Contents
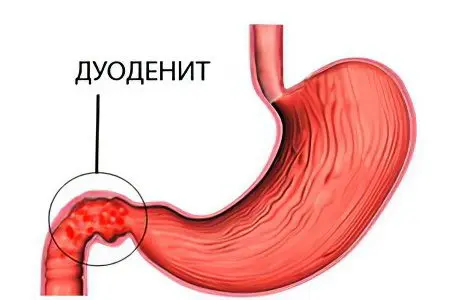
Duodenitis – This is an inflammation of the mucous membrane of the duodenum 12. The disease occurs frequently, in about 5-12% of people. In women, pathology is diagnosed less frequently than in men by about 2 times. This is due to the fact that males are more prone to bad habits.
Duodenitis can be acute, or it can become chronic. Acute inflammation develops when the body is poisoned, when eating spicy dishes that contribute to intestinal irritation. Erosions are formed on it, which heal without leaving scar areas behind. The severe course of the disease can lead to the formation of purulent phlegmon. If you follow medical recommendations and stick to a diet, then you can cope with the pathology in 7-14 days. The probability of transition of duodenitis into a chronic form when it occurs again is 90%.
Chronic duodenitis manifests when a person has other pathologies of the digestive system, for example, pancreatitis or gastritis. Serious errors in the diet can also provoke a disease. As the disease progresses, the duodenal mucosa begins to atrophy or become covered with erosions. The chronic course of duodenitis is accompanied by periods of exacerbations that occur when the body is exposed to negative factors. Dealing with a chronic form of the disease is more difficult than with an acute one.
Causes of acute duodenitis

The following reasons can provoke the development of acute duodenitis:
Eating fast food, as well as foods that can irritate the intestinal mucosa. It can be coffee, fried, spicy and fatty foods. In order for this food to be digested, a significant amount of hydrochloric acid is needed. It, in turn, negatively affects the protective functions of the intestine.
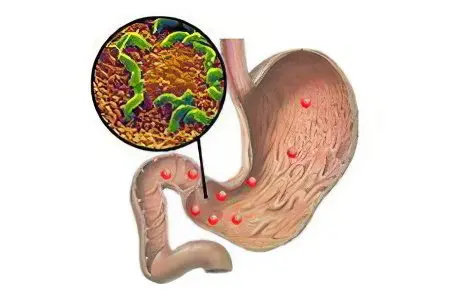
Food poisoning, which was caused by pathogenic microflora: staphylococci, streptococci, clostridia, enterococci. Infection with Helicobacter pylori, Giardia and helminths can also cause acute duodenitis. Microbes lead to the development of local inflammation, the production of bile and pancreatic juices is disrupted. All this is the basis for the occurrence of duodenitis.
Reflux or backflow of intestinal contents into the duodenum. The cause of this pathology is a violation of the patency of the small intestine, for example, due to a growing tumor. Bacteria that live in the small intestine enter the duodenum, causing it to become inflamed.
Alcohol abuse.
Ingestion of substances that can provoke a burn of the mucous membranes into the digestive tract. These can be acids, alkalis, chlorine-containing agents.
Mechanical damage to the duodenum due to the ingress of foreign objects into it.
Causes of chronic duodenitis
To provoke a chronic form of the disease are capable of factors such as:
Intestinal diseases, which lead to a deterioration in its contractility, to congestion, overstretching of the walls of the organ and atrophy of its mucous layer. These include prolonged constipation, intestinal adhesions, disruption of its blood supply, problems with nervous regulation.
Pathology of the liver, gallbladder, pancreas. All these violations affect the functioning of the 12 duodenal ulcer.
Allergy to food.
Prolonged emotional upheaval.
Taking medications for a long time.
Adherence to bad habits: substance abuse, smoking, alcoholism.
Symptoms of duodenitis

Since duodenitis is often combined with diseases of the digestive system, for example, with gastritis or with a stomach ulcer, its symptoms directly depend on the specific pathology.
The main manifestations of the disease in adults include:
Pain in the epigastric region, which becomes more intense when probing the abdomen. Depending on the nature of the course of the pathology, the pain will have the following features:
If duodenitis has a chronic course, then the pain will be present on an ongoing basis. It becomes more intense when a person is hungry. It has the character of seizures, occurs 2 hours after eating.
If duodenitis develops due to intestinal obstruction, then the pain bursts the stomach from the inside, has the character of attacks, manifests itself after the intestines are full.
If duodenitis occurs against the background of gastritis with high acidity, then pain appears 20 minutes after eating, when food enters the duodenum.
If the disease is provoked by Helicobacter pylori, then the pain will be especially strong on an empty stomach.
If there is a violation of the outflow of bile from the gallbladder, then the area around the Vater nipple becomes inflamed. The pain is intense, reminiscent of an attack of hepatic colic. Discomfort occurs in the right hypochondrium.
Increased fatigue and weakness. This is due to the effect of toxins on the body. They are formed as a result of an inflammatory reaction.
Body temperature can rise up to 38 °C.
Digestive processes are disturbed, this is manifested by such symptoms as:
Nausea.
Decreased appetite.
Increased gas formation.
Belching. In this case, a bitter taste occurs in the mouth, which is due to the ingress of bile into the stomach and back.
Constipation or diarrhea.
The skin and mucous membranes may turn yellow. Puffiness of the Vater nipple leads to the fact that the lumen of the bile duct is clogged, bile enters the bloodstream and accumulates in it.
dumping syndrome. It develops after eating a large amount of food. When the duodenum is full, the blood flow is redistributed in a different way. There is an outflow of blood from the head and its rush to the digestive organs. Therefore, a person experiences dizziness, heaviness in the abdomen, drowsiness, fever in the upper half of the body.
Sometimes duodenitis does not manifest itself. The disease can be detected by chance, after gastroduodenoscopy.
Diagnostics

The reception of the patient begins with a survey of his complaints and examination. The doctor palpates the abdomen. In the area of the 12 duodenal ulcer, pain occurs.
To confirm the diagnosis, the doctor will refer the patient to such instrumental examinations as:
Fibrogastroduodenoscopy. During its implementation, the stomach and duodenum are examined. If there is inflammation, then the mucous membranes of the organ will be swollen and red.
Depending on the form of the disease, its clinical manifestations will differ:
Superficial duodenitis is expressed by redness of the intestinal epithelium.
With an erosive form of the disease, the intestines will be covered with erosions.
If the folds of the organ are smoothed, then this indicates a decrease in its tone.
Nodules appear with the nodular form of inflammation.
Hemorrhagic duodenitis is accompanied by the appearance of bruises on the mucous membrane.
Atrophy of intestinal cells is observed in the atrophic form of the disease.
X-ray with the use of a contrast agent. Barium sulfate is used as a contrast. During the study, violations in the structure and functioning of the intestine are detected.
This is manifested by such signs as:
If there are zones of narrowing, then this will indicate adhesions, tumors or anomalies in the development of the intestine.
If areas of expansion are found, one can suspect a decrease in the tone of the organ, blockage of the intestines located below, a violation of the patency of food, and malfunctions in the nervous regulation of the organ.
Ulcers and erosions are manifested by a symptom of a niche.
The accumulation of gases in the duodenum 12 is a sign of its obstruction.
The absence of folds on the epithelium of the organ is a sign of inflammation and swelling.
If the contents of the duodenum are thrown into the stomach, this may indicate reflux.
In addition to instrumental examination, the patient will have to pass the following tests:
Blood for general analysis. In patients, an increase in ESR is found, which indicates inflammation. If a person develops anemia, then this is a signal of bleeding.
Blood for biochemical analysis. At an early stage of the development of the disease, the level of alkaline phosphatase and enterokinase increases, as the pathology progresses, their values decrease.
Feces for occult blood. It will be detected in the analysis when the patient develops erosive duodenitis.
Features of the course of the disease in childhood

Duodenitis in childhood most often develops due to excessive consumption of dry foods, with pronounced errors in the child’s diet. However, allergies, hereditary predisposition, infestation with parasites and infectious diseases cannot be ruled out.
Children often misread body signals and indicate that they have a stomach ache. Common symptoms of pathology include nausea, weakness, constipation, heartburn, and belching. Exacerbations of pathology occur in the spring and autumn seasons. In children older than 10 years, the symptoms of duodenitis are similar to those in adults.
Treatment must be comprehensive. When the cause of the disease becomes infection with parasites, you need to take drugs from helminths.
Treatment of duodenitis

To cope with the pathology, you need to solve the following tasks:
Stop the inflammatory response.
To prevent the transition of chronic inflammation to the acute phase.
To normalize the work of the duodenum 12.
Restore digestive function.
If the disease has an uncomplicated course, then the treatment is carried out on an outpatient basis. A person will need to eat right, observe the regime of rest and work, minimize stress, give up bad habits, do not take alcohol, stop smoking.
Hospitalization may be required in the following cases:
Acute course of the disease.
The likelihood of having a tumor in the body.
High risk of bleeding.
Severe health of the patient.
Therapy is carried out in such areas as:
Compliance with a diet.
Taking medicines.
Physiotherapy.
Treatment with mineral waters.
Diet

It is proper nutrition that plays a decisive role in the treatment of duodenitis. If a person does not follow a diet, then it will not be possible to cope with inflammation.
The acute course of the disease requires compliance with table 1a according to Pevzner. You can eat mucous decoctions from rice or oats, pureed soups, liquid cereals in a mixture of milk and water.
Basic principles of nutrition for patients with acute duodenitis:
Food should be warm, mashed, steamed.
You need to eat 6 times a day, but in small portions.
There should not be long breaks between approaches to the table.
You can’t overeat.
Sample menu for 1 day:
First breakfast. Buckwheat porridge on a mixture of water and milk with butter, a glass of milk.
Lunch. A glass of milk.
Dinner. Cereal soup with milk (composition: oatmeal, milk, butter, sugar, water), meat puree from boiled low-fat beef with butter and milk, compote with dried apples.
Afternoon snack. A glass of milk and a soft-boiled egg.
Dinner. Rice porridge with a mixture of milk and water, an egg in a bag, a glass of milk.
Before bedtime. A glass of milk.
As the inflammatory process subsides, the diet becomes more varied.
Indicative menu of patients depending on the form of duodenitis:
| Ulcerative duodenitis, table number 1 | Gastritopodobny duodenitis, chair #2 | Duodenitis on the background of pancreatitis or cholecystitis, table number 5 |
1 breakfast | Rice porridge with milk. Compote with sugar | Glass of milk and curd cheese | Vinaigrette and dried bread, tea with milk |
2 breakfast | Yogurt | baked pumpkin | carrot juice |
Dinner | Noodle soup, zrazy, beetroot salad, kissel and bread | Soup with vegetables, meatballs, mashed potatoes, compote with dried fruits | Vegetable soup with sour cream, boiled fish, mashed potatoes, compote with dried apricots |
Afternoon snack | Pear compote | Crackers, rowan broth | A glass of milk |
Dinner | milk noodles | Stewed pollock and vegetables | Cottage cheese casserole, tea with sugar |
2 dinner | A glass of milk | A glass of milk | kissel |
Products that are recommended to be eaten by patients with duodenitis:
Boiled low-fat meat, which is ground into a puree.
Sour-milk drinks and products, milk.
Baked and boiled vegetables without peel, vegetable puree.
Soft-boiled eggs or scrambled eggs.
Vegetable oil, butter.
The juice.
Dried bread.
Honey, mousse, jelly.
Foods that are forbidden to eat with duodenitis:
Raw vegetables and fruits.
Canned food and smoked meats.
Spicy dishes, spices, garlic and onions.
Fatty fish, meat, mushroom broths, meat broths.
Ice cream.
Gas drinks.
Alcohol.
Diet recommendations for patients with duodenitis:
Food should be taken in small portions, 6 times a day. You don’t have to wait until you feel hungry. This can lead to pain.
Dishes should not be hot or cold.
You need to process food in a gentle way, that is, boil, steam, grind.
It is forbidden to overeat and eat at night.
Taking medications
Like any other disease, duodenitis requires medication.
Category of medicines | How do they work | Drug names | How to use |
proton pump inhibitors | They do not allow hydrochloric acid to be produced in significant quantities, due to which the duodenum 12 will not be subject to inflammation | Emanera. Omeprazole, Ultop, Zulbeks. | 20 mg 1-2 times a day. The course of treatment is 7-10 days. |
Antibacterial drugs | They are prescribed in the case when the inflammation is provoked by Helicobacter pylori. | Doxycycline 100-200 mg | 2 times a day. The course of treatment is 7-10 days. |
Clarithromycin, Amoxicillin, Metronidazole | 2 times a day. The course of treatment is 7-14 days. | ||
H2-histamine blockers | Suppress the production of hydrogen chloride | Ranitidine | 2 times a day. The course of treatment is 30-45 days. |
Famotidine | 2 times a day | ||
Antacids | Neutralize hydrogen chloride, envelop the intestinal mucosa, anesthetize | Almagel, Maalox, Gastal | 3 times a day if heartburn bothers |
Prokinetics | Normalize intestinal peristalsis, promote the movement of food through the intestines | Itomed, Ganaton | 1 tablet 3 times a day |
enzymes | Contribute to the normalization of the processes of digestion of food | Pancreatin, Creon | After every meal |
Antispasmodics | Reduce pain | No-shpa, Drotaverin, Platyphyllin | 1 tablet 3 times a day |
Sedative drugs | Relieve nervous tension | Valerian, motherwort | Within 10-14 days |
The drug De-nol is prescribed to patients with duodenitis to provide an antibacterial, anti-inflammatory and antacid effect. It protects the intestinal mucosa and promotes its regeneration. Adults are indicated to take 1 tablet 4 times a day, after each main meal and at bedtime. The drug should be taken with water. During the period of treatment, you should refrain from consuming milk, as the effectiveness of therapy will be reduced. Children under 12 years of age are prescribed 1 tablet 2 times a day. The duration of therapy is 1,5 months.
The rest of the medicines the doctor combines at his own discretion. Treatment with antibiotics is required to get rid of Helicobacter pylori. When stressed, sedatives should be taken. If the patient is diagnosed with hyperacidity of the stomach, antacids, histamine blockers and proton pump inhibitors should be used.
Physiotherapy treatment. Patients with duodenitis are shown to undergo ultrasound treatment, phonophoresis, magnetic therapy.
Treatment with mineral waters. Patients with duodenitis are shown to use non-carbonated mineral waters: Borjomi, Essentuki No. 4, Smirnovskaya No. 1, Slavyanovskaya, Berezovskaya. The water must be warm. Drink it one hour after eating.
An integrated approach to treatment allows you to get rid of the disease and achieve a full recovery.









