Contents
DIC syndrome – This is a disorder of the process of hemostasis, which contributes to the formation of blood clots, as well as the development of various hemorrhagic and microcirculatory disorders. The full name of the disease is disseminated intravascular coagulation, you can also find such a designation of the syndrome as thrombohemorrhagic syndrome.
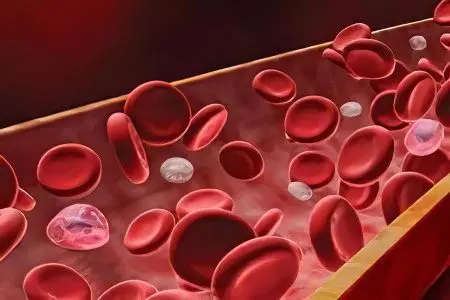
DIC is characterized by hemorrhagic diathesis with increased coagulation of blood inside the vessels, which leads to the formation of blood clots that stop them. This, in turn, entails the development of pathological changes in the organs of a dystrophic-necrotic and hypoxic nature.
DIC-syndrome poses a threat to the life of the patient, as there is a risk of bleeding. They are large and hard to stop. Also, internal organs may be involved in the pathological process, the functioning of which will be completely disrupted. The kidneys, liver, spleen, lungs and adrenal glands are primarily at risk.
The syndrome can occur with a variety of pathologies, but it always leads to thickening of the blood, disruption of its circulation through the capillaries, and this process is not compatible with the normal functioning of the human body.
DIC can lead to both lightning-fast death of the patient and protracted latent fatal forms of disorders.
The statistics of DIC syndrome cannot be calculated, since the syndrome occurs with different frequencies in different diseases. Some pathologies are always accompanied by DIC, while in other diseases it is somewhat less common. This syndrome can be regarded as an abnormal protective reaction of the body, which it gives out in order to suppress the bleeding that occurs when the vessels are damaged. Thus, the body seeks to protect itself from the affected tissues. Thrombohemorrhagic syndrome is often found in the practice of doctors of various specialties. Gynecologists, surgeons, resuscitators, traumatologists, hematologists, etc. are familiar with him.
Causes of DIC
The causes of DIC are various diseases that are accompanied by damage to tissues, blood vessels and blood cells. In this case, hemostasis fails in the body with an increase in blood clotting.
The following pathological processes can lead to the development of thrombohemorrhagic syndrome:
Any shock state of the body. Shock can occur due to an injury, against the background of a burn. Perhaps the development of hemorrhagic, anaphylactic, septic, cardiogenic shock. The longer the shock, the stronger it is, the brighter the DIC will be. (read also: Anaphylactic shock – causes, symptoms and treatment)
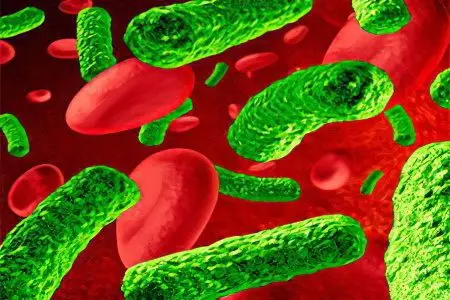
Septic conditions that are a complication of a viral or bacterial infection. Septic shock always provokes the development of this syndrome.
generalized infections. In this case, most often the syndrome occurs in newborns.
Obstetric pathologies – severe preeclampsia, placental abruption or placenta previa, fetal death inside the mother’s womb, manual separation of the placenta, uterine bleeding, cesarean section, anatomical fluid embolism.
Surgical interventions, accompanied by an increased risk of trauma to the patient. Most often, these are operations that are performed to remove malignant neoplasms, interventions performed on organs that mainly consist of parenchyma, and operations on blood vessels. If at the same time the patient requires a massive blood transfusion, or he develops a collapse or bleeding, then the risk of developing thrombohemorrhagic syndrome increases.
Any terminal states of the human body lead to the development of DIC of varying degrees of severity.
With a 100% probability, DIC will develop in people against the background of intravascular hemolysis. The destruction of blood cells most often occurs when a person is transfused with blood of a different type (incompatible transfusion).
Risk factors for the development of DIC are surgical procedures such as organ transplantation, implantation of a prosthetic valve of the heart or blood vessels, the need for artificial start of blood circulation.
Taking certain medications increases the risk of developing the syndrome. These are diuretics, oral contraceptives, drugs from the group of fibrinolysis inhibitors and Ristomycin (an antibacterial drug).
Giant angiomas with their multiple appearance.
The bites of poisonous snakes and other acute poisonings of the human body are capable of provoking the development of DIC.
In some cases, allergic reactions become the cause of the development of a dangerous condition.
Immune diseases such as: rheumatoid arthritis, glomerulonephritis, systemic lupus erythematosus, etc.
Vascular pathologies, including congenital heart defects, myocardial infarction, heart failure, etc.
However, the main cause of the development of DIC is sepsis (virological and bacteriological) and shock of any etiology. These pathologies account for up to 40% of cases of all registered DIC syndromes. If we are talking about newborn children, then this figure rises to 70%. But instead of the term DIC, doctors use the designation “malignant purpura of newborns.”
What happens in DIC?
With DIC, there is a failure of the complex of body reactions that are triggered in order to prevent bleeding. This process is called hemostasis. At the same time, the function responsible for blood clotting is excessively stimulated, and the anticoagulant (anticoagulant) and fibrinolytic systems that balance it, on the contrary, are quickly depleted.
Enzymes produced by bacteria that have entered the body, toxins, immune complexes, amniotic fluid, phospholipids, low cardiac effusion into the bloodstream, acidosis and other pathogenic factors for the body can affect the manifestation of DIC. At the same time, they will circulate either in the bloodstream or act on the vascular endothelium through mediators.
DIC always develops according to certain patterns and goes through several successive stages:
At the first stage the process of excessive blood clotting is started, as well as cell aggregation inside the vessels. An excess amount of thromboplastin, or a substance with a similar effect, is released into the blood. This starts the folding processes. The time of the initial stage can vary widely and take from a minute to several hours if the syndrome develops acutely. From several days to several months, the pathological process will proceed if the syndrome has a chronic form.
The second stage characterized by the start of the process of consumption coagulopathy. At the same time, the lack of fibrogen, platelets and other plasma factors responsible for the process of blood clotting increases in the body.
The third stage is critical. At this time, secondary fibrinolysis occurs, blood coagulation reaches a maximum, up to a complete stop of this process. In this case, hemostasis is largely unbalanced.
recovery stage characterized by normalization of hemostasis. Residual dystrophic-necrotic changes are observed on organs and tissues. Another culmination of DIC can be an acute failure of one or another organ.
The full development of DIC (its severity and mechanism of development) depends on the degree of disturbance of blood microcirculation and on the degree of damage to organs or their systems.
Symptoms of DIC
Symptoms of DIC will be determined by the clinical manifestations of the disorder that provoked its development. They also depend on how quickly the pathological process develops, the state of the mechanisms responsible for the compensation of hemostasis, and what stage of DIC the patient is in.
Symptoms of acute DIC.
In the acute form of DIC, the pathological process quickly spreads throughout the body. Most often this happens within a few hours.
A person is in a state of shock, his blood pressure drops to the border of 100/60 and below.
The patient loses consciousness, symptoms of acute respiratory failure and pulmonary edema are observed.
Bleeding intensifies, profuse and massive bleeding develops. This process involves such systems and organs of the human body as: the uterus, lungs, organs of the gastrointestinal tract. Possible development of bleeding from the nose.
Against the background of acute DIC, there is a destructive destruction of pancreatic tissues with the development of functional insufficiency of the organ. Perhaps the accession of gastroenteritis of an erosive-ulcerative nature.
In the myocardium, there are foci of ischemic dystrophy.
With amniotic fluid embolism, DIC develops at lightning speed. In a few minutes, the pathology goes through all three stages, making the condition of the woman in labor and the fetus critical. Patients undergo hemorrhagic and cardiopulmonary shock, which can hardly be stopped. In this regard, the prognosis for life is unfavorable and death occurs in 80% of cases.
Symptoms of subacute DIC
The course of the syndrome in this case is more favorable.
The hemosyndrome is expressed in the occurrence of rashes of the hemorrhagic type.
Bruising and large hematomas may appear on the skin.
Injured areas, injection sites are characterized by increased bleeding.
Mucous membranes are also prone to bleeding. Blood impurities may be present in sweat and tears.
The skin is characterized by excessive pallor, up to marbling. When touched, the skin feels unnaturally cold.
The internal organs swell, fill with blood, necrotic areas, hemorrhages appear on them. The organs of the gastrointestinal tract, liver and kidneys, as well as the adrenal glands and lungs are subject to pathological changes.
As for the chronic form of DIC, it is not only more common than others, but in most cases it is hidden. The patient, due to the absence of symptoms, may not even be aware of the development of pathologies in the hemostasis system. However, as the disease that caused DIC progresses, its symptoms will become more pronounced.
Other symptoms
Other symptoms that may indicate the development of chronic DIC include:
Deterioration and lengthening of the regeneration process of any wounds.
The growth of asthenic syndrome with the corresponding symptom complex.
Accession of a secondary purulent infection.
The formation of scars on the skin in those places where there were injuries.
Complications of DIC

Complications of DIC, as a rule, are very severe and threaten not only the health, but also the life of the patient.
More often than not, the following conditions develop:
Hemocoagulation shock. Organs and tissues begin to experience oxygen deficiency, as blood microcirculation is disturbed in small vessels responsible for their nutrition. In addition, the amount of toxins in the blood itself increases. As a result, the patient’s pressure drops sharply, both arterial and venous, organ failure, shock, etc.
Acute respiratory failure. It is a borderline condition that poses a direct threat to the life of the patient. As hypoxia intensifies, loss of consciousness occurs, convulsions develop and hypoxic coma occurs.
Acute renal failure is another most common complication of DIC. The patient stops urinating, up to the complete absence of urine output. The water-salt balance is disturbed, the level of urea, nitrogen, and creatinine increases in the blood. This condition is potentially reversible.
Liver necrosis.
From the digestive tract: stomach ulcer, intestinal infarction, pancronecrosis.
From the side of the cardiovascular system – ischemic stroke.
On the part of the hematopoietic system – hemorrhagic anemia in acute form.
Diagnosis of DIC
Diagnosis of DIC is built on examining the patient, taking an anamnesis and conducting laboratory tests.
The patient is required to take the following tests:
UAC;
OAM;
blood smear;
Blood on a coagulogram, as the main method for diagnosing hemostasis (platelets, fibrogens and other important indicators are counted);
ELISA (determination of PDF, RFMK, D-dimer as the main markers of blood coagulation inside the vessels):
Blood for paracoagulation tests (allow to confirm or refute the diagnosis).
The doctor finds out the cause that led to the development of DIC, determines its stage and nature.
If the course of the syndrome is hidden, then hypercoagulability can be determined solely according to laboratory tests. In this case, fragmented erythrocytes will be present in the blood smear, thrombosed time and APTT will increase, and the concentration of PDP will increase. A blood test will indicate a lack of fibrinogen and platelets in it.
If the syndrome is confirmed, then the most vulnerable organs are examined without fail: kidneys, liver, heart, brain, lungs, adrenal glands.
Treatment of DIC

Treatment of DIC is a rather complicated process; the patient’s recovery does not occur in every case. If an acute form of the syndrome is diagnosed, then death occurs in 30% of cases, which is a fairly high rate. However, it is not always possible to accurately establish the reason why the patient died. Whether DIC became a critical condition, or the patient died as a result of the negative impact of the underlying disease.
Doctors observing DIC, first of all, make efforts to eliminate or minimize the factor that led to the development of the syndrome and stimulates its progression. It is important to eliminate purulent-septic conditions, which most often provoke a violation of hemostasis. At the same time, it makes no sense to wait for the results of bacteriological studies; therapy is carried out in accordance with the clinical signs of the disease.
Antibacterial therapy against the background of DIC is indicated in the following cases:
Postponed abortion;
Premature discharge of amniotic fluid, especially when they are not transparent and contain turbidity;
An increase in body temperature;
Symptoms indicating inflammation of the lungs, urinary tract, abdominal organs;
Signs of meningitis.
For treatment, broad-spectrum antibacterial drugs are used, with the inclusion of y-globulins in the treatment regimen.
For the relief of shock conditions, injections of saline solutions, plasma transfusions with Heparin, Prednisolone (intravenously), Reopoliglyukin are used. If the shock syndrome is eliminated in a timely manner, it is possible to stop the development of DIC, or significantly mitigate its manifestations.
As for Heparin, when it is administered, there is a risk of bleeding. It does not have a positive effect in case of its belated use. It should be administered as early as possible, strictly following the recommended dosage. If the patient is in the third stage of the development of DIC, then the introduction of Heparin is a direct contraindication. Signs indicating a ban on the use of this drug are: pressure drop, bleeding (it may be hidden), hemorrhagic collapse.
If the syndrome has just begun to develop, then the introduction of a-blockers is indicated: Dibenamine, Fentolamine, Thioproperazine, Mazheptil. The drugs are administered intravenously in the required concentration. They contribute to the normalization of microcirculation in the organs, resist the formation of blood clots inside the vessels. Epinephrine and noradrenaline preparations should not be used, as they can worsen the situation.
In the formation of renal and hepatic insufficiency, in the early stages of the development of DIC, it is also possible to use drugs such as Trental and Curantil. They are administered intravenously.
At the third stage of the development of DIC, the administration of protease inhibitor drugs is necessary. The drug of choice is Kontrykal, the method of administration is intravenous, the dose is not more than 100 IU at a time. If such a need arises, the infusion can be repeated.
Local effects are reduced to the treatment of bleeding erosions, wounds and other areas with the help of Androxon in a 6% concentration.
Summing up, it can be noted that the complex treatment of DIC is reduced to the following points:
Elimination of the root cause that provoked the development of the syndrome.
Carrying out antishock therapy.
Replenishment of blood volumes with transfusion of plasma enriched with Heparin, if there are no contraindications to this.
Early use of adrenergic blockers, and drugs that reduce the number of platelets in the blood: Curantil, Trental, Ticlodipine.
Introduction Contrykal, transfusion of platelets to normalize hematocrit against the background of severe bleeding.
Appointment of plasmacytapheresis, if there are indications for this.
To normalize microcirculation in the affected organs, nootropics, angioprotectors and other syndromic drugs are used.
With the development of acute renal failure, hemodiafiltration, hemodialysis are performed.
Patients with DIC are necessarily hospitalized and are under round-the-clock medical supervision. They are located either in the intensive care unit or in intensive care units.
As for the prognosis, it is very variable. To a greater extent, it depends on what caused the development of DIC, on the degree of hemostasis impairment, on how quickly first aid was provided and how adequate it was.
It is impossible to exclude a lethal outcome, since it can occur against the background of heavy blood loss, shock, and organ failure.
Doctors should pay special attention to patients belonging to risk groups – the elderly, pregnant women, newborns, people with underlying diseases.









