Contents

Chronic renal failure is a progressive decline in kidney function associated with the death of nephrons or their replacement with connective tissue against the background of chronic pathology.
Nephrons are important structural units of the kidneys, which are involved in the purification of blood from nitrogenous toxins, contribute to the production of erythropoietin, the removal of excess salt and water, and the absorption of electrolytes.
In this regard, as the functioning of the kidneys deteriorates, the functioning of the body as a whole is disrupted. Various organs and systems suffer. Although modern medicine has advanced capabilities in terms of treating kidney pathologies, nevertheless, up to 40% of them sooner or later turn into chronic renal failure.
Causes of chronic renal failure
The causes of chronic renal failure lie in various diseases. Almost any protracted kidney disease of the method, after some time, leads to the inability of the organs to function normally or to a complete failure. In other words, we can say that chronic renal failure is only a matter of time, provided that a person has kidney disease and does not receive adequate treatment. However, not only diseases of the kidneys themselves can lead to the inability of these organs to work normally.
Therefore, the full list of causes provoking this pathological process is as follows:
In the first place are various renal diseases: glomerulonephritis, pyelonephritis, chronic tubulointerstitial nephritis. Kidney tuberculosis, hydronephrosis, polycystosis, kidney neoplasms, nephrolithiasis are dangerous;
Diseases of the urinary tract, including urethral strictures, kidney and bladder stones;
Diseases of the cardiovascular system, for example, angiosclerosis of the renal vessels. Hypertension, although rare, still leads to the development of renal failure;
Diabetes.
Systemic pathologies – hemorrhagic vasculitis, amyloidosis of the kidneys.
The pathogenesis of the disease is based on the progressive death of nephrons. First, the process of the organs becomes less productive, after which more pronounced violations of kidney function begin to increase. The parenchyma is gradually replaced by connective tissue with its subsequent atrophy and shrinkage of the organ. A distinctive feature of this process is the impossibility of the kidney to recover, that is, the parenchyma does not regenerate, the compensatory capabilities of the kidneys are depleted. This can happen in a short time (in a few months), but it is possible that the process will drag on for many years.
Symptoms of chronic renal failure
The symptoms of chronic renal failure are as follows:
Appearance of patients. Practically no characteristic external signs will be noticeable until such time as there is a pronounced decrease in glomerular filtration of organs. Then it will be possible to visualize the following violations:
The pallor of the skin is due to anemia, which gradually increases. Violations of the water and electrolyte balance lead to increased dryness of the skin. For the same reason, the skin loses elasticity, it is possible to acquire an icteric color;
Subcutaneous hematomas often begin to occur. Bruising appears without previous trauma or bruising;
On the skin of patients there are scratches, which are caused by severe painful itching;
The face becomes very swollen. Edema extends to the limbs, to the stomach;
Muscle tone decreases, they become flabby, which affects their functionality. This has a negative impact on a person’s ability to work. Muscle twitches and convulsions against the background of clear consciousness are explained by a drop in the level of calcium in the blood;
The skin remains dry even at a time when the patient is experiencing strong excitement or stress.
Nervous system disorders. Patients become lethargic, sleep poorly at night, during the daytime they feel tired and overwhelmed. Cognitive functions suffer, primarily memory and attention. The ability to learn and perceive information is deteriorating. Often patients complain of coldness in the extremities, a tingling sensation, “goosebumps”. It is associated with a disorder of the peripheral nervous system. As the pathological process progresses, movement disorders are observed in the upper and lower extremities.
Urinary system. The volume of urine at the initial stages of the development of the disease increases, and the patient often goes to the toilet at night. As the insufficiency develops, the volume of urine excreted becomes less and less, edema continues to increase, complete anuria is possible.
Violations of the water-salt balance. The thyroid gland begins to produce parathyroid hormone in large volumes. As a result, phosphorus levels rise and calcium levels fall. This causes frequent spontaneous fractures against the background of softening of the bone tissue.
There is constant thirst, the patient’s mouth is dry;
With a sharp rise from a place, there is a darkening in the eyes, muscle weakness. This is due to the washing out of sodium from the body;
Against the background of excess potassium in the blood, muscle paralysis increases;
Possible violations of the respiratory function;
Water-salt balance is essential for the functioning of the body as a whole. Failures can lead to serious problems in the work of the heart, up to its stop.
nitrogen imbalance. If the glomerular filtration rate falls below 40 ml per minute, the patient develops signs of enterocolitis. Against the background of an increase in the level of urea and uric acid in the blood, as well as an increase in creatinine, an ammonia smell will come from the patient’s mouth, articular lesions will begin to develop.
Manifestations from the cardiovascular system. The function of hematopoiesis suffers, which is expressed in anemia, lethargy, increased fatigue and weakness.
Pericarditis and myocarditis develop;
Blood pressure rises;
There are pains in the heart of a dull and aching nature, shortness of breath increases, the heart rhythm is disturbed;
Acute heart failure is a complication of renal failure and can provoke the death of the patient.
At a late stage in the development of renal failure, a “uremic lung” develops. Interstitial edema increases, a bacterial infection joins, which is associated with a drop in immunity.
As for the digestive system, its work is disrupted. Appetite disappears, nausea and vomiting may occur. Often, the salivary glands and the mucous membrane of the oral cavity react with inflammation. Sometimes patients reach the stage of anorexia due to aversion to food. Uremia causes ulcers of the stomach and intestines, which can be complicated by bleeding. Acute hepatitis also often accompanies uremia.
Stages of chronic renal failure
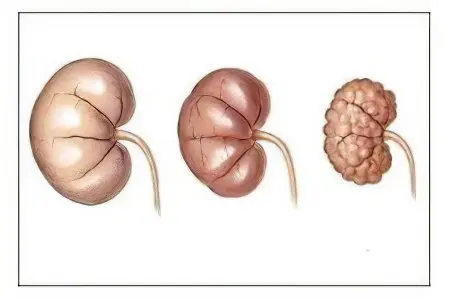
The stages of chronic renal failure are characterized by the steady destruction of the renal glomeruli with their replacement by scar tissue. At the same time, compensatory changes occur in the remaining intact glomeruli.
Therefore, the pathological process develops gradually, passing through several stages:
Initial or latent stage. The glomerular filtration rate is about 60-70 ml per minute. This is considered a variant of the norm, but kidney damage is already present, and there is also an imbalance between nighttime and daytime diuresis. Patients, as a rule, do not present complaints at this time, although some decrease in working capacity is possible.
compensated stage. Efficiency becomes worse, fatigue increases, a feeling of dryness appears in the mouth. The filtration rate varies from 30 to 60 ml/min. It is worth noting that for the elderly, this rate is a variant of the norm, if there are no other structural damage to the kidneys. Nocturnal diuresis predominates, urine osmolarity falls, creatinine and urea in the blood are still at the normal level, but there are fewer and fewer working nephrons.
Intermittent stage characterized by an increase in symptoms, since the filtration rate does not exceed 15-30 ml per minute, and sometimes it can drop to 30 ml/min. Depending on this, one or another degree of brightness of the clinical picture will be observed. However, there is always an increase in the volume of urine excreted, appetite worsens, and excessive dryness of the skin appears. In 50% of cases, there is an increase in blood pressure. Daily diuresis falls, the content of creatinine and urea in the blood increase.
terminal stage characterized by a drop in filtration rate to 15 ml/min or less. Anuria may develop. The skin acquires a yellow-gray tint, becomes flabby. Patients fall into apathy, drowsiness, inactive. Signs of poisoning are increasing due to an increase in the level of nitrogenous toxins in the blood. The water-electrolyte balance is disturbed, organs and systems work intermittently. First of all, it concerns the heart and nervous system. If dialysis is not carried out at this stage, then the patient dies.
Complications
Complications of chronic renal failure are as follows:
Anemia against the background of oppression of the hematopoietic system. Violation of the coagulation properties of the blood, the development of thrombocytopenia;
Hypertension, myocarditis, pericarditis, uremic pneumonia;
congestive heart failure;
Confusion, delirium, hallucinations, peripheral polyneuropathy;
Stomatitis, enterocolitis, atrophic gastritis, gastric and duodenal ulcers with possible bleeding;
Osteoporosis, osteomalacia, skeletal deformities, bone fractures, arthritis;
Lymphocytopenia, dysfunction of the immune defense and the development of purulent-septic conditions.
Diagnostics
Diagnosis of chronic renal failure is within the competence of a nephrologist and is based on the performance of laboratory tests.
Among them:
Biochemical analysis of urine;
Blood chemistry;
Reberga sample;
Trial of Zimnicko.
In addition, ultrasound of the kidneys, ultrasound of the vessels of the kidneys is indicated. With regard to radiopaque urography, it should be done very carefully, since most of the substances used for this purpose have a toxic effect on the kidneys.
How to treat kidney failure?
Treatment of chronic renal failure directly depends on the stage of the pathological process and whether the patient has other diseases.
It has been established that the initial, latent stage of the pathology may not reveal itself for a long time. Therefore, therapy in most cases is absent.
When the disease is detected at the compensated stage, then very serious treatment is required. They resort to surgical intervention in order to normalize the exit of urine from the organs. This is necessary in order to return the disease to its initial stage. If there is no treatment at this stage, then the compensatory mechanisms of the kidneys will soon run out, and the disease will move to the next stage.
Surgical interventions at the intermittent stage are not performed, as they are associated with high risks. At this stage, palliative treatment and detoxification therapy are carried out. The operation can be performed only when the function of the kidneys is restored.
If the disease has progressed for a long time and is at the last stage, then the struggle will go on for a person’s life. In this case, treatment must be very careful, planned and targeted. This is the only way to succeed.
To prevent disturbances in the work of nephrons, the following treatment is indicated:
Remove the functional load from the nephrons that have not yet lost their efficiency;
Activate the immune defense, which will rid the body of nitrogenous toxins;
Correct the vitamin, mineral and electrolyte balance in the body;
Engage in blood purification using hemodialysis and peritoneal dialysis;
Choose replacement therapy, organ transplantation is possible.
Physiotherapeutic measures are indicated to accelerate the elimination of nitrogenous toxins. This may be a visit to the infrared sauna, taking therapeutic baths, spa treatment. Enterosorbent preparations, for example, Polyphepan, help to correct the pathological process. Lespenefril is prescribed to normalize protein metabolism.
Cleansing enemas and the appointment of laxatives help to get rid of excess potassium in the body. This allows you to reduce the concentration of the trace element in the intestine and accelerate its excretion.
Up to 4 times a year, patients are placed in a hospital to perform infusion therapy. A course administration of glucose, Reopoliglyukin, diuretics, anabolic steroids, sodium bicarbonate, vitamin B and ascorbic acid is carried out.
Hemodialysis
Hemodialysis, although it is a complex procedure, many patients cannot do without it.
Its mechanism is as follows:
Arterial blood enters the dialysis machine, where it interacts with the membrane, which has incomplete permeability. On the other side of the membrane is the dialysis solution;
Nitrogenous toxins from the patient’s blood gradually pass into this solution, and the blood is cleansed;
Not only toxins are removed, but also excess water, which brings the water-salt balance of the body back to normal;
Purified blood is returned to its owner.
The duration of the procedure is from 4 to 5 hours, the multiplicity is once every two days.
As for peritoneal dialysis, it is carried out for patients who have severe comorbidities and do not tolerate heparin. A special sterile solution is injected into the abdominal cavity through a catheter, it is saturated with decay products, after which it is brought back through the same catheter. This method can be applied even at home.
Operation
Kidney transplant surgery is the most radical treatment. It is carried out in specialized nephrological medical centers. Almost all patients with chronic renal failure require transplantation. But the problem lies in the selection and search for a donor. Therefore, you can wait for your turn for decades. The kidney is transplanted into the iliac region with implantation of the ureter into the bladder, into its side wall.
It is very important that compatibility is matched by tissue type, Rh factor, cross-check and HLA typing system. However, there is always a risk of organ rejection, therefore, after the operation, preventive measures are taken with the help of immunosuppressive drugs.
Recommendations after discharge
In a hospital, patients are treated during an exacerbation of a chronic process, as well as in the last stages of the disease. In all other cases, a person can receive treatment at home, with regular visits to the doctor to monitor therapy.
To relieve the load from working intact nephrons, the following measures are taken:
Refuse drugs that have a toxic effect on the kidneys;
Reduce physical activity, but this does not mean a complete rejection of them;
Sources of infection must be promptly eliminated and treated;
It is necessary to use drugs that allow the removal of toxins from the intestines;
It is important to follow a dietary plan. Give up salt and control your daily protein intake.
You can not consume more than 60 g of protein per day, and in conditions of exceeding the level of nitrogenous compounds in the body, this figure is reduced to 20 g. However, amino acids must be supplied to the body in a normal, balanced amount. If there is high blood pressure, it is not possible to get rid of edema, then you should not consume more than 4 g of salt per day. However, this restriction is removed as soon as the patient’s condition improves, since the lack of sodium in the body is no less dangerous. It has been established that the rejection of salt provokes hypokalemia and disrupts filtration.
The more a person sweats, the faster nitrogenous toxins are eliminated from the body. Therefore, you should not refuse physiotherapy, if there are no other contraindications for their implementation. This is an infrared sauna, therapeutic baths, treatment in sanatoriums.
Hemodialysis can also be done at home. For this, specialized devices have been created to make this procedure easier and safer. However, this practice is not common, so patients are forced to regularly visit medical facilities. In addition, peritoneal dialysis can be performed at home to remove uremic waste products from the body.
[Video] Dr. Berg – #1 Food for Kidney Disease. How to support kidney health:









