Contents
What is chorioretinal dystrophy?
Chorioretinal dystrophy (CHRD) is a dystrophy of the central part of the retina. Synonyms: central disciform dystrophy, senile macular degeneration. This is an age-related pathology that occurs at the age of 50-60 years and is more often observed in women.
With age-related retinal degeneration, gradual irreversible changes occur in the macular (central) zone of the retina, the consequence of which is a significant loss of central vision. The retinal tissue is replaced by fibrous tissue with scarring. Usually this process develops in parallel in both eyes, but in some cases it can occur ahead of time in one eye.
Even in severe cases, CRRD does not lead to complete blindness, as peripheral vision is maintained within the normal range. However, at the same time, the ability to perform work that requires a clear vision (reading, writing, driving, etc.) is completely lost.
The disease has a chronic, slowly progressive course. It should be differentiated from retinal detachment – these are different pathologies.
Causes of chorioretinal dystrophy
The causes and etiology of CRRD have not been fully elucidated.
The list of factors that increase the likelihood of its development includes:
hereditary predisposition;
Weakening of the immune system;
Circulatory disorders in the vascular system of the eyes;
Endocrine pathologies (diabetes mellitus);
Myopia (nearsightedness) of medium and high degree;
Problems with the cardiovascular system (hypertension, atherosclerosis);
Excessive exposure to ultraviolet radiation on the eyes;
Infectious, toxic or traumatic lesions of the eyes;
Irrational nutrition;
Having bad habits.
Chorioretinal dystrophy develops under the influence of a combination of factors. It can be either a congenital disease with an autosomal dominant type of transmission, or a consequence of an infectious-inflammatory process.
Additional risk factors include:
Female;
Light pigmentation of the skin and iris of the eyes;
Smoking abuse;
Operative treatment of a cataract in the anamnesis.
Symptoms of chorioretinal dystrophy

There are two forms of CCRD: non-exudative (dry, atrophic) and exudative (wet).
Dry non-exudative dystrophy is an early form of the disease and occurs in 85-90% of cases. It is characterized by metabolic disorders between the vessels and the retina. Colloidal substances (decay products) accumulate between the basal layer formed by the vascular and retinal membranes and the retinal pigment epithelium, redistribution of the pigment and atrophy of the pigment epithelium occur.
The disease begins asymptomatically and progresses slowly. Visual acuity remains normal for a long time, but there may be a curvature of straight lines, bifurcation, distortion of the shapes and sizes of objects. Gradually, blurring of the image appears when looking directly (as through a layer of water), visual acuity begins to decrease. This process may stabilize at some stage, but may also lead to a complete loss of central vision.
In the second eye, the disease begins to develop no later than five years after the defeat of the first. In 10% of cases, dry dystrophy turns into a more severe wet form. When this occurs, the penetration of fluid (blood) through the walls of the newly formed vessels and its accumulation under the retina.
Exudative dystrophy has four stages of development:
Detachment of the pigment epithelium. Visual acuity is preserved, weak manifestations of farsightedness or astigmatism, the appearance of fog or cloudy spots before the eyes are possible. The process may have a reverse development (adjacency of places of detachment).
Detachment of the neuroepithelium. To the above symptoms, a significant decrease in vision is added, up to the loss of the ability to read and write. Fuzziness of the boundaries and edema of the detachment zone, pathological proliferation of blood vessels are noted.
Hemorrhagic detachment of the pigment and neuroepithelium. Vision remains low. A large pink-brown focus of pigment accumulation with clear boundaries is formed. The cystic retina protrudes into the vitreous body. With rupture of newly formed vessels, hemorrhages occur.
Scar stage. At the site of the lesion, fibrous tissue is formed and a scar is formed.
Diagnosis of chorioretinal dystrophy
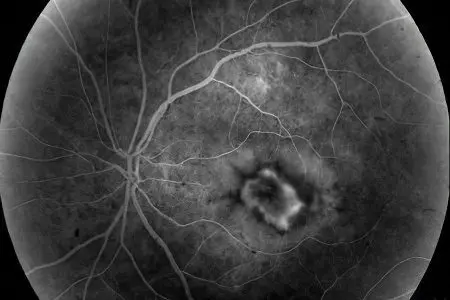
The diagnosis is established on the basis of a patient questioning, visual acuity testing, ophthalmoscopy, campimetry and the Amsler test (studies of the central visual field).
Of the instrumental diagnostic methods used:
Computer perimetry;
Laser scanning tomography of the retina;
Electroretinography;
Fluorescent angiography of the fundus.
Treatment of chorioretinal dystrophy

The choice of treatment tactics depends on the form and stage of the process. The main goal is its stabilization and compensation. Methods of treatment: medical, laser, surgical.
In the non-exudative form, intravenous injections of antiplatelet agents, anticoagulants and angioprotectors, vasodilators (Cavinton), antioxidants (Emoxipin), vitamin therapy are prescribed. Treatment should be continuous and take courses 2 times a year (in autumn and spring).
With the exudative form, general and local treatment is carried out, laser coagulation (cauterization) of the retina is possible in order to eliminate edema and destroy the neovascular (formed from pathological vessels) membrane. This allows you to stop the further development of the dystrophic process.
Surgical treatment is used to improve the blood supply to the back of the eye. This can be vitrectomy (removal of part of the vitreous body), vasoreconstruction, revascularization (restoration of a normal network of microvessels).
The prognosis is generally unfavorable, since it is impossible to restore vision. But even with a complete loss of central vision, peripheral vision remains, sufficient for self-service in everyday life and orientation in space.
Author of the article: Degtyareva Marina Vitalievna, ophthalmologist, ophthalmologist









