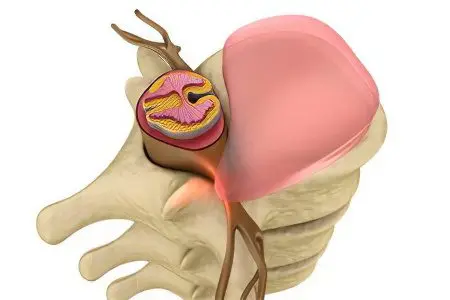
Disc prolapse is a displacement of the intervertebral disc by a distance not exceeding 2-3 mm. Disc prolapse is the initial stage in the formation of an intervertebral hernia. Further displacement of the disc, which exceeds 4 mm or more, is already called protrusion.
Although a prolapsed disc is not a reason for hospitalization, it is impossible to leave a section of the spinal column in this state, since in the future the disc will move more. Therefore, disc prolapse requires immediate treatment.
Considering the term “disc prolapse”, different authors give different characteristics to this condition. So, Russian scientists, including Golovatenko-Abramov K.V., and Magometov M.K., designate prolapse as a bulging of the intervertebral disc beyond the vertebrae against the background of stretching of the fibrous ring. However, the rupture of the ring does not occur. The authors consider prolapse and protrusion as identical conditions. They consider these terms to be used as synonyms.
Japanese scientists, among them: Maeda M., Takashi I., Tarou K. and others, generally do not single out such a thing as disc prolapse. They propose to consider the stages of hernia formation from the moment of the onset of protrusion of the disc with or without rupture of the fibrous ring (without the hernia going beyond the boundaries of the fibrous ring). In this case, this condition is defined as disc protrusion.
Swedish scientists (Stromqvist B., Jonsson B. et al.) consider disc prolapse as any dislocation of the nucleus pulposus to the posterior longitudinal ligament in the absence of rupture of the fibrous ring, or with its rupture. At the same time, they call protrusion such a protrusion in which the rupture of the fibrous ring does not occur, or it is minimal.
To end the disputes around these terms, the team of authors of the Department of Neurology of the RMA of Postgraduate Education (Professor V.N. Shtok, Professor O.S. Levin, etc.) proposed any protrusion of the disc edge beyond the line of adjacent vertebrae, which exceeds 2-3 mm called a herniated disc. Thus, prolapse can be considered as the initial stage of hernia formation without rupture of the fibrous ring.
Causes of a prolapsed disc

The main reason for the formation of spinal disc prolapse is osteochondrosis. With this disease, degenerative-dystrophic changes occur in the spinal column, the disc loses moisture and ceases to be elastic. Gradually, the size of the disc decreases, which leads to increased pressure on the vertebrae. As a result, the disc is injured, as the spine is constantly under physical stress. Parts of the disc begin to protrude beyond the vertebrae, forming a prolapse. In the future, a person develops an intervertebral hernia.
The average age a person is diagnosed with a hernia is between 30 and 50 years of age. However, prolapse may begin to develop earlier, due to the early manifestation of osteochondrosis.
The reasons are:
Anomalies in the development of the spinal column.
Diseases of a dysmetabolic nature (hyperthyroidism, diabetes mellitus).
Injuries of the spinal column, transferred at an early age.
Skeletal anomalies, such as hip dysplasia.
Risk factors that contribute to the formation of disc prolapse include:
Weight lifting;
Bruises of the spine;
Frequent vibrations;
Sudden movements, for example, during sports;
Prolonged sitting (at risk are people working at a computer, motorists, etc.).
Excess body weight;
Kyphosis, lordosis and other types of curvature of the spine;
Posture disorders;
Prolonged pastime in an uncomfortable position for a person.
If you do not start to control the prolapse of the spinal disc at the initial stages, then in the future a full-fledged hernia will form in a person. In turn, this is a serious disease, which often significantly worsens the quality of life of the patient and requires surgical intervention.
Disc prolapse symptoms

Most often, the patient does not feel symptoms of disc prolapse, since the initial stages of hernia development have a latent course.
Although, depending on the individual characteristics of the body, a person may present the following complaints:
Periodically arising pains in that department of a backbone where there is an infringement.
The pains are dull in nature, not always present. It is possible to increase pain during static and dynamic loading. During the adoption of a horizontal position of the body, the pain completely disappears.
A person seeks to protect the painful area from loads and excessive stress, limiting movement in it.
In the area where the disc has shifted, muscle tension occurs.
As the hernia progresses, the pain intensifies, the mobility of the affected area is increasingly limited. In the future, complications of the disease develop, including: radicular syndrome, discogenic myelopathy, vertebral artery syndrome. Often, disc prolapse, like a disc herniation, does not betray itself in any way until the stage of exacerbation sets in.
Distinguish disc prolapse of the cervical, thoracic and lumbar spine. Depending on this, the symptoms of the disease differ, namely, the location of the pain.
Treatment of prolapsed disc

Treatment of disc prolapse should begin as soon as it is discovered. Therapy is carried out on an outpatient basis and is reduced to drug correction. Spinal disc prolapse can and should be monitored in conjunction with the attending physician.
Therapy must be comprehensive. The patient is prescribed drugs to reduce pain. Preference is given to drugs from the NSAID group: Ibuprofen, Diclofenac, Ketoprofen, Naproxen, etc.
To reduce muscle tension and relieve increased tone from the back muscles, it is necessary to use muscle relaxant drugs, for example, Tolperisone hydrochloride. In parallel, the patient is prescribed vitamin-mineral complexes with an emphasis on vitamins of group B. Specialists often treat the early stages of spinal hernia with the help of chondroprotectors, including: Teraflex, Chondroitin sulfate, Chondroxide, etc. Oral administration of drugs in the form of tablets and their local application in ointment form.
Equally important is the passage of physiotherapy techniques, which at the initial stage of the development of the disease allow to achieve the maximum effect. Traction therapy will help restore the disc, due to which there is an increase in the distance between the vertebrae, which leads to a decrease in the load on the disc. It is possible to supplement the treatment with manual therapy methods, however, it should only be carried out by an experienced doctor.
It is important to remember about the complexes of physiotherapy exercises. Thanks to well-chosen exercises, it is possible to stretch the spine, strengthen the muscle frame, and improve the blood supply to the affected disc. However, in order to achieve the desired effect, it is necessary to exercise on a regular basis.
Thus, disc prolapse is a condition that requires treatment. With competent and timely correction, it is possible to achieve significant results. As a rule, after a month from the start of treatment, the patient notices an improvement in his condition. The apogee of therapy is a decrease in disc prolapse in size due to resorption processes, which means preventing the formation of an intervertebral hernia.









