Contents
- Cutaneous staphylococcus – what is it?
- Cutaneous staphylococcus – how does it work?
- Cutaneous staphylococcus – who is at risk?
- Cutaneous staphylococcus – signs of infection
- Cutaneous staphylococcus – diseases
- Cutaneous staphylococcus – what diseases can it cause?
- Cutaneous staphylococcus in children
- Cutaneous staphylococcus – diagnosis
- Cutaneous staphylococcus – treatment
- Cutaneous staphylococcus – home remedies
- Cutaneous staphylococcus – prognosis
- Cutaneous staphylococcus – complications
Cutaneous staphylococcus, or Staphylococcus epidermidis, is a common symbiote bacteria found on the skin, oral mucosa and urogenital tract. Infection with cutaneous staphylococcus can lead to serious complications.
Cutaneous staphylococcus – what is it?
Cutaneous staphylococcus (Staphylococcus epidermidis) is a gram-positive bacterium and one of over 40 species belonging to the genus Staphylococcus. It is part of the normal human flora, usually the skin flora, less commonly the mucosal flora. It is a facultative anaerobic bacterium. Although cutaneous staphylococcus is usually not pathogenic, patients with a compromised immune system are at risk of developing an infection. These infections are usually acquired in a hospital.
Cutaneous staphylococcus is a particular problem for people with catheters or other surgical implants because they are known to form biofilms that grow on these devices. Being part of the normal skin flora, cutaneous staphylococcus is a common cause of contamination in samples sent to a diagnostic laboratory.
See also: Diseases that you can catch through a handshake
Cutaneous staphylococcus – how does it work?
One of the key factors enabling coagulase-negative species (such as dermal staphylococcus) to survive in a harsh environment is the production of biofilm. Biofilm formation occurs with initial adhesion to a foreign surface or endothelium, leading to accumulation in multicellular structures.
Once formed, the biofilm protects against the host’s innate defense through protective exopolymers called poly-y-glutamic acid. Other exotoxins and endotoxins also appear to cause an immune response and virulence within the host, one of which is the PSM peptide toxin, which codes for methicillin resistance.
Cutaneous staphylococcus – who is at risk?
Cutaneous staphylococcus is one of the most common causes of nosocomial bloodstream infections. Patients with prosthetic valves, cardiac devices, central lines, catheters, and those taking intravenous drugs are at greatest risk of contracting these types of staphylococcus. Cutaneous staphylococcus is also very common in newborns.
See also: Hospital infections. There are still too many of them
Cutaneous staphylococcus – signs of infection
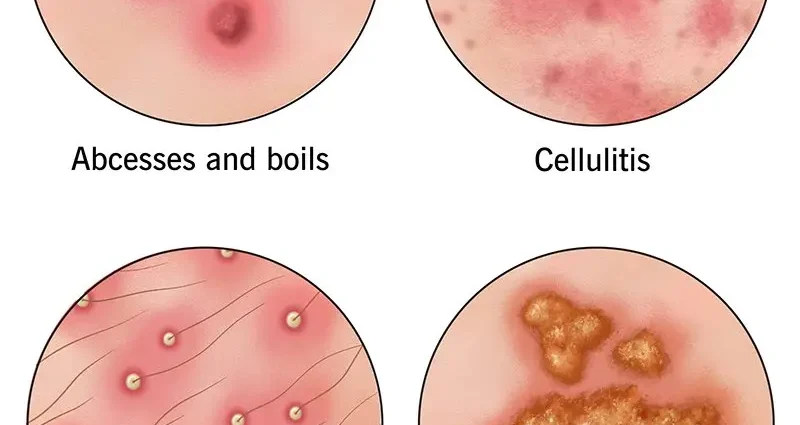
Cutaneous staphylococcus can cause wound infections, boils, sinus infections, endocarditis, and other inflammations. The bacteria can stay in “hiding places” in the body for a long time, where they are not noticed by the immune system, and therefore also remain unaffected. As soon as the conditions for a new infection are favorable for the bacteria, for example, if a person has a weak immune system, the bacterium can re-ignite foci of inflammation which can become chronic and – if the pathogen is multi-resistant – hard to combat.
Symptoms of cutaneous staphylococcus infection are divided into types – hospital and non-hospital.
Hospital symptoms:
- pneumonia characterized by severe coughing and difficulty breathing;
- blood clots with symptoms of chills, fever and often fast and uneven breathing
- wound infection during surgery, manifested by severe redness, pain and even swelling;
- peritonitis;
- osteomyelitis.
Out-of-hospital symptoms:
- boils;
- barley;
- abscesses;
- impetigo;
- various eruptions under the skin;
- weakness;
- fever;
- pain in diseased areas;
- inflammation of follicle.
Cutaneous staphylococcus – diseases
Cutaneous staphylococcus can manifest in many ways in the human host, including local and systemic infections. Below are some of the most common diseases caused by cutaneous staphylococcus.
Infections associated with intravascular catheters
Cutaneous staphylococcus and other coagulase negative staphylococci are one of the leading causes of catheter-related bloodstream infections. Infection largely occurs when bacteria migrate from the patient’s skin to the surface of the catheter. Local symptoms such as inflammation, erythema, or abscess around catheter insertion may occur in patients with a catheter-related infection. They may also show systemic symptoms such as fever, hypotension and other sepsis symptoms.
Infective endocarditis
Cutaneous staphylococcus is one of the most common staphylococcal species causing infective endocarditis in both the valve prosthesis and the natural valve. Up to 40% of infectious valve endocarditis (PVE) cases are caused by coagulase negative staphylococci. When bacteria produce a biofilm in the heart valves, they can accumulate and form vegetation. Patients with infective endocarditis may show fever, chills, malaise, night sweats, and shortness of breath. On physical examination, the patient may show cardiac murmurs as well as ecchymoses and / or fragmentary hemorrhages. Uncommonly, other clinical signs include Janeway’s symptoms, Osler’s nodules, and Roth’s spots.
Cardiac devices, joint prostheses and CNS fistula infection
Cutaneous staphylococcus can cause infections due to the implantation of medical devices such as cardiac devices, orthopedic devices, and CNS fistulas. Up to 20% of patients with cardiac devices may become infected and may show signs of erythema, pain, abscess around the site of infection, and sepsis. In patients with a joint prosthesis infection, pain and abscesses may occur around the prosthesis insertion site.
Fistula infection may be asymptomatic, but it can also cause headache, dizziness, nausea, vomiting, and mental disturbances.
Cutaneous staphylococcus – what diseases can it cause?
Cutaneous staphylococcus can cause diseases such as:
- peritonitis;
- endocarditis;
- meningitis;
- inflammation of the urinary system;
- bacteremia;
- osteomyelitis.
Cutaneous staphylococcus in children
It should be emphasized that the immune system of children is more sensitive than the immune system of an adult, which means that cutaneous staphylococcus can be dangerous also for the youngest. If a child suffers injuries, it is recommended to dress them properly and protect them from external factors to minimize the chances of infection. If your child develops skin changes without any reason, you should see your doctor.
Cutaneous staphylococcus can cause in children, for example:
- inflammation of follicle;
- staphylococcus sycosis;
- multiple abscesses;
In children, cutaneous staphylococcus can also cause diseases such as:
- bullous impetigo;
- bullous inflammation;
- peeling of the skin.
See also: The mother of an infected newborn baby sued the hospital. The court issued the verdict
Cutaneous staphylococcus – diagnosis
Blood cultures are required prior to starting antibiotic therapy in patients with suspected catheter-related bloodstream infections. It is recommended to collect cultures from both the peripheral vein and catheter site for the most reliable results. Given that coagulase negative staphylococci are often found as contaminants in blood cultures, having two positive blood culture bottles with these species will increase the positive predictive value.
Patients suspected of having endocarditis based on the clinical picture will also require blood cultures and an echocardiogram (Echo of the heart). A minimum of three blood culture sets from different venipuncture sites are recommended.
The echocardiogram is essential in the diagnosis of endocarditis. Transthoracic echocardiogram (TTE) is the first step, which has a high sensitivity of up to 75% and detail of around 100%. If the TTE is inconclusive and there is clinical suspicion of endocarditis, a Transesophageal echocardiogram (TEE) may be performed for further diagnosis.
In addition, doctors carry out urine tests in the case of skin staphylococcus infection, as well as take a smear from the places on the skin affected by the bacterium. Very often, in the case of cutaneous staphylococcus, nasal swabs and throat swabs are also collected. Thanks to this, it will be known what antibiotic to include in the treatment.
See also: Six myths about antibiotics
Cutaneous staphylococcus – treatment
Treatment of cutaneous staphylococcal infections largely depends on the type and severity of the infection. Patients with systemic infection require parenteral treatment. Methicillin resistance is present in more than 80% of coagulase-negative staphylococcal isolates. Intravenous vancomycin is the choice of empirical therapy for staphylococcal epidermidis infection, as methicillin resistance should be assumed. If the pathogen is methicillin sensitive, treatment may be limited to beta-lactam antibiotics such as nafcillin and oxacillin. The duration of therapy depends on the clinical picture. Typically, prosthetic and medical devices need to be removed to control the source of infection.
Due to the fact that the patient’s immunity plays an important role in infection with cutaneous staphylococcus, it is important to pay attention to the diet, adequate sleep and rest, and to give up stimulants (coffee, cigarettes or alcohol). Doctors often recommend the use of appropriate ointments.
See also: Smoking is a disease!
Cutaneous staphylococcus – home remedies
Home treatments can also be used for cutaneous staphylococcus. These include:
- warm water compresses to cleanse the wounds of pus;
- tea tree oil has a strong antimicrobial effect (works well in treating infected areas of the skin);
- turmeric mash, which has a strong antibacterial effect;
- manuka honey compresses (having anti-inflammatory and anti-itching properties) acting on the affected areas and on even the most resistant strains of staphylococcus;
- apple cider vinegar to remove toxins.
In addition to compresses and wound pulps, inhalations, for example from grated onions, twice a day for a week also work well. Birch sap also has good healing properties, and the betulin contained in it has strong antibacterial properties.
See also: Birch bark betulin supports metabolism
Cutaneous staphylococcus – prognosis
The prognosis depends on the type of infection and the patient’s comorbidities at the time of infection. In low birth weight neonates, the mortality rate from cutaneous staphylococcal sepsis was 4,8% and 9,4%. In people with coagulase-negative staphylococcal endocarditis, the mortality rate can be as high as 36%.
See also: RS virus attacks again. It is especially dangerous for infants and premature babies
Cutaneous staphylococcus – complications
Sepsis and septic shock are complications of high mortality that can occur from catheter-related infections. Mortality from septic shock can be as high as 20 to 30%. Prosthetic endocarditis or native valve endocarditis can lead to complications including septic embolism, septic aneurysm, paravalvular abscess, and heart failure.
Patients undergoing procedures requiring the implantation of prostheses or medical devices should be informed about the possibility of infection with cutaneous staphylococcus. If patients are knowledgeable about the common signs and symptoms of infection, this will lead to faster evaluation and treatment, which will overall lead to a reduction in mortality and complications.
Content from the site medTvoiLokony they are intended to improve, not replace, the contact between the Website User and his doctor. The website is intended for informational and educational purposes only. Before following the specialist knowledge, in particular medical advice, contained on our Website, you must consult a doctor. The Administrator does not bear any consequences resulting from the use of information contained on the Website. Do you need a medical consultation or an e-prescription? Go to halodoctor.pl, where you will get online help – quickly, safely and without leaving your home.