Contents
What is a bone fracture?
Fracture – the destruction of the bone with the subsequent separation of parts. It can be caused by a blow or various edema or inflammation.
There are several complications that can occur after fractures:
as soon as the bone is destroyed, its fragments can damage soft tissues, which will lead to additional injuries and bleeding;
paralysis may occur due to damage to nerve cells by bone fragments or the bone itself;
with open fractures, the risk of infection with subsequent purulent inflammation increases;
a fracture can lead to injury to vital organs, such as the brain, if the skull is injured or fractured, or the lungs, heart, etc., if the ribs are broken.
Causes of fractures
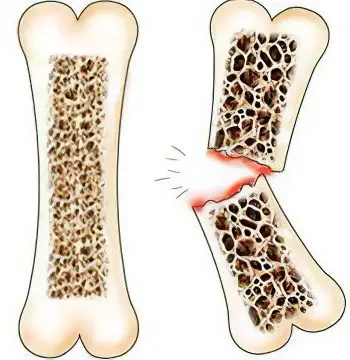
Fractures can be divided into two large groups. The cause of fractures of the first group is the impact on the bone of various forces: a fall, a blow, and more. The cause of fractures of the second group is the weakening of the bone itself and its fragility.
In the second type, the risk of fracture increases several times. It even comes to the point that when walking a person can also break his leg. Here the reason is that this is the pathology of the bone itself, and not the impact on it from the outside. Often this is affected by various diseases, such as osteoporosis and various tissue tumors. If you suffer from osteoporosis, then, as mentioned above, it may be enough for you to just stand up – and your bone may break. Hip fractures are very common in older people. As for open fractures, they most often occur in the lower leg, that is, the legs, and also happen on the hands, where the skin layer is thin. If you fall from a height, then most likely there will be a fracture of the spine or chest, that is, the ribs.
Types of fractures
There are two types of fractures: traumatic and pathological fractures:
Traumatic fractures appear due to the fact that a short but rather powerful force acts on the bone.
pathological fractures – this is the action of various diseases that affect the bone, destroying it. The fracture in this case happens by chance, you don’t even notice it.
There are also open and closed fractures:
Closed fractures are usually not visible, and deformation of the skin due to splinters does not occur.
As for open fractures, the opposite is true. As soon as an open fracture occurs, an infection immediately enters the wound, which can subsequently spread throughout the body. Gunshot-type fractures are very rare for the common people, but such ones also exist.
Also, fractures can be divided by how many parts the bone has broken or whether it has shifted (fracture with and without displacement)
Fractures can be subdivided according to the shape of the fracture, based on the direction of the fracture line into:
Transverse
V-shaped
Helical
Skew
Longitudinal
T-shaped
There may also be fractures by bone types:
Broken arm
Fracture of the radius
Broken leg
Tailbone fracture
Clavicle fracture
Fracture of the lower leg
Humerus fracture
Jaw fracture
Broken nose
Fracture of the foot
pelvic fracture
Fracture of the tibia
Fracture healing phases
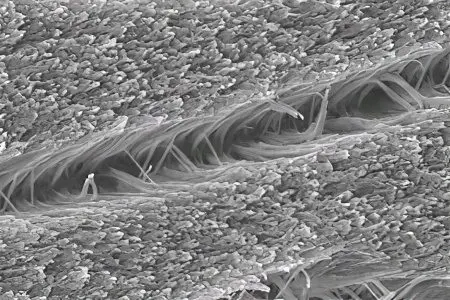
After a fracture, the damaged bones in most people grow together in a chondroblastic pattern. Chondroblasts are the youngest and most active cartilage cells. They have a flattened shape, located inside the perichondrium and throughout the entire thickness of the cartilaginous tissue. At the stage of growth and fusion of bones in chondroblasts, the process of mitotic division and fermentation takes place. In other words, a person owes the ability to grow the skeleton and restore it after injuries to chondroblasts.
At the site of the fracture, a cartilaginous bone callus is formed. This process continues for several months and includes four main phases.
The first phase is catabolic (7-10 days):
In the soft tissues surrounding the fracture site, aseptic (that is, without the participation of microbes) inflammation develops;
There are extensive hemorrhages;
Blood circulation in the tissues around the fracture is disturbed as a result of stagnation of blood;
Toxic products of aseptic inflammation are thrown into the bloodstream and spread throughout the body, which explains the general poor health of the patient (fever, weakness, chills, nausea);
Enzymatic cellular activity increases around the fracture site;
On the surface of the fracture of the bones, necrotic processes occur (microscopic ulcerations and areas of death appear);
There are no signs of fusion of broken bones yet.
The second phase is differential (7-14 days):
The process of formation of fibrous-cartilaginous callus is started (new cells are actively produced at the fracture site: chondroblasts, fibroblasts, osteoblasts, osteoclasts and chondrocytes);
In these cells, the biosynthesis of glycosaminoglycans (polymeric carbohydrate molecules) occurs, the main of which is chondroitin sulfate, which is contained in young cartilage tissue up to two-thirds. Chondroitin sulfate is a substance whose carbohydrate chains are 90% identical to the monosaccharides galactosamine and glucosamine;
Gradually, the basis of the future bone callus, the metrics, is formed. Collagen fibers are actively produced in the cells around the fracture site. At this stage, the callus is still fibrocartilaginous, that is, there are no channels of blood supply vessels in it. It feeds on fluid from the extravascular space, which is almost ten times more than in the intravascular space. Due to this difference, the process of osmosis occurs – one-way diffusion of liquid through cell membranes towards a higher concentration.
The third phase is primary accumulative (2-6 weeks):
From the surrounding tissues, small capillaries gradually grow into the fibrous-cartilaginous callus, which form the vascular network of the future callus;
Chondroitin sulfate molecules located in the mitochondria of cartilage cells combine with phosphate and calcium ions;
The regulating enzyme citrate synthetase and the main energy carrier in cells – adenosine triphosphate (ATP) help the active synthesis of calcium phosphate. Then the chondroitin sulfate molecules combine with calcium phosphate, go into the extracellular space and already there they react with collagen;
During this period, the concentration of silicon and magnesium ions also greatly increases in the cartilage tissue. With the participation of these elements from calcium phosphate and collagen, primary callus is formed at the fracture site. While it is still very weakly mineralized, it does not have an ordered crystal structure and therefore is not strong enough.
The fourth phase is mineralization (2-4 months):
In the extracellular space of the primary callus, a molecular complex is formed from chondroitin sulfate and calcium collagen pyrophosphate;
These molecules react with phospholipids resulting in crystalline hydroxyapatite;
Hydroxyapatite crystals, in turn, settle around the collagen fibers in a special way – so that their axes are located at an angle of 41 degrees relative to each other;
From this tandem, the first callus crystallization nuclei are obtained. Moreover, they can increase in size, feeding on inorganic ions from the fluid of the surrounding soft tissues. This process is called primary bone mineralization;
Then secondary mineralization occurs – intercrystalline bonds are formed around the nuclei. At the end of this stage, we can talk about the complete completion of the healing of the fracture.
Features of the phase flow
Above are averaged data on the course and duration of each phase of bone fusion. The calculations are made based on the fact that we have a relatively healthy patient, and the injury does not differ in increased complexity.
But fractures are different, and the speed of recovery directly depends on many factors:
Type of fracture (open or closed, multiple or single, on one bone or on several);
The age of the patient (in the elderly, bone fusion can last more than six months, and in adolescents it can be completed in a month);
General health (bone mineralization, blood quality, muscle tone);
The presence or absence of aggravating factors (comorbidities and injuries) – the more damage to bones, organs and soft tissues received by the patient as a result of an injury, the longer the rehabilitation process will continue.
Treatment

With a closed fracture, the patient is sedated with some kind of anesthetic that is injected into the fracture site. The broken place is strengthened, for example, with a splint, so that the bone and its broken honor are in a motionless state. If the fracture is of an open type, then the pain is also relieved and the victim is brought to life, but only so that he is in adequate condition, then the bleeding should be stopped by clamping the wounds. The bone is also fixed in the tire and the victim is immediately taken to the hospital. If the bleeding does not stop, and this occurs with arterial or venous damage, then a tourniquet is applied above the affected area.
Upon arrival at the hospital, the patient will be set the bone, but this will only happen under complete anesthesia or, for example, anesthesia. If the fracture is not visible enough, then the skin is cut a little. The bone is fixed with plaster.
At this point in time, all the treatment of fractures can be divided into two types:
Conservative – with the help of the same gypsum. This is how it was treated in ancient times. Now only minor fractures or cracks in the bones are treated this way;
Prompt – the bone can be reduced or attracted with the help of all kinds of knitting needles, tubes, all kinds of chemical elements are also used.









