is divided into hypotensive, hypertensive and normotensive forms. The latent course of the disease, which lasts long enough with normal intracranial pressure, is the most dangerous, since the symptoms of the pathology can increase suddenly and avalanche-like without any visible prerequisites. Most often, this situation occurs with external replacement hydrocephalus.
There are congenital and external forms of dropsy of the brain. The congenital form occurs in the process of intrauterine development, acquired hydrocephalus – as a result of trauma or inflammation of the brain structures.
Symptoms of external hydrocephalus

The human body has impressive compensatory abilities. A mild form of external hydrocephalus can go almost unnoticed for the patient – the circulation of cerebrospinal fluid is restored independently. The prognosis of such a disease is the most optimistic, and its consequences are minimal.
An increase in intracranial pressure leads to the following symptoms:
Headache aggravated after a long stay in a horizontal position;
Nausea and vomiting;
Drowsiness;
visual disturbances (double vision);
Increased fatigue;
Weakness.
All these manifestations are a consequence of a decrease in the density of brain structures due to the fact that they are saturated with cerebrospinal fluid, narrowing of the subarachnoid and subdural space, and improper resorption of cerebrospinal fluid. With the replacement of the cerebral parenchyma with CSF, the symptoms of the disease are exacerbated.
Symptoms of replacement external hydrocephalus:
Violation of large and small motor skills;
Uncertain unsteady gait;
Involuntary urination and fecal incontinence;
Violations of intellectual activity, memory, attention;
Signs of dementia.
If external hydrocephalus is diagnosed in an infant, the following symptoms occur:
Divergence of sutures between the bones of the skull;
Swelling of fontanelles;
Enlargement of the frontal part of the skull;
Lack of appetite;
Swelling of the veins on the skull, clearly visible under thin, stretched skin in the form of a venous network;
Excessive increase in the circumference of the child’s head.
Causes of the disease

Any disruption in the normal functioning of the brain structures can lead to the development of the disease.
Causes of external hydrocephalus:
brain injury;
Consequences of injuries and fractures of the spine;
Tumors of any etiology;
Stroke, hematoma, cerebral hemorrhage;
Consequences of inflammatory processes or neuroinfections (meningitis, meningoencephalitis, tuberculosis, herpes, toxoplasmosis);
Pathology of the cervical vertebrae;
Diseases of the circulatory system;
Age-related changes in brain structures;
Congenital anatomical changes in the central nervous system.
Diagnosis of external hydrocephalus

The most informative diagnostic method is magnetic resonance imaging, or MRI. A little less information can be obtained as a result of CT, or computed tomography.
What can be seen during an MRI:
Contours of the skull, ventricles, subarachnoid space, brain;
The presence of anomalies – cysts, tumors, hematomas, aneurysms;
The shape and size of the ventricles.
In addition to tomographic diagnostic methods, the following studies are prescribed:
Radiography of the cisterns of the base of the skull – allows you to clarify the type of hydrocephalus, pkti circulation of the cerebrospinal fluid;
Angiography, or X-ray of blood vessels – diagnoses pathologies of the blood supply to the brain;
A blood test for the presence of antibodies to possible infectious agents that have affected the development of the disease.
In addition to the appointment of instrumental methods, the doctor conducts a neuropsychological examination, which allows to clarify the symptoms of the disease, the time of their appearance.
Possible treatment options for external hydrocephalus

If the diagnosis of the disease revealed a moderate degree of external hydrocephalus, the neurologist determines the drug treatment regimen. The goal of therapy is to restore the functioning of the cerebral vessels and the activity of the central nervous system.
The patient takes diuretics (Diakarb) in combination with drugs that compensate for the excessive removal of potassium and magnesium from the body, vitamin complexes, nootropics, vasodilators.
Additional treatments:
Manual therapy;
Special diet and diet;
Salt and coniferous baths
Physiotherapy.
If within 2-3 months there is no improvement in performance, or the patient’s condition worsens, surgical treatment is performed.
Methods of surgical intervention:
Shunting to remove excess cerebrospinal fluid;
An endoscopic operation to create additional pathways for the outflow of cerebrospinal fluid into the cisterns of the brain, designed to absorb this fluid in a natural way.
The result of these operations is the restoration of normal CSF circulation, improvement of the quality of life of the patient, in some cases – complete compensation of the condition.









