Contents

Hematologists suggest that fibrinogen is continuously converted to fibrin in the blood plasma. Since fibrin is the main component of blood clots, it would seem that this process should negatively affect the human body. However, this does not happen due to the coordinated work of the fibrinolytic and coagulation systems. The fact is that fibrin threads dissolve under the action of the anticoagulant system, participating in the process of fibrinolysis. To monitor the functioning of the hemocoagulation system in clinical laboratory diagnostics, a special marker, D-dimer, is used.
D-dimer are paired fibrinogen fragments that allow you to observe the process of its formation and dissolution.
D-dimer – what is it?
The use of D-dimer as a test for diagnosing the early stages of a thrombus has been practiced since the 90s of the last century. The method began to be used in practice as one of the main tests, allowing at an early stage to detect in the laboratory conditions that predispose to the formation of blood clots. Such a feature of the D-dimer as the appearance of protein compounds after the collapse of a blood clot was known 20 years before the use of this analysis in practice, but the discovery did not receive practical significance due to the little knowledge of the method.
If earlier the determination of D-dimer was available only to specialized clinics, then in modern medicine any medical institution that provides assistance in acute pathologies of hemostasis has the equipment to implement the technique. Emergency diagnostics, carried out at a high level, helps to start treatment in a timely manner and save the health and life of patients.
Reasons for the appearance of D-dimer
When hemostasis is activated, the process of fibrinolysis begins. Its main catalyst, plasmin, stimulates the breakdown of fibrin and fibrinogen. In addition to the predicted decay products, D- and E-fragments, by-products, dimers and trimers, are formed.
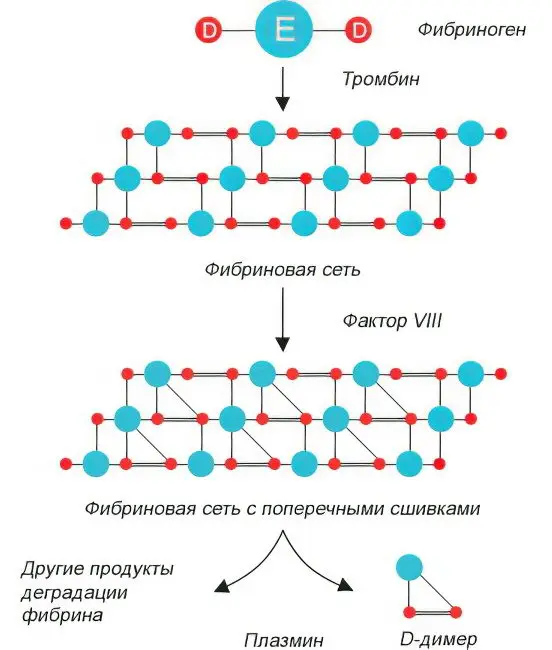
The appearance of D-dimers in the blood plasma indicates an excessively active fibrinolysis. An intensive splitting process indicates an increase in the blood clotting threshold and the accumulation of insoluble fibrin at previous stages. If during the study of blood plasma D-dimers are found in it, then there is an increased risk of thrombosis, immediate measures must be taken to correct hemostasis.
D-Dimer Norm, Consequences of Low and High

The study of the D-dimer index is a test of the activation of hemostasis at the highest level. The technique is quite complicated and is not included in a typical diagnostic kit.
The normal concentration of the marker in the blood plasma of a healthy person is up to 0,5 μg / ml (500 ng / ml), or it is not detected at all, has negative values.
Conditions in which the level of D-dimer in plasma increases:
Physiological changes during pregnancy;
Acute course of the inflammatory process;
Infectious lesion of any etiology;
oncological disease;
Consequences of thrombolytic therapy;
Diseases leading to damage to the liver parenchyma;
Thrombophilia during pregnancy or infertility;
Ischemia, myocardial infarction;
Hematomas of a large area, significant injuries;
Operational interventions;
Elderly age.
In 2% of cases, when the D-dimer values are significantly below the norm with the presence of signs of thrombosis, it is necessary to find out the reason for the paradoxical results.
Reasons for low values:
The minimum size of blood clots;
Long exposure of material for testing (more than 6 hours) in laboratory containers;
Delayed testing;
Deficiency of plasminogen or an excessively high concentration of an inhibitor of plasminogen activation.
Using the study of the level of D-dimers, it is possible to assess the degree of risk of developing thrombosis, DIC, to track the dynamics of therapy for hemostasis pathologies. Despite the accuracy and informativeness of the technique, it is not necessary to wait for its results to start anticoagulant treatment. Therapy is carried out based on the clinical picture of the disease, without wasting time.
The study of the level of D-dimers is carried out at an increased risk of developing cardiovascular diseases (ischemia), suspicion of pathological processes in the hemostasis system.
D-dimer during pregnancy
When conducting pregnancy, determining the level of fibrinogen in blood plasma is of great importance. The closer the due date, the higher these figures. It should be noted that an excessive increase in fibrinogen levels does not always fit into the norm, sometimes it is a sign of deep vein thrombosis.
Before childbirth and directly in the process of childbirth, it reaches its maximum level, after 3 days it intensively decreases, after 30-35 days it comes to standard values.
Table: D-dimer norm by day of pregnancy:
Gestational age | Normal D-dimer values by week of pregnancy in ng/ml | mkg FEU/ml |
Up to 13 weeks | Until 280 | Until 0,56 |
13 – 20 weeks | 100 – 700 | 0,2 – 1,4 |
21-28 weeks | 150 – 850 | 0,3 – 1,7 |
29 – 35 weeks | 150 – 1500 | 0,3 – 3,0 |
From 36 weeks to delivery | 200 – 1550 | 0,4 – 3,1 |
1 µg FEU/ml = 500 ng/ml
In accordance with the data in the table, it can be concluded that during pregnancy, the concentration of the marker increases with increasing gestational age. Deciphering its values will help prevent pathologies of pregnancy and childbirth, supplement the information obtained from the traditional analysis of the results of the coagulogram.
What if the D-dimer is up or down?

In the presence of a negative D-dimer test result, there is a high probability that the ability to form blood clots in such a person is minimal. However, even with this result, there remains a certain probability that thromboembolism may occur. Even the most sensitive test has an error of no more than 1% when the D-dimer is negative, but thrombosis is still present.
With positive results and a high D-dimer level, an in-depth diagnosis should be performed to detect deep vein thrombosis of the lower extremities or pulmonary artery. For this, ultrasound of the vessels and scintography are used. When interpreting test results, it is important to take age into account.
The result obtained is not always true due to conditions that cause an ambiguous hemostasis reaction, and this should also be taken into account.
Reasons for a high (false positive) value:
Inflammatory processes occurring in the body;
The presence of neoplasms;
Liver disease
Pregnancy;
Recent injuries and surgical interventions that mobilize the hemocoagulation system;
Increased rheumatoid factor.
Reasons for a low (negative) result:
There are anticoagulants in the blood that prevent the formation of blood clots, or dissolve existing blood clots, which completely distorts the results of the analysis;
The blood sample was taken incorrectly, after a short time after the formation of a blood clot or with a delay, in the first case, the hemocoagulation system did not have time to respond, in the second case, the blood sample was stored for too long.
A technical error can also give false results, for example, if the volume of blood taken does not match the volume of anticoagulant, although the percentage of such errors is extremely small. Modern analyzers and reagents for express tests are extremely sensitive, which allows timely detection of serious pathologies associated with thrombus formation.









