Contents
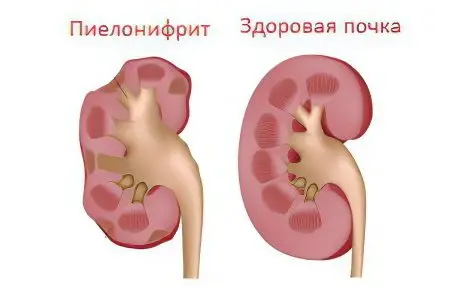
Chronic pyelonephritis is a disease that has an infectious and inflammatory nature in which the calyxes, pelvises and tubules of the kidneys are involved in the pathological process, followed by damage to their glomeruli and blood vessels.
According to available statistics, chronic pyelonephritis among all diseases of the genitourinary organs with an inflammatory nonspecific nature is diagnosed in 60-65% of cases. Moreover, in 20-30% of cases it is a consequence of acute pyelonephritis.
Most often, the development of chronic pyelonephritis affects women and girls, which is due to the peculiarities of the structure of their urethra. As a result, it is much easier for pathogens to enter the bladder and kidneys. Two kidneys are mainly involved in the pathological process of a chronic nature, which is the difference between chronic pyelonephritis and acute. In this case, the organs may not be affected in the same way. The acute course of the disease is characterized by a sharp increase in symptoms, the rapid development of the disease. While chronic pyelonephritis can often occur latently, making itself felt only during periods of exacerbation, which are then replaced by remission.
If a complete recovery from acute pyelonephritis does not occur within three months, then it makes sense to talk about chronic pyelonephritis. Therefore, the chronic form of the disease, according to some reports, is somewhat more common than the acute form.
Symptoms of chronic pyelonephritis
The course of the disease and symptoms of chronic pyelonephritis largely depend on the localization of inflammation, on the degree of involvement of one or two kidneys in the pathological process, on the presence of urinary tract obstruction, and on the presence of concomitant infections.
For many years, the disease can proceed sluggishly, with involvement of the interstitial tissue of the kidney in inflammation. Symptoms are most pronounced during an exacerbation of the disease and can be almost invisible to a person during remission of pyelonephritis.
Primary pyelonephritis gives a more pronounced clinical picture than secondary. The following symptoms may indicate an exacerbation of chronic pyelonephritis:
An increase in body temperature to high values, sometimes up to 39 ° C.
The appearance of pain in the lumbar region, both on one and on both sides.
The occurrence of dysuric phenomena.
Deterioration of the general well-being of the patient.
Lack of appetite.
The occurrence of headaches.
Abdominal pain, vomiting and nausea occur more often in childhood than in adult patients.
The appearance of the patient changes somewhat. He can notice these changes on his own, or the doctor will pay attention to them during the examination. The face becomes somewhat puffy, there may be swelling of the eyelids (see also: Why do the eyelids swell?). The skin is pale, bags under the eyes are not uncommon, they are especially noticeable after sleep.
During the remission period, it is much more difficult to diagnose the disease. This is especially true of primary chronic pyelonephritis, which is characterized by a latent course.
Possible symptoms of this course of the disease are as follows:
Pain in the lumbar region is rare. They are small and not permanent. The nature of the pain is pulling or aching.
Dysuric phenomena are most often absent, and if they occur, they are very weak and proceed almost imperceptibly for the patient himself.
Body temperature, as a rule, remains normal, although in the evening it may slightly increase to 37,1 degrees.
If the disease is not diagnosed and treated for a long time, then people begin to notice increased fatigue, loss of appetite and associated weight loss, drowsiness, lethargy, and sometimes unexplained headaches. (read also: Causes, signs and symptoms of headache, consequences)
As the disease progresses, dysuric phenomena increase, the skin begins to peel off, becomes dry, its color changes to grayish-yellow.
The tongue of patients with long-term chronic pyelonephritis is coated with a dark coating, the lips and oral mucosa are dry.
In such patients arterial hypertension often joins with a pronounced increase in diastolic pressure. Nosebleeds are possible.
The advanced stages of chronic pyelonephritis are characterized by pain in the bones, polyuria with the release of up to 3 liters of urine per day, severe thirst.
Causes

The cause of chronic pyelonephritis etiologically can be only one – it is damage to the kidneys of the microbial flora. However, in order for it to enter the organ and begin to actively multiply, provocative factors are needed. Most often, inflammation leads to infection with para-Escherichia or Escherichia coli, enterococci, Proteus, Pseudomonas aeruginosa, streptococci, as well as associations of microbes. Of particular importance in the development of the chronic form of the disease are L-forms of bacteria that multiply and exhibit pathogenic activity due to insufficient antimicrobial therapy, or when the acidity of urine changes. Such microorganisms are particularly resistant to drugs, are difficult to identify, can simply exist in the interstitial tissue of the kidneys for a long period of time and be active under the influence of favorable factors for them.
Most often, the development of chronic pyelonephritis is preceded by acute inflammation of the kidneys.
Additional stimulating reasons for the chronicization of the process are:
Timely unidentified and untreated causes leading to a violation of the outflow of urine. It can be urolithiasis, urinary tract strictures, prostate adenoma, nephroptosis, vesicoureteral reflux.
Violation of the terms of treatment of acute pyelonephritis, or incorrectly selected therapy. Lack of systemic dispensary control for a patient who has suffered acute inflammation.
The formation of L-bacteria and protoplasts, which can exist for a long time in the kidney tissue.
Decreased immune forces of the body. immunodeficiency states.
In childhood, the disease often develops after acute respiratory viral infections, scarlet fever, tonsillitis, pneumonia, measles, etc.
Having a chronic illness. Diabetes mellitus, obesity, tonsillitis, gastrointestinal diseases.
In women at a young age, a regular sexual life, its onset, the period of pregnancy and childbirth can become an incentive for the development of a chronic form of the disease.
A possible cause of the development of the disease is unidentified congenital developmental anomalies: bladder diverticula, ureterocele, which disrupt normal urodynamics.
Recent studies point to a significant role in the development of the disease of secondary sensitization of the body, as well as the development of autoimmune reactions.
Sometimes hypothermia of the body becomes the impetus for the development of the chronic form of the disease.
Stages
There are four stages of chronic pyelonephritis:
At the first stage of the development of the disease, the glomeruli of the kidneys are intact, that is, they are not involved in the pathological process, the atrophy of the collecting ducts is uniform.
At the second stage of the development of the disease, some glomeruli hyalinize and become empty, the vessels undergo obliteration and narrow significantly. Growing cicatricial-sclerotic changes in the tubules and interstitial tissue.
At the third stage of the development of the disease, the death of most of the glomeruli occurs, the tubules strongly atrophy, the interstitial and connective tissue continues to grow.
At the fourth stage of development of chronic pyelonephritis, most of the glomeruli die, the kidney becomes smaller in size, its tissues are replaced by scar tissue. The organ looks like a small wrinkled substrate with a bumpy surface.
Complications and consequences

Possible consequences of chronic pyelonephritis may be secondary wrinkling of the kidney, or pyonephrosis. Pyonephrosis is a disease that develops at the final stage of purulent pyelonephritis. In childhood, such an outcome of the disease is extremely rare, it is more typical for people aged 30 to 50 years.
Complications of chronic pyelonephritis can be as follows:
Acute renal failure. This condition, which can be reversed, comes on suddenly, is characterized by a pronounced impairment or complete cessation of the functioning of the kidney.
Chronic renal failure. This condition is a gradual extinction of the work of the body against the background of pyelonephritis, caused by the death of nephrons.
Paranephritis. This complication is a process of purulent inflammation of the located perirenal tissue.
Necrotizing papillitis. This is a serious complication that most often occurs in inpatient urological patients, mainly in women. Accompanied by renal colic, hematuria, pyuria and other serious disorders of the body (fever, arterial hypertension). May end in kidney failure. (read also: Causes and symptoms of kidney failure)
Urosepsis. One of the most severe complications of the disease in which the infection from the kidney spreads throughout the body. This condition poses a direct threat to the life of the patient and often ends in death.
Diagnostics
Diagnosis of chronic pyelonephritis should be comprehensive. To make a diagnosis, the results of laboratory and instrumental studies will be required.
Doctors refer patients for the following laboratory tests:
UAC. The chronic course of the disease will be indicated by anemia, an increase in the number of leukocytes, a shift in the blood formula to the left, as well as an increased erythrocyte sedimentation rate.
OAM. According to the results of the analysis, an alkaline environment will be revealed. Urine is cloudy, its density is reduced. The presence of cylinders is possible, bacteriuria is sometimes determined, the number of leukocytes is increased.
The Nechiporenko test will reveal the predominance of leukocytes over erythrocytes, in addition, active leukocytes will be detected in the urine.
Performing a prednisolone and pyrogenal test, when prednisolone is administered to the test subject and several portions of urine are collected at certain intervals.
The Zimnitsky test will reveal a decrease in density in various portions of urine that are collected throughout the day.
The LHC will detect an increased amount of sialic acids, seromucoid, fibrin, urea.
In addition, to confirm the diagnosis and study the state of the organ, it is necessary to perform some instrumental examinations, the choice of which remains with the doctor:
Performing an overview x-ray examination of the kidney area. In the chronic course of the disease, the kidneys will be reduced in size (either, both, or one).
Performing chromocytoscopy. If there is chronic pyelonephritis, then the doctor will note a violation of the excretory function of the kidneys – one or two-sided.
Performing excretory or retrograde pyelography will allow you to detect existing deformities and pathological changes in the calyces and pelvis of the organs.
Ultrasound of the kidneys allows you to detect the asymmetry of organs, their deformation, heterogeneity.
Radioisotope scanning also reveals asymmetry of the kidneys and their diffuse changes.
Detailed structural changes in the organ can be detected by such highly informative studies as CT and MRI.
Renal biopsy and biopsy examination are performed in clinically unclear cases of the disease.
It is important to exclude diseases such as renal amyloidosis, chronic glomerulonephritis, hypertension, diabetic glomerulosclerosis, which can give a similar clinical picture.
Treatment
Treatment of chronic pyelonephritis cannot be complete without an individual approach to the patient and without comprehensive measures aimed at his recovery. It includes following a diet and drinking regimen, taking medications, as well as eliminating causes that may interfere with the normal flow of urine.
In the stage of exacerbation of chronic pyelonephritis, the patient should be placed for treatment and observation in a hospital. With primary pyelonephritis, patients are assigned to a therapeutic or specialized nephrological department, and with a secondary one, to a urological department.
The duration of bed rest directly depends on the severity of the course of the disease and on the effectiveness of the treatment. Diet is an indispensable aspect of the complex treatment of chronic pyelonephritis.
Edema, as a rule, does not occur in such patients, so their drinking regimen should not be limited. Priority drinks are ordinary water, fortified drinks, cranberry juice, juices, compotes, jelly. The volume of fluid entering the body during the day can be equal to 2000 ml. A decrease in its amount is possible according to the doctor’s indications, in the presence of arterial hypertension, in case of violations of the passage of urine. In this case, salt intake is limited, up to its complete elimination.
The decisive moment in the treatment of chronic pyelonephritis is the appointment of antibiotics. They are prescribed as early as possible and for a long time after the sensitivity of bacterial agents to specific drugs that have been sown from the urine has been established. The effect will not be achieved if antibiotics are prescribed too late, for a short time, or if there are any obstacles to the normal passage of urine.
If the disease is diagnosed at a late stage, then even high doses of antimicrobials are often not effective enough. In addition, against the background of existing disorders in the functioning of the kidneys, there is a risk of developing severe side effects even from the most effective drugs. The likelihood of developing resistance also increases many times over.
Before choosing one or another antibacterial drug, the doctor should familiarize himself with the acidity of the urine of patients, as it affects the effectiveness of drugs.
Antibiotics during an exacerbation of the disease are prescribed for up to 8 weeks. The specific duration of therapy will be determined by the results of the laboratory tests performed. If the patient’s condition is severe, then combinations of antibacterial agents are prescribed to him, they are administered parenterally or intravenously and in large doses.
The success of the treatment can be judged by the following criteria:
Absence of dysuric phenomena;
Normalization of blood and urine parameters;
Normalization of body temperature;
The disappearance of leukocyturia, bacteriuria, proteinuria.
However, despite the successful treatment of chronic pyelonephritis, a relapse of the disease is possible, which will occur with a probability of 60% to 80%. Therefore, doctors conduct many months of anti-relapse therapy, which is quite justified in the chronic process of inflammation of the kidneys.
If allergic reactions occur during treatment, it is necessary to perform antihistamine therapy.
When anemia is detected by blood tests, patients are prescribed iron supplements, taking vitamin B12, and folic acid.
Patients with arterial hypertension are recommended to take Reserpine, Clonidine, Gemiton and other antihypertensive drugs in combination with Hypothiazid, Triampur and other saluretics.
In the terminal stages of the disease, organ-preserving surgery or nephrectomy is recommended. Often, it is possible to determine the volume of surgical intervention performed already during the operation.
In addition, patients are shown sanatorium treatment in balneo-drinking sanatoriums.
Nutrition for chronic pyelonephritis

Proper nutrition in chronic pyelonephritis is a prerequisite for complete treatment. It provides for the exclusion from the diet of spicy dishes, all rich broths, various seasonings to enhance the taste, as well as strong coffee and alcohol.
The calorie content of food should not be underestimated; an adult needs to consume up to 2500 kcal per day. The diet should be balanced in terms of the amount of proteins, fats and carbohydrates and have the maximum set of vitamins.
Optimal for chronic pyelonephritis is considered a vegetable-milk diet with the addition of meat and fish dishes.
It is necessary to include a variety of vegetables in the daily diet: potatoes, zucchini, beets, cabbage, as well as various fruits. Eggs, dairy products and milk itself must be present on the table.
With iron deficiency, you need to eat more apples, strawberries, pomegranates. At any stage of chronic pyelonephritis, the diet should be enriched with watermelons, melons, cucumbers, pumpkin. These products have a diuretic effect and allow you to quickly cope with the disease.
Prevention of chronic pyelonephritis
Prevention of patients with pyelonephritis is reduced to the timely and thorough treatment of patients at the stage of acute pyelonephritis. Such patients should be registered in the dispensary.
There are recommendations for the employment of patients with chronic pyelonephritis: patients are not recommended to work in enterprises that require hard physical labor, contributing to being in constant nervous tension. It is important to avoid hypothermia in the workplace and outside it, you should avoid working on your feet and at night, work in hot shops is excluded.
You should follow a diet with salt restriction as recommended by doctors.
The success of preventive measures in secondary pyelonephritis depends on the complete elimination of the cause that led to the development of the disease. It is important to remove any obstacles to the normal outflow of urine without fail.
It is important to identify and treat hidden foci of infection and intercurrent diseases.
After discharge from the hospital, patients must be registered with a dispensary for a period of at least one year. If after this time bacteriuria, leukocyturia and proteinuria are not detected, then the patient is removed from the register. If signs of the disease persist, then the follow-up period for such patients should be extended to three years.
If primary pyelonephritis is detected in patients, then the treatment is long-term, with periodic placement in a hospital.
No less important is the correction of immunity and maintaining it in good condition. For this, it is necessary to maintain a healthy lifestyle, a long stay in the fresh air, dosed physical activity according to the doctor’s indications.
Staying in sanatorium-resort institutions of a specialized profile allows you to reduce the number of exacerbations of the disease.
Special attention deserves the prevention of the disease in pregnant women and children, as well as in patients with weakened immune systems.
With a latent course of the disease, patients do not lose their ability to work for a long time. Other forms of pyelonephritis can have a significant impact on a person’s performance, as there is a threat of rapid complications.









