Contents
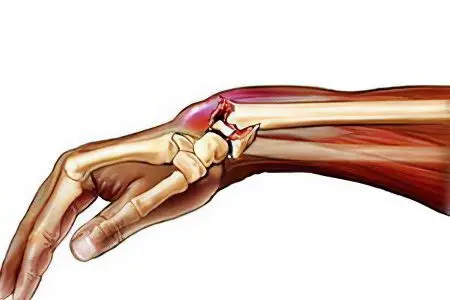
The human hand has a very complex anatomical structure, thanks to which it is able to perform various movements. In childhood, the joint capsule and ligaments are very elastic, so dislocation can occur quite rarely. The older a person becomes, the rougher his ligaments become, which can no longer fully fulfill their functions.
The risk group for dislocation of the wrist includes people who are engaged in active sports that are accompanied by frequent falls (football, volleyball, basketball, pole vaulting, etc.). According to existing statistics, the likelihood of a dislocation for pedestrians increases with the advent of the winter season. During the sleet, the number of victims increases sharply, who, when falling, get dislocations of the upper limbs.
Classification of dislocations
Dislocations of the upper limbs are classified as follows:
By origin: Dislocations of the hands are:
acute traumatic;
habitual traumatic;
congenital
pathological.
By volume: Dislocations of the upper limbs are:
full;
partial.
By location: Dislocations of the hands are:
shoulder dislocation;
dislocation of the elbow joint;
dislocation of the forearm;
dislocation of the hand;
dislocation of the finger.
By type of damage: Dislocations of the upper limbs are:
open;
closed.
By duration: Dislocations of the hands are:
fresh (no more than 3 days have passed since the injury);
stale (3 to 4 weeks have passed since the injury of the upper limb);
chronic (more than 30 days have passed since the dislocation was received).
Types of dislocations of the hand

Modern medicine has identified a large number of types of dislocations of the hand of the upper limb:
perelunary;
true;
transnavicular-perilunary;
transnavicular-translunate;
peritrihedral-lunar;
perinavicular-lunar;
dislocation of fingers, etc.
Causes and symptoms of a dislocated arm
The main causes of dislocation of the hand include the following:
a fall;
lifting weights;
swipe;
amateur massage, etc.
Sometimes dislocations (pathological) can occur against the background of the progression of various diseases:
arthrosis;
bone tuberculosis;
arthropathy (of various origins);
arthritis and other diseases in which there is a change in the joint capsule.
With a dislocation of the arm, regardless of the location of the injury, a person experiences severe pain. He may completely or partially lose the mobility of his arm. Almost immediately after the injury, edema forms in the area of the injured joint. Some patients lose sensation in the lower part of the limb (this is due to the fact that during the dislocation the median nerve was compressed). When probing the pulse of the victims, both rapid and slow rhythm can be noted. Another indicator of dislocation of the hand is the “symptom of springy fixation.” Confirming the presence of this symptom is quite simple by making a passive movement of the lower part of the hand.
Most often, dislocation occurs in the shoulder joint of the upper extremities. If this joint is injured, the risk of damage to the nerves and arteries increases, so patients with such a dislocation must be urgently taken to the hospital.
In this category of patients, the following symptoms may appear:
severe pain;
bruising;
puffiness;
impaired motor function in the injured upper limb, etc.
First aid for the victim

Each person should be able to help a patient who has a dislocated arm. The first thing to do is to apply a cold compress to the site of injury to the upper limb (it can be a heating pad with ice or cold water) and give an analgesic drug from the class of analgesics.
You can’t set your hand on your own, as you can cause even more harm to the patient. It is advisable to fix the injured hand of a person in a forced position. To do this, you can use any means at hand (a board, rags, etc.). In this position, the victim should be taken to the nearest medical facility.
Diagnostics
A patient who has received a hand injury must be urgently taken to a medical facility, where specialists will diagnose and provide emergency care. The doctor of the traumatic point will carefully examine the injured hand, palpate, and interview the patient. During probing the damaged area, the specialist determines not only the sensitivity of the skin, but also the motor function of the upper limb. Careful palpation will reveal any abnormalities in the neurovascular bundle, as well as check the rhythm in which the artery pulsates.
After a personal examination, the patient will be sent for x-rays, thanks to which it will be possible to determine whether, in addition to dislocation, there are any other injuries (fracture, bone fracture, etc.) of the upper limb. Usually, an x-ray is taken in two or three projections, and its results are stored in a medical institution (they must be issued to patients on demand).
If during the diagnostic measures serious injuries of the limbs were detected, the patient is sent to the surgical department, where he will undergo an emergency operation. Sometimes there are cases when patients were diagnosed with dislocation of the same joint more than 3 times. This category of patients needs surgical treatment, after which they will be assigned a disability group. The male half of the population with such a diagnosis will automatically be exempted from the obligation to serve in the Army.
When diagnosing a traumatic dislocation, a specialist during palpation determines how much the shape of the joint has changed. It is equally important to identify whether retraction has occurred at the locations of the articular endings. During palpation, the traumatologist may feel springy resistance in the damaged area.
In traumatic dislocation of the upper limbs, patients may have:
tear or complete rupture of tendons;
extensive rupture of the capsule;
nerve compression;
rupture of blood vessels, etc.
Hand dislocation treatment

Since a dislocation, like any other injury, is accompanied by a strong pain syndrome, the patient’s treatment begins with his anesthesia (in case of severe injuries, general anesthesia is done). In most cases, this category of patients is prescribed potent painkillers, since after the pain syndrome is relieved, the dislocated segments of the upper limbs are reduced to patients. After complete relaxation of the muscles, the traumatologist proceeds to the reduction procedure, which is carried out very carefully, without sharp and rough movements. The reduced limb is fixed in the correct position by means of a plaster cast, which must be worn for a certain time (for several weeks).
As soon as the plaster bandage has been removed, the patient needs to undergo a rehabilitation course that will help restore the mobility and functionality of the arm.
For these purposes can be assigned:
physiotherapeutic procedures;
physiotherapy;
hydrotherapy;
magnetotherapy;
massage;
mud treatment;
mechanotherapy, etc.
Each of the rehabilitation methods is aimed at normalizing blood circulation in the injured limb, relieving pain, etc. Thanks to a properly selected physiotherapy complex, patients can quickly increase the elasticity of muscle tissues.
Some patients, self-medicating, lose precious time for non-surgical reduction of dislocation of the joints of the upper extremities. Often they arrive at a medical facility several weeks after the injury.
In such a situation, specialists are forced to carry out treatment in several stages:
First of all, a distraction apparatus is applied to the patient, the functions of which are to stretch the wrist joint.
After the wrist joint has been stretched, surgeons perform an open reduction of the dislocation and remove the distraction apparatus. This procedure can be delayed for 8-10 days, depending on the complexity of the dislocation.
The damaged wrist joint is fixed with Kirschner wires.
After the operation, this category of patients will have to undergo physiotherapy.
During the surgical treatment of chronic dislocation, in which deforming arthrosis has developed, specialists perform arthrodesis of the wrist joint. Patients who have undergone such an operation need a long course of rehabilitation therapy.
Hand dislocation reduction

To correct a dislocation of the upper limb, a specialist may need the help of one or two employees of a medical institution.
When choosing a technique according to which the shoulder joint will be reduced, traumatologists prefer:
the Hippocratic method;
the Kocher method;
Mota-Mukhina method.
When reducing the dislocation of the hand, it is necessary to achieve a certain angle of flexion in the elbow joint – 90 ° C. One assistant should firmly fix the shoulder joint, and keep it in this position throughout the procedure. At this time, the surgeon stretches the joint of the hand of the upper limb along the axis of the forearm. When the hand is set, the thrust is carried out with one hand for 1 finger, and with the other hand for the remaining fingers. Once the stretching of the joint has been completed, the surgeon applies physical pressure to the hand. Press on the joint until the dislocation of the protruding part of the hand is completely eliminated.
After elimination of the dorsal dislocation of the hand of the upper limb, the doctor must fix the hand at a certain angle of flexion (40 ° C), and apply a plaster cast. In order to make sure that the chosen treatment technique is correct, the patient is sent for a second x-ray.
In the event that the hand joint is unstable, the specialist may choose another treatment method, in which fixation is carried out using Kirschner wires. Each pin is inserted at an angle and passes through the distal end of the outer surface of the radius. The pins also pass through the fifth metacarpal and the carpal joint.
Currently, many specialists carry out the reduction of dislocations with the use of distraction devices.
This technique is shown in the following cases:
if the surgeon cannot set the dislocation with his hands;
if the patient has no symptoms indicating that compression of the anatomical formations has occurred in the articular canal of the wrist;
if the patient sought medical help a week (or more) after receiving a dislocation.
Surgical reduction of dislocations of the upper extremities is indicated in the case when the patient had compression of the nerve node in the articular canal of the wrist. Late medical attention, in this case, can lead to nerve degeneration and loss of mobility of the lower arm.
During surgery, the surgeon makes an arcuate incision on the skin of the injured hand, through which it will be possible to get to the wrist joint. If necessary (this is decided by the specialist during the operation), another incision is made that dissects the capsule of the hand joint. After that, distraction is carried out (along the axis of the forearm), in parallel with which the surgeon removes damaged tissues and reduces the dislocation.
Sometimes, during a surgical operation, there is a need for additional fixation of the wrist joint. For these purposes, surgeons use Kirschner wires, which must be present in the patient’s joint for at least 4 weeks (in difficult cases, the wires can fix the joint for 4 months). Their removal occurs after examination of the damaged joint and control radiography.









