Contents
Chronic prostatitis is a serious problem even for modern urology, as many questions regarding this disease still remain unanswered. There is an opinion that chronic prostatitis is a pathology that implies that a person has a whole range of health problems, including tissue damage, functional disorders of the work of not only the prostate gland and urinary tract, but also other male organ systems.
Since there is no single characteristic of the concept of “chronic prostatitis”, this negatively affects the diagnosis and treatment of the disease as a whole.
In order to make this diagnosis, a man must have pain in the perineum, in the pelvic area and in the organs of the genitourinary system for at least 3 months (USA, National Institutes of Health). Signs such as urination disorder and detection of bacteria in secret are not prerequisites for making a diagnosis.
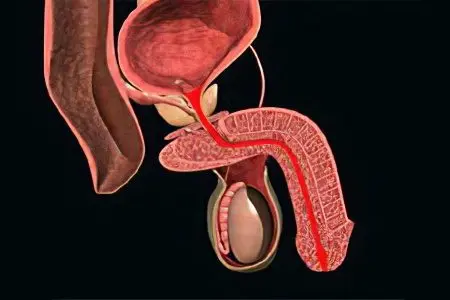
In this case, the process of inflammation in the tissues of the prostate gland must be confirmed by the data of histological studies of prostate tissues, or by microbiological analysis of the secret. Ultrasound examination allows you to clarify the nature of changes in the organ.
Epidemiology of chronic prostatitis
Statistics indicate that the disease is extremely common and is in first place among all diseases of the male reproductive system of an inflammatory nature. In addition, this pathology holds a leading position among all diseases that affect young men in general. We are talking about the representatives of the stronger sex up to 50 years. The average age of patients is 43 years, while 30% of men will definitely suffer this pathology until they reach the age of 80.
Up to 35% of all visits to a urologist in the Russian Federation are due to chronic prostatitis. Often the disease occurs with complications – it can be vesiculitis, dysuria, erectile dysfunction, inability to conceive a child, epididymitis. These and other complications occur according to various data in 7-36% of cases.
Causes of chronic prostatitis

The causes of chronic prostatitis are varied. The disease occurs under the influence of infectious agents, while patients have neurovegetative, hemodynamic, immunological, hormonal disorders. It affects the reflux of urine into the prostate lobes, biochemical factors (disturbance of metabolic processes, and in particular salt metabolism), as well as disturbances in the functioning of growth factors responsible for the proliferation of living cells.
Experts identify the following provocateur factors that influence the formation of the disease:
Infections of the genitourinary system (non-compliance with the rules of personal hygiene, lack of a permanent sexual partner, failure to protect, the presence of an infection in a partner);
Surgical interventions on the prostate without prior preparation with antibacterial agents;
Dysrhythmia of sexual life;
Regular hypothermia;
Bladder catheterization on an ongoing basis;
Hypodynamia.
The role of immunological disorders in the development of the disease should not be rejected. If there is an imbalance of immunocompetent factors, namely cytokines, then this directly affects the work of immunity.
Intraprostatic reflux of urine contributes to the development of chronic non-bacterial prostatitis.
Chronic abacterial prostatitis is associated with neurogenic disorders of the pelvic floor muscles, as well as those elements that are responsible for the functioning of the bladder wall, prostate and urethra.
Pelvic pain syndrome may be due to the fact that a man forms myofascial trigger points, which are located next to the prostate gland and the organs of the genitourinary system. Points that are the result of injuries, surgical interventions and some diseases can lead to pain in the perineum, pubis and nearby areas.
Symptoms of chronic prostatitis
The symptoms of chronic prostatitis are diverse, but the pain and discomfort that occurs in the pelvic area and lasts at least 3 months come to the fore.
In addition, men suffer from erectile dysfunction and urination disorders:
As for pain, they occur mainly in close proximity to the prostate gland, that is, in the perineum, but can radiate to the anus, to the inner surface of the thigh, scrotum, lower back, sacrum and inguinal zone. When pain occurs on one side and radiates to the testicle, most likely this is not a symptom of chronic prostatitis.
Libido suffers, erection does not occur at the moment when there are adequate conditions for this, but although certain sexual disorders are present, complete impotence is not observed.
Another symptom of chronic prostatitis is premature ejaculation. This is typical for the initial stages of the development of the disease. As the pathology progresses, ejaculation becomes, on the contrary, slow. Orgasm is often dim, devoid of richness and emotional color. The ejaculate loses its qualitative and quantitative characteristics.
The disease is characterized by irritative symptoms (increased urination at night, urgency, pain and burning sensation during bladder emptying, urinary incontinence). Ifravesical obstruction with bladder occlusion is less common.
The disease has an undulating course, the symptoms either weaken or become stronger, but they clearly indicate the presence of inflammation.
The following stages of development of chronic prostatitis can be distinguished:
exudative stage. A man experiences pain in the scrotum, in the groin, in the pubis. Urination becomes more frequent, there may be a feeling of discomfort at the end of intercourse. Erections can hurt.
alternative stage. The pains intensify, are localized mainly in the pubic region, in the groin and are given to the sacrum. Emptying the bladder most often goes without any difficulty, although it may occur more often than usual. Erection does not suffer.
proliferative stage. The stream of urine loses its strength, during an exacerbation of the disease, urination becomes more frequent. The erection is intense, but some slowing down of the reaction is possible.
Scar stage. Prostate tissue sclerosis occurs. In the pubic area, in the sacrum there is a feeling of heaviness. Urination becomes more frequent, the urge disturbs the man not only during the day, but also at night. Ejaculation may be completely absent, erection becomes weak.
One should not expect that the symptoms characteristic of a particular stage will be present in a strictly defined order and will arise in full. They may vary depending on the characteristics of the individual course of the disease. But pain, increased urination and functional erectile dysfunction will gradually increase.
At the same time, many men underestimate the severity of the disease until they encounter it. Meanwhile, studies show that the quality of life of people with this problem suffers no less than if they would have suffered angina pectoris, Crohn’s disease, or myocardial infarction.
Classification of chronic prostatitis

The classification of prostatitis was proposed in 1995 in the United States, developed by scientists from the National Institutes of Health:
Acute bacterial prostatitis – type 1 (5% of all diagnosed inflammation of the prostate gland).
Chronic bacterial prostatitis – type 2.
Abacterial prostatitis of chronic course – type 3. This prostatitis is also called chronic pelvic pain syndrome.
Inflammatory form (with a leukocyte jump in the discharge from the prostate) of chronic prostatitis – type 3A. Diagnosed among the total mass of chronic prostatitis in 60% of cases.
Non-inflammatory form (without leukocyte surge) of chronic prostatitis – type 3B. Diagnosed among the total mass of chronic prostatitis in 30% of cases.
Asymptomatic prostatitis – type 4.
Diagnosis of chronic prostatitis
Diagnosis of chronic prostatitis is not particularly difficult when there is a complex of symptoms (pain, urination disorders, sexual disorders). However, it happens that the pathology is asymptomatic, which requires additional research methods, in addition to the standard survey and examination of the patient. These are physical, laboratory, and instrumental methods. Be sure to study the immunological status of the patient, a neurological examination.
In addition, questionnaires and questionnaires have been developed that allow you to clarify the subjective feelings of the patient, give more complete information about the state of his health, about the strength of pain, about urinary disorders, erection, ejaculation, about the patient’s psycho-emotional moods.
Often practicing urologists use the prostatitis symptom scale questionnaire developed by the American National Institutes of Health – this is the NIH-CPS questionnaire.
Laboratory diagnosis of chronic prostatitis
Laboratory diagnosis of chronic prostatitis allows you to distinguish between abacterial and bacterial forms of the disease, determine the type of pathogen and make the most accurate diagnosis. When the fourth urine sample, or prostate secretion, contains more than 10 leukocytes in the PZ, or bacterial associations, chronic inflammation of the prostate is confirmed in this case. If the number of leukocytes is increased, but the bacteria are not sown, the material should be examined for the detection of chlamydia and other STD pathogens in it.
Discharge from the urethra is sent to the laboratory to detect leukocytes, bacterial, fungal or viral flora, as well as mucus in it.
A scraping taken from the urethra is studied by PCR, which makes it possible to identify pathological sexually transmitted agents.
The secret of the prostate is sent for microscopic examination to count the number of leukocytes, macrophages, amyloid and Trousseau-Lallemand bodies. They also conduct its bacteriological study and immunological study, determine the level of nonspecific antibodies.
10 days after the digital rectal examination, blood is taken to determine the concentration of PSA in it. If the indicator exceeds 4,0 ng / ml, then the patient is recommended to undergo a prostate biopsy to exclude cancer.
Based on the results of the performed studies, a diagnosis is made.
Instrumental diagnosis of chronic prostatitis
Transrectal ultrasound examination of the gland makes it possible to clarify the form of the disease, its stage. With the help of ultrasound, it is possible to weed out other diagnoses, track the effectiveness of the therapy, visualize the size of the prostate, its echostructure (exclude the presence of cysts, stones, sclerotic changes, abscess), the density and uniformity of the seminal vesicles.
Urodynamic studies and myography of the pelvic floor muscles reveal neurogenic disorders and infravesical obstruction, which often accompanies chronic prostatitis.
Tomography, both computed and magnetic resonance, is used to make a differential diagnosis, in particular, with prostate cancer. In addition, these methods make it possible to identify existing disorders in the spinal column, in the pelvic organs.
Differential diagnosis of chronic prostatitis
Differential diagnosis of chronic prostatitis is of no small importance, since there is a risk that a man has a more serious disease.
So, the differential diagnosis is established with diseases such as:
Bladder dysfunction of neurogenic origin, complex regional pain syndrome, functional disorder of the detrusor-sphincter system, pseudodyssynergia;
Prostate adenoma, hypertrophic changes in the neck of the bladder, bladder stricture;
Cystitis (interstitial), osteitis of the pubic joint;
Pathologies of the rectum.
To summarize the above, we can give brief answers to frequently asked questions:
What needs to be examined? It is necessary to examine the prostate gland.
How to investigate? Passage of ultrasound examination. Perhaps the appointment of a biopsy of the prostate.
What tests are needed? Analysis of prostate secretion, detection of prostatic antigen in the blood.
Which doctor to contact? Urologist or andrologist.
Treatment of chronic prostatitis
Treatment of chronic prostatitis is the responsibility of the urologist (andrologist). The approach to therapy should be complex, it is necessary to consistently solve the problems facing the patient and the doctor.
The way of life of a man, his habits, peculiarities of thinking are subject to correction. It is important to get rid of addiction to alcohol, move more, play sports, normalize sex life, eat right. Naturally, it will not be possible to do without a course of basic therapy, taking medications is a prerequisite for complete recovery.
[Video] Dr. Evdokimenko “treatment of prostatitis is simple. Is it possible to cure prostatitis forever?:









