Contents
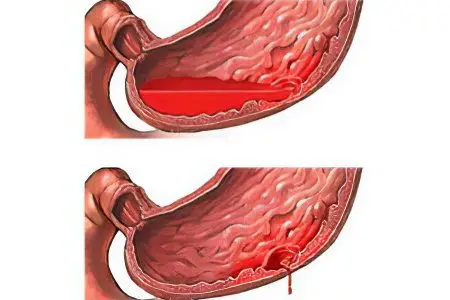
The main difference between erosive gastroduodenitis and other forms of this pathology is the presence of ulcers and erosion against the background of inflammation of the mucous membrane of the stomach and duodenum. At the same time, the normal functioning of the glands of the gastrointestinal tract is maintained.
Erosive gastroduodenitis is diagnosed mainly in young women and men. With this disease, superficial defects occur on the mucous membrane. Ulcers and erosions do not penetrate into the submucosal and muscular layer, they can be single or multiple. Erosive gastroduodenitis is accompanied by bleeding from mucosal defects, which eventually leads to anemia.
If the patient does not receive adequate treatment, the pathological process is complicated by the development of stomach ulcers and upper intestines, cholecystitis, pancreatitis. This form of gastroduodenitis is the most common among all pathologies of the gastroduodenal zone, the disease can be both acute and chronic. Compared with ordinary gastritis, erosive gastroduodenitis does not go into remission for a long time, it is difficult to treat.
Causes of erosive gastroduodenitis

The pathological process is based on the aggressive influence of hydrochloric acid against the background of its excessive secretion. The epithelial layer of the mucous membrane does not have the ability to regenerate, as a result of which erosion and ulcers appear on it.
Negative factors provoking the development of erosive gastroduodenitis:
Genetic predisposition;
Infection with the bacterium Helicobacter pylori;
Irrational nutrition;
Frequent stress and psycho-emotional upheaval;
intestinal infections;
Poisoning by poor-quality products;
Diseases of neighboring organs of the gastrointestinal tract (liver, pancreas);
Reflux (reverse throwing) of acid from the duodenum into the stomach;
Side effects of drugs from the group of NSAIDs, antibiotics, glucocorticosteroids;
Eating spicy, rough, too hot or too cold food;
Alcoholism.
Infection with the bacterium Helicobacter pylori is the most common cause of the development and progression of the disease.
How is erosive gastroduodenitis manifested?

The clinical picture of the disease depends on the form in which it proceeds. Acute erosive gastroduodenitis occurs most often due to poisoning with toxins or poor-quality food. The chronic form is the result of an imbalance between damaging factors and the protective function of the mucous membrane.
The main and most striking symptom is constant or periodic pain in the epigastric region. It occurs immediately after eating or after a few hours.
Other symptoms:
Sour eructation;
Nausea;
Heartburn;
Bloating;
Frequent constipation;
Decreased appetite;
Vomiting of mucus with blood clots or acidic contents (with exacerbations);
Black loose stools (with internal bleeding);
Deterioration of general well-being (weakness, headache, insomnia).
With frequent gastric and duodenal bleeding, the patient develops anemia.
Symptoms of anemia against the background of chronic gastroduodenitis:
Dizziness;
Tachycardia;
Fast fatiguability.
In the chronic form of pathology with mild changes in the mucous membrane, the symptoms are muffled. Patients notice that they have a serious disruption of the gastrointestinal tract only at the sight of black feces.
Diagnostics

The best method for diagnosing erosive gastroduodenitis is esophagogastroduodenoscopy, or EGDS. The study is carried out using an endoscope armed with a microscopic camera. The purpose of endoscopy is to determine changes in the mucosa associated with the inflammatory process, as well as to assess the size and location of erosions.
What the doctor sees during the study:
Hyperemia and edema of the mucous membrane of the stomach and duodenum 12;
Looseness of the mucosa and increased sensitivity to touch;
Bleeding in the area of erosion;
Small hemorrhages;
Gray plaque on erosion in the form of a film;
The size of defects is 0,3-0,5 mm.
During endoscopy, the doctor performs a biopsy of the mucosal area for histological examination and clarification of structural changes.
Diagnosis of the presence of Helicobacter pylori:
Microscopic examination of a biopsy from the stomach and upper intestine;
PCR test – search for bacterial DNA by the presence of DNA polymerase;
Breath test – collection of air exhaled by the patient before and after exercise;
ELISA method – a study of blood serum for the presence of antigens in it to a bacterial agent.
Diagnosis of anemia is carried out using a complete blood count. When confirming hemorrhagic anemia, the color index sharply decreases, the level of hemoglobin and erythrocytes falls.
Treatment of erosive gastroduodenitis

Dietary nutrition, a rational diet are an indispensable condition for the effective treatment of this pathology. Of particular importance is the diet and content of the menu during exacerbations of the disease.
Diet requirements:
Exclusion of fatty and fried foods;
Refusal of hot spices and spices;
Food should not contain coarse fiber, be too hot or cold;
The daily volume of food is divided into 5-6 meals.
If Helicobacter pylori is detected, it is eradicated using first and second line therapy:
The first line is a complex of drugs, including Clarithromycin, Amoxicillin and proton pump inhibitors (Omeprazole, Rabeprazole).
The second line (used when the first line is ineffective) is a complex of drugs, including Tetracycline, Metronidazole, bismuth preparations, antisecretory agents.
Additional medicines:
To protect the mucous membrane – alginates, antacids;
To create a film over erosion that protects against the action of gastric juice – cytoprotectors;
To improve regeneration – reparants, vitamin preparations;
To reduce pain – antispasmodics (papaverine, drotaverine hydrochloride);
To relieve stress – sedatives.
Prophylaxis and prognosis
To avoid the development of the disease, you need to carefully compose your menu, adhere to the correct diet, do not eat too hot or cold food. When taking NSAIDs and glucocorticosteroids, it is necessary to strictly observe the dosage and follow the doctor’s recommendations. When the first symptoms of the disease appear, you need to contact a gastroenterologist and undergo a study for the presence of Helicobacter pylori.
The prognosis of erosive gastroduodenitis is favorable with timely treatment. Otherwise, the patient is at high risk of developing stomach and duodenal ulcers.









