Contents
DIC (disseminated intravascular coagulation syndrome) is a disorder in the functioning of the hemostasis system, which is manifested primarily by increased formation of blood clots in small vessels.
This pathology is relevant for various fields of medicine. Obstetricians, resuscitators, and surgeons are engaged in the diagnosis and treatment of DIC. Pathology occurs both in adults and in children, including newborns. Often, coagulopathy (disturbances in the process of blood clotting) are congenital in nature, but can develop throughout life. DIC in newborns is a form of coagulopathy.
The mechanism of development of the disorder is quite complex, pathology can have many symptoms. For this reason, doctors face certain difficulties in making a diagnosis. DIC tends to aggravate the course of other diseases, but it is not an independent disease.
Thrombosis: when is the norm, and when is it a deviation?
Throughout life, a person receives various injuries, ranging from minor scratches to serious injuries. The body has its own defense mechanism to stop the bleeding. To do this, in the damaged area, it begins to curl up, forming a blood clot.
In general, the body has two systems that have a cardinally opposite purpose. One system is called coagulation, and the second is called anti-coagulation. If they work without any disturbance, then the balance is maintained in the body. When a threatening situation arises, for example, in case of injury, the blood coagulates, preventing massive bleeding. In the absence of any damage, the blood is in a liquid state.
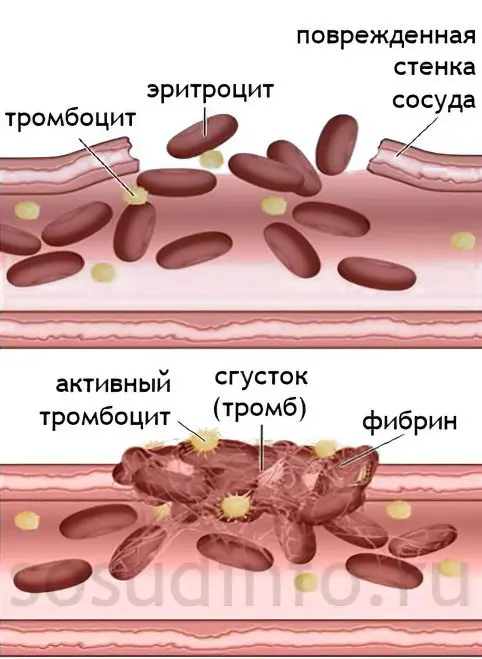
In order for a blood clot to form at the site of damage to the vessel, the body must trigger many complex reactions. They involve a protein called fibrinogen, which is present in the blood plasma, as well as platelets, a clotting factor, and various enzymes. As a result, the resulting clot closes the defect on the vascular wall and prevents blood from pouring out.
If there is no damage to the vessel, then the blood circulates through the vessels in a liquid state, preventing blood clots from forming. Antithrombotic mechanisms are responsible for this, which are carried out thanks to substances called anticoagulants. They include plasma proteins, endogenous heparin, and proteolytic enzymes. If fibrinogen begins to accumulate in one place or another of the vessel, then the fast blood flow “breaks” it and a blood clot does not form. This mechanism is called fibrinolysis. It also involves enzymes that produce white blood cells, platelets and other blood cells. Small particles of fibrin in the future will simply be destroyed by macrophages and leukocytes.
If there is a failure in certain systems of hemostasis, or a person develops any disease, the mechanisms that regulate the work of the coagulation and anticoagulation systems fail. At the same time, blood clots begin to form in the body, and the risk of massive bleeding increases. It is these disorders that underlie the development of DIC. They are extremely dangerous to human health and carry a threat to life.
DIC – what are the causes?

DIC is not a disease, but a consequence of certain disorders in the body.
Therefore, its development is influenced by a number of conditions:
Infectious diseases accompanied by sepsis, or a severe course of a viral or bacterial infection.
Shock of any etiology: against the background of an injury, against the background of poisoning of the body, against the background of an infection.
A condition bordering on a fatal outcome is clinical death.
Operations for organ transplantation, for the installation of a prosthetic heart valve. Serious injury.
The presence of a person on a ventilator during the operation.
Cancer lesions of internal organs. In terms of the development of DIC, leukemia is of particular danger.
In obstetric practice, DIC develops against the background of massive bleeding during childbirth, with early placental abruption, with amniotic fluid embolism.
During pregnancy, DIC can be accompanied by severe toxicosis, Rh conflict, ectopic pregnancy, and more.
Diseases of the cardiovascular system.
Inflammation of the internal organs, accompanied by suppuration.
DIC can develop during clinical death, during resuscitation. Against the background of terminal states, DIC either develops or will develop in the near future if certain therapeutic measures are not taken.
In a healthy newborn baby who appeared on time, DIC is very rarely diagnosed. It can be accompanied by severe neonatal hypoxia, respiratory disorders, amniotic fluid embolism. In the latter case, the symptoms of DIC will be diagnosed in both the woman and the child.
Hereditary coagulopathy includes hemophilia and von Willebrand disease. In this case, the child has increased bleeding. Thrombohemorrhagic syndrome in children is diagnosed very rarely. Infectious diseases and severe injuries can provoke it.
DIC syndrome: stages and forms
Depending on the mechanism that provoked the development of DIC, the following stages are distinguished:
Stage of hypercoagulability. At the same time, the concentration of thromboplastin in the blood increases, which contributes to its increased coagulability. As a result, blood clots begin to form in a person.
Consumption coagulopathy. The level of clotting factors in the blood rises, in response to this, the body increases fibrinolytic activity in order to prevent blockage of blood vessels by blood clots.
Hypocoagulation. During this period, there is a shortage of platelets in the body, as the body has used up their reserves during the previous stages. This situation leads to the fact that the blood does not clot well.
Recovery stage. So, any serious injury or bleeding, or other damaging factor, entails an increased and uncontrolled consumption of platelets and other blood components responsible for its coagulation. This causes their deficiency and further hypocoagulation with increased bleeding. Provided that during this period the patient will be provided with high-quality medical care, he will have a recovery phase.
The severity of the lesion is due to the fact that blood clots form in all small vessels, which entails the defeat of most tissues of organs and systems.

Depending on the nature of the symptoms of DIC and the severity of their course, the following forms are distinguished:
Sharp form. The duration of DIC in acute form can be from several hours to several days. Most often, this violation accompanies injuries, sepsis, surgical interventions, blood transfusion with massive blood loss.
Subacute form. The duration of this form of DIC can be several weeks. It most often accompanies chronic diseases of infectious origin and autoimmune processes.
Chronic form. This form of DIC can last for several years. Most often, it is diagnosed by therapists who observe patients with diseases of the liver, kidneys, heart, blood vessels, as well as diabetes. As the underlying disease progresses, the symptoms of DIC will increase.
relapsing form.
hidden form.
Sometimes DIC can develop within minutes. This form of pathology is called fulminant. Most often, obstetricians encounter this variant of DIC.
Symptoms of DIC
If DIC has a subacute or chronic course, then diagnosing it by symptoms can be very problematic. The acute phase, on the contrary, is accompanied by severe clinical manifestations, which are expressed in skin rashes and increased bleeding. In this case, it is not difficult to make a diagnosis.

Since, against the background of DIC, blood clots form in small vessels, organs such as the liver, lungs, skin and brain will suffer first of all. It is in them that the capillary network is more developed than in other organs. The prognosis for recovery depends on the severity of DIC.
The main symptoms that make it possible to suspect DIC include:
The appearance of a hemorrhagic rash on the skin. There may be foci of necrosis on the face, arms and legs.
Dyspnea. It occurs as a result of damage to the lungs. As respiratory failure increases, respiratory arrest with pulmonary edema is possible.
The accumulation of fibrin in the small vessels of the kidneys leads to malfunctions in their work, up to the development of renal failure. This is manifested by urinary retention and electrolyte imbalance in the body.
Neurological disorders are the result of brain damage.
Also, DIC is characterized by the appearance of nosebleeds, uterine bleeding, the appearance of hematomas in the area of soft tissues and internal organs.
If we consider the symptoms of DIC as a whole, then they come down to the appearance of thrombosis and hemorrhage, as well as disturbances in the work of most organs that are life-supporting.
Diagnosis of DIC

Diagnosis of DIC is impossible only on the basis of its clinical manifestations. Performing laboratory tests is a mandatory diagnostic measure. They make it possible not only to confirm the presence of DIC, but also to determine its stage and form.
The basic research method is a blood coagulogram, which makes it possible to detect a decrease in the number of platelets, an increase in fibrinogen (at the initial stage of the development of the pathology) or its fall (at the subsequent stages of the development of DIC). Also, a coagulogram will allow you to determine the increase in blood clotting time and other disorders.
If a person has died, then it is possible to conduct a post-mortem diagnosis of DIC. To do this, his tissue is sent for histological examination. They will detect blood cells that accumulate in the capillaries, as well as blood clots that clog them. The internal organs of a person are subject to multiple hemorrhages, covered with areas of necrosis.
If DIC is suspected, it is necessary to monitor blood counts, since in the initial stages of the development of the pathology they may be within the normal range. You also need to monitor electrolyte imbalances in the body, the level of urea and creatinine in the blood, diuresis and blood pH.
Treatment of DIC
There is simply no single regimen that could be used to treat any form of DIC. However, based on the stage of development of the pathological process, doctors have developed certain approaches to therapy.
First you need to establish the cause of DIC.
Depending on this, the following approaches can be implemented:
The appointment of antibiotics, if DIC develops against the background of purulent conditions.
Replenishment of blood with massive blood loss.
Stabilization of the work of the heart and blood vessels, blood pressure during the development of a shock state.
Provision of adequate obstetric care.
Conducting anesthesia in the development of shock on the background of trauma or other damage.
To eliminate the symptoms and manifestations of DIC, it is necessary to carry out the following therapy:
Treatment with anticoagulants. For this purpose, Heparin is most often used, which allows you to normalize the processes of blood coagulation, prevents blood clots from forming, and accelerates the process of their dissolution. As a result, the work of organs and tissues is normalized.
The appointment of fibrinolytics and antifibrinolytics, which depends on the stage of DIC. To make up for the lack of blood clotting factors, the patient is prescribed infusion therapy. For this, frozen plasma is used. It can be administered with Heparin, Gordox or Contrykal, which prevent hypercoagulation processes.
Improving blood flow, prescribing drugs to normalize blood microcirculation in the vessels. To achieve these goals, Aspirin, Trental, Curantyl and rheological solutions, for example, Voluven and Reopoliglyukin, are used.
Carrying out extracorporeal detoxification. In this case, the patient undergoes hemodialysis, plasmapheresis, cytopheresis.
Sometimes the decision to choose a therapeutic scheme has to be made very quickly, since there are only a few seconds to save a person’s life. It is imperative to take into account the stage of development of DIC, since at one time some drugs are indicated, and at another point in time they can be categorically contraindicated. In parallel, the state of the blood coagulation system, its electrolyte and acid-base balance should be monitored.
It is also impossible to allow a person to endure pain, anti-shock measures must be taken. At the first stage of the development of the pathological condition, Heparin is administered to the patient.
All patients who are at risk of developing thrombohemorrhagic syndrome, or who have already been diagnosed, are delivered to the intensive care unit. If this syndrome has reached stage 3, then the probability of death is 70%. The chronic course of thrombohemorrhagic syndrome always ends with the death of the patient.
In order to prevent the development of DIC, it is necessary to diagnose it in a timely manner and select therapy that is adequate to the situation. The sooner hemostasis is normalized, the faster the person will recover.
Video: lecture by A.I. Vorobyov about DIC:









