Contents
Crohn’s disease is an inflammation of the intestinal wall, which has an autoimmune nature. Periods of exacerbation are replaced by periods of remission, but they cannot be called full-fledged. With this chronic pathology, the entire digestive tract as a whole becomes inflamed. The process involves not only the mucous membrane of the organ, but also its submucosal and muscular layer. This autoimmune disease affects 50-60 people out of 100.
What is Crohn’s disease?

In Crohn’s disease, healthy areas of the intestine alternate with inflamed areas. Sometimes the pathological process covers large areas, and sometimes very small ones. Not only the intestines are exposed to inflammation, but also the stomach with the esophagus, but this does not always happen.
Most patients are diagnosed with lesions of the small intestine in the region of the ileocecal canal. Sometimes the disease manifests in the ileum and spreads further. This affects both the small and large intestines. Its examination allows visualization of ulcers. They differ in shape and size. Healthy areas of the intestine are replaced by areas of stenosis and seals. However, the structure of goblet cells and crypts is not disturbed.
Classification
Depending on where the inflammation is concentrated, the following forms of Crohn’s disease are distinguished:
Ileitis (lesion of the ileum).
Ileocolitis (lesion of the ileum and colon). This form of pathology is more common than others.
Gastroduodenitis (damage to the stomach and duodenum).
Colitis (damage to the large intestine).
Eunoileitis (damage to the small intestine and ileum).
Depending on the characteristics of the course of pathology, there are acute and chronic forms of Crohn’s disease.
Causes of Crohn’s disease

Until now, scientists have not figured out the exact causes of Crohn’s disease. There are only a few theories, but none of them are supported by scientific facts, among them:
Hereditary predisposition.
Theory of antigen formation.
Infectious theory.
autoimmune theory.
Which of them is correct is not known. Therefore, each of them needs to be considered in more detail.
Theory of antigen formation. Adherents of this theory believe that antigens from food are attached to the intestinal walls. A person’s own antibodies react to them. This triggers an inflammatory response in the form of Crohn’s disease.
Infection theory. There are scientists who suggest that Crohn’s disease is a consequence of past infections. They believe that various viruses and bacteria that live in the human gastrointestinal tract cause pathology.
autoimmune theory. Most scientists are of the opinion that Crohn’s disease has an autoimmune origin, that is, it develops due to malfunctions in the human immune system. These failures lead to the fact that immune cells begin to attack their own intestinal tissues, causing inflammation and destruction.
Genetic factors. Genetics is critical in terms of the development of Crohn’s disease. The likelihood of pathology in people with a burdened family history is 10 times higher. Crohn’s disease often affects siblings and identical twins.
There is evidence that the probability of developing the disease in a child is 70% if one of the parents suffered from it. And the symptoms will coincide by 80%.
The probability of developing pathology in smokers and drinkers, in citizens living in an unfavorable environmental situation increases. Increase the risk of Crohn’s disease frequent stress and chronic emotional overstrain.
However, most scientists are of the opinion that Crohn’s disease still has an autoimmune nature.
Symptoms of Crohn’s Disease

General symptoms of pathology are due to intoxication of the body and the deterioration of its resistance.
You can suspect Crohn’s disease by the following signs:
Chronic fatigue.
Malaise.
High body temperature.
Anemia, bleeding disorder.
Abdominal pain, stool disorder.
These symptoms are characteristic of some other diseases, such as appendicitis, ulcerative colitis, IBS. Therefore, you cannot try to make a diagnosis on your own. If a person is haunted by cramping abdominal pain that does not stop within 6 hours, you should consult a doctor.
Local Symptoms

The symptoms of Crohn’s disease can be mild or severe. Most often, with each period of exacerbation, they gain strength. During remission, a person lives a normal life without suffering from any pathological symptoms.
Local manifestations of Crohn’s disease:
Diarrhea. It is the liquefaction of the stool that comes to the fore in patients with Crohn’s disease. The process of digestion of food occurs with disturbances, the intestines are reduced all the time, so the feces are liquefied, the urge to empty the intestines becomes more frequent.
Increased body temperature, deterioration of well-being. Most often, the hyperthermic reaction is not too intense, the mark on the thermometer does not exceed 38 ° C.
Pain in the abdomen, spasms in the intestines. Since the intestinal walls become covered with ulcers, and the organ itself becomes inflamed, a person experiences pain. Sometimes they are weak and sometimes very strong. In some cases, the pain is accompanied by nausea and vomiting.
Blood in feces. Bleeding can be hidden, while blood is present in the stool, but it is not possible to see it with the naked eye. With severe damage to the intestines, blood will be noticeable.
Lack of desire to eat, weight loss. A person gradually loses his appetite, which occurs due to persistent inflammation of the digestive tract.
Pain in the anus. It occurs when a fistula forms in a person.
Ulcers in the mouth.
Extraintestinal symptoms of the disease
Extraintestinal symptoms of Crohn’s disease include:
Violations of the organs of vision with the development of keratitis, uveitis, conjunctivitis.
The defeat of the skin in the form of pyoderma and nodular erythema.
Damage to articular tissues with the development of monoarthritis or spondylitis.
Stomatitis.
Violations of the hepatobiliary system in the form of cirrhosis, fatty degeneration of the liver, cholangiocarcinoma.
Kidney damage with the development of cystitis, hydronephrosis or pyelonephritis.
Increased risk of developing cancerous tumors, namely, carcinoma of the large intestine.

Diagnosis of Crohn’s disease
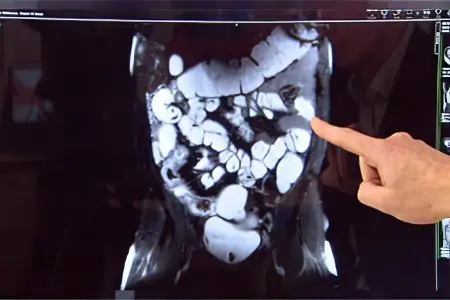
To make a diagnosis, a comprehensive examination of the patient is required. It is important not only to detect the disease itself, but also to clarify the degree of its development, the activity of the pathological process. Only in this way will it be possible to choose the optimal therapy and improve the quality of life of the patient.
Diagnosis is carried out in dynamics, with each episode of exacerbation of the pathology, which will prolong remission. Depending on the results obtained at each specific stage of the disease, the treatment regimen is adjusted.
Collection of anamnesis. During the first visit to the doctor, you will need to answer the following questions from the doctor:
How long ago did the first signs of the disease appear?
How often does the pathology worsen?
Is there any relationship between periods of exacerbation and certain events (with eating, smoking, taking medications, etc.)?
What is the state of health of a person at the time of admission?
Has the disease been treated before?
When the doctor receives the necessary information, he will refer the patient for testing.
Analyzes. With the help of analyzes, it will be possible to understand how much the disease has affected human health. Without fail, the patient will need to donate urine, feces and blood. According to the blood test, it will be possible to clarify whether there is a decrease in the level of hemoglobin in the blood, whether the value of leukocytes in the blood is increased, and also to determine the ESR.
In addition to the general blood test, its biochemical study is carried out, during which the following values uXNUMXbuXNUMXbare determined:
Fibrinogen level (values will be increased).
Gamma globulin fraction level (values will be increased).
Albumin level (values will be lowered).
The presence of C-reactive protein in the blood (indicates an inflammatory reaction).
Vitamin B12 and folic acid levels (values will be reduced).
An immunological blood test can detect many immune complexes, as well as a decrease in the number of T-lymphocytes.
Urine analysis can also be used to judge the stage of development of the disease. If it has an acute course, then protein and blood will be found in the urine. Also, its analysis allows you to clarify whether the kidneys are involved in the pathological process, whether there is an infection of the urinary system.
Blood, white blood cells, and epithelial cells are found in the stool of a patient with Crohn’s disease. Sometimes parasites and bacteria are found in the stool. It is good if the feces are taken for analysis during the acute period of the disease. So the study will be as informative as possible. To clarify the diagnosis, the doctor can take tissues from the intestinal mucosa and send them for examination.
Colonoscopy. This study is carried out using special equipment. A tube with a camera is inserted into the colon, which displays an image on a monitor. This allows the doctor to visualize the state of the intestine from the inside. If the doctor detects ulcerative defects or other tissue changes, then he collects them and sends them for further research.
Endoscopy. This study is prescribed for all patients with Crohn’s disease. A tube with a video camera is inserted into the anus or into the mouth. With its help, the doctor assesses the state of the digestive tract.
Endocapsular colonoscopy. This is a modern study that allows you to assess the state of the entire digestive tract with maximum comfort for a person. He will simply need to swallow the capsule, which will pass through the intestines, taking a series of shots. The doctor will only have to study them. This study makes it possible to examine each section of the small intestine, which is impossible with classical endoscopy.
Signs that will indicate Crohn’s disease:
erosion. They look like small ulcers around which scar tissue has formed. Erosions are surrounded by healthy parts of the intestinal wall.
Ulcerative defects. They affect the intestine deeper than erosion, sometimes reaching the muscle structures of the organ.
Swelling of the mucous membranes. Between the ulcers, edematous tissue areas will be noticeable. Therefore, the intestines from the inside resemble a cobblestone pavement.
Scarring. These inelastic tissues pull the walls of the defects together, thereby narrowing the intestinal lumen.
Fistulas. They are represented by channels that are formed due to the destruction of the tissues of the organ. Fistulas can connect the intestines to other organs, such as the bladder, or to the external environment, such as the abdominal wall and skin.
X-ray. During the examination, pictures of the abdomen are taken. This eliminates the expansion of the colon and perforation of the intestine.
Irrigography. This procedure involves examining the intestines using x-rays, but with the use of a contrast agent. Both air and barium can act as a contrast.
Ultrasound. The study provides information about the size of intestinal loops, the presence of effusion in the abdominal cavity.
CT and MRI. These studies are indicated for patients with a complicated course of pathology, when there is a suspicion of damage to other organs. In addition, MRI provides information about the state of the lymph nodes, the narrowing of certain parts of the intestine, the degree of its damage, and the presence of fistulas.
Biopsy and histology. A biopsy involves the collection of altered tissues of the organ. The resulting biopsy is sent for histology. The study is carried out in a laboratory, where the materials are carefully studied. This will allow the doctor to make the correct diagnosis.
Exclusion of diseases similar to Crohn’s disease. There are a number of pathologies that can resemble Crohn’s disease in their symptoms.
Therefore, it is important to carry out differential diagnosis with such disorders as:
Salmonellosis, dysentery and other intestinal infections.
Appendicitis.
Chronic infections of the pelvic organs.
Celiac disease, in which the human body does not perceive gluten.
Enteritis and chronic non-ulcerative colitis.
Nonspecific ulcerative colitis. Unlike Crohn’s disease, this pathology does not affect the entire intestine.
Autoimmune diseases: scleroderma and systemic lupus erythematosus.
Bowel cancer.
Which doctor treats Crohn’s disease?

To identify and treat Crohn’s disease, you need to contact a gastroenterologist. The doctor will examine the patient and give him a referral for tests and instrumental examination. Then the doctor will be able to make a conclusion about the state of human health.
Sometimes, to clarify the diagnosis, consultation of such specialists is required, such as:
Immunologist. It will detect deviations in the functioning of the immune system.
Nephrologist. Patients with suspected kidney disease are referred to this specialist.
Hematologist. The doctor will prescribe a blood transfusion to the patient, if necessary.
Infectious disease. The specialist is engaged in the detection of infectious causes of the development of pathology.
Dermatologist. His consultation is needed in case of damage to the skin.
A visceral surgeon examines a patient when an operation is indicated for him. A consultation of specialists allows you to maximize the prognosis of a patient with Crohn’s disease.
Therapies
Treatment for Crohn’s disease is based on medication. They allow you to remove the inflammatory reaction, reduce the frequency of bowel contractions, get rid of stool disorders, reduce cases of exacerbation of the pathology, achieve a stable remission.
If the pathology has a severe course, then serious medications are required. Sometimes in the acute phase of the disease, the help of a surgeon is needed. It is possible to decide on therapy only together with a specialist who knows the patient’s medical history.
There is no specific medicine that could help to cope with Crohn’s disease once and for all. Therapy must be comprehensive. The sooner it is started, the higher the chances of success.
The main tasks to be solved:
Improve patient well-being.
Reduce pain intensity.
Get rid of diarrhea.
Stop bleeding.
Saturate the body with nutrients.
Anti-inflammatory treatment. The drugs that are prescribed to stop the inflammatory reaction differ depending on the characteristics of the course of the pathology.
Sulfasalazine and Mesalazine are taken by mouth, but they work in the rectum. With the localization of the inflammatory process in the small intestine, these drugs will be useless.
Prednisolone and other corticosteroid hormones quickly eliminate inflammation, regardless of where it is concentrated. However, they have many side effects, including: tissue swelling, facial hair growth, sleep disturbance, hypertension, diabetes, osteoporosis, cataracts, glaucoma, decreased immunity. Each patient’s body reacts differently to corticosteroids.
Budesonide (Budenofalk) is the latest generation corticosteroid. It has a pronounced therapeutic effect, but at the same time does not give such a number of complications. However, the drug does not act along the entire length of the intestine, but only in certain sections of it. Hormone therapy should not exceed 4 months. Otherwise, the treatment will do more harm than good. After completion of the course, patients are transferred to receive small doses of immunosuppressants.
Immunosuppressors. These drugs reduce the inflammatory response, but it does so at the expense of immune suppression. Sometimes patients with Crohn’s disease need to take 2 medicines at once.
Drugs that can be used:

Azathioprine (Imuran) and Mercaptopurine (Purinetol). It is these medicines that are most often used in the treatment of intestinal diseases. However, even a short intake of them contributes to the development of side effects such as decreased bone marrow function, hepatitis, pancreatitis. Long-term treatment increases the risk of lymphoma and skin cancer.
Infliximab (Remicade), Certolizumab Pegol (Cimzia), Adalimumab (Humira). These drugs affect a protein called tumor necrosis factor, reducing its activity. Their appointment to patients with Crohn’s disease allows to achieve its stable remission.
Immunosuppressants should be used in the treatment of patients immediately after diagnosis. They must be prescribed to patients with severe pathology. However, tumor necrosis factor inhibitors are not used to treat patients with tuberculosis, viral hepatitis, and other dangerous diseases.
Methotrexate (Rheumatrex). The drug is used in the treatment of cancer patients, people with psoriasis and rheumatoid arthritis. However, it allows achieving remission in patients with Crohn’s disease.
Cyclosporine (Sandimmun Neoral, Ecoral, Panimun Bioral), Tacrolimus (Advagraf, Prograf, Astrograf XL, Tacrosel). These drugs are indicated for patients with Crohn’s disease complicated by fistulas, as well as for those patients who are not helped by classical anti-inflammatory drugs to achieve remission. It must be remembered that Cyclosporine can cause a variety of adverse reactions, up to damage to the tissues of the kidneys and liver. Therefore, preparations based on it are prescribed for short courses.
Natalizumab (Tysabri) and Vedolizumab (Entivio). These drugs prevent molecules that are located on the surface of the intestine and integrins (leukocyte molecules) from binding. This prevents an autoimmune reaction, so symptoms of Crohn’s disease do not occur. In severe and moderate pathology, Natalizumab is prescribed. Its reception can cause the development of multifocal leukoencephalopathy, in which the brain suffers, because of which a person can even become disabled. Therefore, a trial use is required before starting the course. Vedolizumab does not lead to such severe health effects, but works in the same way as Natalizumab.
Ustekinumab (Stelara). This drug was developed to treat psoriasis, but research shows it can help treat Crohn’s disease.
Antibiotics. Antibacterial drugs are indicated for the appointment when the patient develops complications of Crohn’s disease, which are accompanied by the addition of an infection, including abscesses and fistulas. These drugs do not affect the underlying pathology.
More often than not, they prescribe such means as:
Metronidazole (Flagyl, Trichopol, Klion). Metronidazole has been the drug of choice in the treatment of Crohn’s disease in recent years. When prescribing it, you need to remember that it can cause muscle pain, numbness, weakness, tingling in the limbs.
Ciprofloxacin. This drug can reduce the intensity of the symptoms of Crohn’s disease. If there is a need to take antibiotics, then modern medical science recommends giving preference to Ciprofloxacin, and not Metronidazole.
Other medicines. There are drugs that can improve the quality of life of patients with Crohn’s disease and reduce its manifestations.
These funds include:

Drugs to stop diarrhea. If it has an uncomplicated course, then Citrucel can be used. In severe cases of diarrhea, Loperamide or Imodium is indicated for admission.
Pain relief drugs. In Crohn’s disease, analgesics familiar to most people, such as Ibuprofen or Naproxen, are not prescribed, as they can worsen the course of the pathology. Acetaminophen (Tylenol) is used for pain relief.
Iron preparations for the treatment of iron deficiency anemia.
Vitamin B12 injections for the treatment of B12 deficiency anemia.
Vitamin D and calcium preparations. Crohn’s disease increases the risk of developing osteoporosis. To prevent this from happening, the patient is prescribed vitamins and minerals.
Surgical intervention
Surgery for Crohn’s disease is only considered when other treatments have failed to achieve remission. More than half of patients undergo at least one intestinal intervention. Despite this, the possibility of recurrence of the pathology cannot be ruled out. Therefore, doctors resort to radical methods only in extreme cases.
Preference is given to laparoscopy. This minimally invasive procedure is more easily tolerated by patients and does not cause severe complications.
Indications for surgical intervention are:
The formation of intestinal strictures, due to which feces cannot leave it normally.
Fistula formation.
Intestinal suppuration.
The development of intra-abdominal bleeding.
Formation of a perforated ulcer of the intestine.
After the operation, the patient is shown medication.









